Podcast
Questions and Answers
What is the primary function of the renal artery in the kidneys?
What is the primary function of the renal artery in the kidneys?
- Drains blood after filtration
- Supplies oxygen to the kidney tissue
- Connects the kidneys to the bladder
- Carries blood to be filtrated (correct)
Which structure is responsible for draining urine to the bladder?
Which structure is responsible for draining urine to the bladder?
- Renal hilum
- Renal artery
- Renal vein
- Ureter (correct)
What is the approximate weight of each kidney?
What is the approximate weight of each kidney?
- 200 g
- 150 g (correct)
- 250 g
- 100 g
Which of the following best describes the position of the kidneys?
Which of the following best describes the position of the kidneys?
What anatomical feature marks the entry and exit points for renal structures?
What anatomical feature marks the entry and exit points for renal structures?
What is the dimension of a typical kidney in length?
What is the dimension of a typical kidney in length?
Which protective structure is located posteriorly to the kidneys?
Which protective structure is located posteriorly to the kidneys?
How can kidney inflammation be detected?
How can kidney inflammation be detected?
Which organ serves the primary function of producing urine in the urinary system?
Which organ serves the primary function of producing urine in the urinary system?
What is the main nitrogen waste product found in urine?
What is the main nitrogen waste product found in urine?
Which structure conducts urine from the kidneys to the urinary bladder?
Which structure conducts urine from the kidneys to the urinary bladder?
What is the primary function of the urinary bladder?
What is the primary function of the urinary bladder?
Which of the following best describes the role of nephron structures in the kidneys?
Which of the following best describes the role of nephron structures in the kidneys?
The contraction of which muscle drives the process of urination?
The contraction of which muscle drives the process of urination?
Which of the following components is primarily responsible for the toxic buildup in cells during nitrogen metabolism?
Which of the following components is primarily responsible for the toxic buildup in cells during nitrogen metabolism?
How do ureters transport urine to the urinary bladder?
How do ureters transport urine to the urinary bladder?
What is the primary function of the nephron in the kidney?
What is the primary function of the nephron in the kidney?
Which type of nerve fibers primarily innervate the nephrons?
Which type of nerve fibers primarily innervate the nephrons?
How do the kidneys maintain homeostasis concerning blood volume?
How do the kidneys maintain homeostasis concerning blood volume?
What is one of the effects of sympathetic stimuli on the kidneys?
What is one of the effects of sympathetic stimuli on the kidneys?
What are the two types of nephrons found in the kidneys?
What are the two types of nephrons found in the kidneys?
Which structure directly connects to the glomerulus in the nephron?
Which structure directly connects to the glomerulus in the nephron?
What role does renin play in the kidney's response to sympathetic stimuli?
What role does renin play in the kidney's response to sympathetic stimuli?
Which of the following correctly describes a function of the renal circulation patterns?
Which of the following correctly describes a function of the renal circulation patterns?
What is the primary role of the fibrous capsule in kidney protection?
What is the primary role of the fibrous capsule in kidney protection?
Which layer of tissue is primarily responsible for cushioning the kidney?
Which layer of tissue is primarily responsible for cushioning the kidney?
What structure separates adjacent renal pyramids in the kidney?
What structure separates adjacent renal pyramids in the kidney?
How many lobes does each kidney typically contain?
How many lobes does each kidney typically contain?
Which layer is characterized as a dense, fibrous outer layer that anchors the kidney?
Which layer is characterized as a dense, fibrous outer layer that anchors the kidney?
What is the function of perinephric fat in relation to the kidneys?
What is the function of perinephric fat in relation to the kidneys?
Which kidney structure is not directly associated with the kidney's protective layers?
Which kidney structure is not directly associated with the kidney's protective layers?
The renal papilla is associated with which kidney structure?
The renal papilla is associated with which kidney structure?
What process occurs only in the renal corpuscle?
What process occurs only in the renal corpuscle?
During which process are substances like H+ ions added to the tubular fluid?
During which process are substances like H+ ions added to the tubular fluid?
Which nephron segment is primarily responsible for filtration?
Which nephron segment is primarily responsible for filtration?
What dictates the balance between reabsorption and secretion in the nephron?
What dictates the balance between reabsorption and secretion in the nephron?
Where does the final volume of water in tubular fluid largely derive from?
Where does the final volume of water in tubular fluid largely derive from?
What happens to water and solutes during reabsorption?
What happens to water and solutes during reabsorption?
What is the role of the efferent arterioles in the secretion process?
What is the role of the efferent arterioles in the secretion process?
Which of the following components are primarily filtered during the initial filtration process?
Which of the following components are primarily filtered during the initial filtration process?
What effect does abnormal blood pressure have on filtration rate?
What effect does abnormal blood pressure have on filtration rate?
Which component is responsible for central regulation of glomerular filtration rate?
Which component is responsible for central regulation of glomerular filtration rate?
What happens if autoregulation of glomerular filtration rate is ineffective?
What happens if autoregulation of glomerular filtration rate is ineffective?
What role does Renin play in the regulation of blood pressure?
What role does Renin play in the regulation of blood pressure?
How does blood viscosity affect the filtration rate in the nephrons?
How does blood viscosity affect the filtration rate in the nephrons?
Which of the following statements about the filtration rate is true?
Which of the following statements about the filtration rate is true?
What is the primary purpose of autoregulation in the kidneys?
What is the primary purpose of autoregulation in the kidneys?
Which of the following factors does NOT impact the filtration rate?
Which of the following factors does NOT impact the filtration rate?
Flashcards
What are the organs of the urinary system?
What are the organs of the urinary system?
Two kidneys, ureters, urinary bladder, and urethra.
What is the main function of the kidneys in the urinary system?
What is the main function of the kidneys in the urinary system?
The kidneys are the primary organs responsible for producing urine.
What is urea, and why is it important?
What is urea, and why is it important?
Urea is a nitrogen-containing waste product produced by the body during metabolism.
What is the function of the ureters?
What is the function of the ureters?
Signup and view all the flashcards
What is the primary function of the bladder?
What is the primary function of the bladder?
Signup and view all the flashcards
What is the urethra and what is its role?
What is the urethra and what is its role?
Signup and view all the flashcards
What is micturition?
What is micturition?
Signup and view all the flashcards
What is the significance of the high blood flow to the kidneys?
What is the significance of the high blood flow to the kidneys?
Signup and view all the flashcards
Kidneys
Kidneys
Signup and view all the flashcards
Renal Hilum
Renal Hilum
Signup and view all the flashcards
Renal Artery
Renal Artery
Signup and view all the flashcards
Renal Vein
Renal Vein
Signup and view all the flashcards
Ureter
Ureter
Signup and view all the flashcards
Kidney Location
Kidney Location
Signup and view all the flashcards
Kidney Protection
Kidney Protection
Signup and view all the flashcards
Palpation of the Kidneys
Palpation of the Kidneys
Signup and view all the flashcards
What is the fibrous capsule?
What is the fibrous capsule?
Signup and view all the flashcards
What is the perinephric fat?
What is the perinephric fat?
Signup and view all the flashcards
What is the renal fascia?
What is the renal fascia?
Signup and view all the flashcards
What is the renal sinus?
What is the renal sinus?
Signup and view all the flashcards
What is the renal cortex?
What is the renal cortex?
Signup and view all the flashcards
What is the renal medulla?
What is the renal medulla?
Signup and view all the flashcards
What are renal pyramids?
What are renal pyramids?
Signup and view all the flashcards
What is the renal papilla?
What is the renal papilla?
Signup and view all the flashcards
What is a nephron?
What is a nephron?
Signup and view all the flashcards
What is the glomerulus?
What is the glomerulus?
Signup and view all the flashcards
What is the efferent arteriole?
What is the efferent arteriole?
Signup and view all the flashcards
What is the afferent arteriole?
What is the afferent arteriole?
Signup and view all the flashcards
What are peritubular capillaries?
What are peritubular capillaries?
Signup and view all the flashcards
What is the overall function of the kidneys?
What is the overall function of the kidneys?
Signup and view all the flashcards
What is the role of the renal nerves?
What is the role of the renal nerves?
Signup and view all the flashcards
Glomerular Filtration
Glomerular Filtration
Signup and view all the flashcards
Tubular Reabsorption
Tubular Reabsorption
Signup and view all the flashcards
Tubular Secretion
Tubular Secretion
Signup and view all the flashcards
Renal Corpuscle
Renal Corpuscle
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
Urine Formation
Urine Formation
Signup and view all the flashcards
Collecting System Function
Collecting System Function
Signup and view all the flashcards
Reabsorption-Secretion Balance
Reabsorption-Secretion Balance
Signup and view all the flashcards
What affects Glomerular Filtration Rate?
What affects Glomerular Filtration Rate?
Signup and view all the flashcards
How does autoregulation affect GFR?
How does autoregulation affect GFR?
Signup and view all the flashcards
What is central regulation for GFR?
What is central regulation for GFR?
Signup and view all the flashcards
What is the role of Renin in GFR?
What is the role of Renin in GFR?
Signup and view all the flashcards
What is the juxtaglomerular complex (JGC)?
What is the juxtaglomerular complex (JGC)?
Signup and view all the flashcards
What is the RAAS system?
What is the RAAS system?
Signup and view all the flashcards
How does the RAAS system affect blood pressure?
How does the RAAS system affect blood pressure?
Signup and view all the flashcards
How do kidneys maintain blood pressure?
How do kidneys maintain blood pressure?
Signup and view all the flashcards
Study Notes
Urinary System Anatomy
- The urinary system includes the kidneys, ureters, urinary bladder, and urethra.
- Kidneys are paired retroperitoneal organs.
- Kidneys are reddish-brown in color.
- Average kidney dimensions are ~10 cm (4 in.) long, ~5.5 cm (2.2 in.) wide, ~3 cm (1.2 in.) thick.
- Average kidney weight is ~150 g (5.25 oz).
- They are located posterior and superior in the abdominal cavity, between the posterior body wall and parietal peritoneum.
Urinary System Organs Diagrammed and Described
- The diagram shows the position of the kidneys, ureters, bladder, prostate, and urethra in the body.
- The kidneys filter blood to produce urine.
- Ureters transport urine from the kidneys to the bladder.
- The bladder stores urine.
- The urethra carries urine out of the body.
Urinary System Learning Outcomes
- Understand the structures and functions of the urinary system.
- Understand nitrogen waste and urea as the main components of urine.
- Understand the internal structures of the kidneys, with a focus on filtration.
- Understand the structure of nephrons and their roles in water, electrolyte, and glucose regulation.
- Understand the anatomy and physiology of urination (micturition).
- Understand the reflex mechanisms associated with urination.
Urinary System Major Functions
- Adjusting blood volume and pressure.
- Regulating plasma concentrations of sodium, potassium, chloride, and other ions.
- Stabilizing blood pH.
- Conserving nutrients by preventing loss in urine.
- Removing drugs and toxins from the bloodstream.
- Urea is a main nitrogenous waste product created during metabolism.
- Urea is toxic when it builds up in cells.
Kidney Structure (Two Kidneys)
- Reddish brown
- Dimensions: ~10 cm (4 in.) long; ~5.5 cm (2.2 in.) wide; ~3 cm (1.2 in.) thick; Weight: ~150 g (5.25 oz)
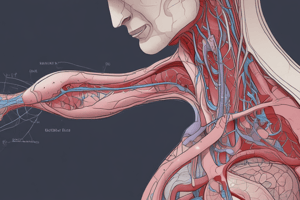
- Renal hilum: medial indentation where renal artery, renal nerves, renal vein, and ureter enter/exit the kidney.
- Renal artery: blood entering for filtration.
- Renal vein: blood leaving after filtration.
- Ureter: drains urine to the bladder.
Kidney Location and Structure
- Located in a retroperitoneal position between the muscles of the posterior body wall and parietal peritoneum.
- Posterior and superior in the abdominal cavity.
- Connected to the urinary bladder by the ureters.
- Empty into the posterior, inferior surface of the urinary bladder.
Kidney Location and Structure (Posterior Location)
- Lateral on either side of the vertebral column.
- Superficial palpation from the back can assess kidney inflammation.
- Protected anteriorly by visceral organs like the liver and stomach.
- Protected posteriorly by body wall musculature and the 11th and 12th ribs.
Tissue Anchoring and Protecting the Kidneys
- Connective tissues protect and connect the kidneys to the peritoneal cavity and adjacent organs.
- Fibrous capsule covers the outer surface.
- Projects collagen fibers through perinephric fat to the renal fascia.
- Adipose tissue surrounds the kidney, cushioning it and supplying biomolecules for energy.
Deep Anatomy of the Kidneys
- Major structural landmarks: fibrous capsule, renal sinus (cavity lining the kidney), renal cortex (superficial cortex of the kidney), renal medulla (deep region of the kidney), renal pyramid (conical structure in the medulla), renal papilla (tip of the pyramid), renal column (separates adjacent pyramids).
- Kidney lobe (pyramid, overlying cortex, and adjacent renal columns); each kidney contains 6-18 lobes.
- Other features: renal hilum (medial indentation), minor calyx, major calyx, renal pelvis (funnel-shaped structure collecting urine from major calyces, continuous with the ureter).
Renal Sinus
- Blood pools in the renal sinus and circulation slows, ensuring maximum filtration.
The Nephron – The Filtration Unit within the Kidney
- Two types of nephrons: cortical nephrons (85% of all nephrons, located primarily in the cortex, responsible for most regulatory functions) and juxtamedullary nephrons (15% of all nephrons, long nephron loop extending deep into the medulla, essential for producing concentrated urine).
The Anatomy of a Nephron
- Two components: renal corpuscle (blood pressure forces water and solutes out of glomerular capillaries into filtrate) and renal tubule (tubular passageway up to 50 mm long that receives filtrate and modifies it to create urine).
Renal Corpuscle and Renal Tubules of the Nephron
- The renal corpuscle generates glomerular filtrate.
- Proximal convoluted tubule: reabsorbs sodium, chloride, potassium, water, glucose, amino acids, bicarbonate, calcium, and phosphate; secretes ammonium and creatinine.
- Loop of Henle (thin descending limb): reabsorbs water.
- Loop of Henle (thin ascending limb): reabsorbs sodium and chloride.
- Loop of Henle (thick ascending limb): reabsorbs ammonium, sodium, and chloride.
- Distal convoluted tubule: reabsorbs sodium and chloride.
- Collecting duct: reabsorbs sodium, chloride, and water; secretes ammonium, hydrogen ions, and potassium.
Nephron - First Interaction or Filtration with Blood Circulation
- Bowman's capsule (cup-shaped chamber) surrounds glomerulus capillaries.
- Blood is initially filtered at the renal corpuscle—water and soluble molecules like urea, electrolytes, and glucose are sent to the tubules.
- Larger components (like cells and large proteins) are not filtered and return to circulation (efferent blood flow), leaving the glomerulus via the efferent arteriole .
Segments of a Nephron - Secondary Filtration of Primary Filtration Through the Nephron Tubule (PCT)
- Beginning of secondary filtration; reabsorbs nutrients from the tubular filtrate (now called tubular fluid).
- Proximal part immediately after the Glomerulus where primary filtration occurs.
- Afferent Blood Flow (blood cells are not filtered)
- Not straight and convoluted
Module 24.4: Segments of a nephron (Loop of Henle)
- Long linear loop of the nephron tubule.
- Establishes an osmotic gradient for water reabsorption.
- Can be adjusted to retain or remove more water to meet the needs from low/high blood pressure or dehydration.
Module 24.4: Segments of a nephron (DCT)
- Adjusts fluid composition through reabsorption and secretion.
- Distal part (distal from the Glomerulus) of the Nephron before to the Collecting Duct.
- The Collecting Duct leads to the Ureter to the Bladder.
Renal Physiology – Continuous Filtration and Reabsorption
- Secondary filtration occurs all through the tubule with water and electrolytes being filtered.
- Water and solutes are reabsorbed. Filtration events include glomerular capillaries and Bowman’s capsule (filtration membrane) with filtrate entering the proximal convoluted tubule of the nephron.
Segments of a nephron – Urine Collection and Final Reabsorption
- Collecting System; series of tubes conveying tubular fluid away from the nephron as part of the final step in water and solute reabsorption before exiting the kidneys via the ureter to the bladder.
- Collecting duct: collects fluid from many nephrons, carries fluid through renal medulla.
- Papillary duct: delivers fluid to a minor calyx.
Segments of a nephron – Urine Collection and Final Reabsorption (Continued)
- Collecting duct lined with intercalated cells (play a role in secreting/reabsorbing hydrogen and bicarbonate ions) and principal cells (reabsorb water and secrete potassium); delivers fluid to minor calyx.
Circulation Patterns in the Kidney
- Blood flow around a cortical nephron starting with the afferent arteriole, then glomerulus and efferent arteriole connecting to peritubular capillaries.
- Cortical radiate veins collect blood from capillaries, draining into arcuate veins then to interlobar veins to the renal vein where it exits the kidney to inferior vena cava.
- Arterial patterns: renal artery → segmental arteries → interlobar arteries → arcuate arteries → cortical radiate arteries. Afferent arterioles deliver blood to the capillaries of each nephron (glomerulus) (site of primary filtration).
Nephron Innervation
- Each kidney has ~1.25 million nephrons.
- Cortical and juxtamedullary nephrons are innervated by renal nerves.
- Entering at the hilum, they follow the renal artery branches.
- Most nerve fibers are sympathetic postganglionic fibers from celiac plexus and inferior splanchnic nerves.
- They adjust blood flow/blood pressure in glomeruli and stimulate renin release.
Renal Function Physiology
- The urinary system maintains homeostasis via adjusting blood volume and composition; concentrating urine by reabsorbing water through the nephron; regulating water and solute reabsorption based on body needs (e.g., dehydration).
- Concentrates urine by reabsorbing water throughout the nephron to the collecting tubule.
- Regulates the amount of water and solute reabsorption back into circulation depending on the body's need (i.e., dehydration).
Renal Physiology – Waste Removal
- Urea; most abundant organic waste via amino acid and nucleotide breakdown.
- Creatinine; byproduct of creatine phosphate breakdown in muscles.
- Uric acid; formed during recycling of nitrogenous bases of RNA (nucleic acids).
Renal Physiology- Basic Steps in Urine Formation
- Three processes: filtration, reabsorption, and secretion.
- Filtration: Blood pressure forces water and solutes across glomerular capillaries to be into the Bowman’s capsule.
- Reabsorption: Water and solutes are transported out of tubular fluid into peritubular fluid for reabsorption through the peritubular capillaries.
- Secretion: Transport of remaining solutes and water from the tubular fluid to the nephron and collecting duct.
- Urine leaves the kidneys via the ureter to the bladder.
Filtration at the Glomerulus – Filtration by Size
- Filtration membrane prevents most plasma proteins/cells from entering the capsular space, remaining in the efferent arteriole.
- Fenestrated glomerular capillaries contain large diameter pores.
- Dense layer with specialized basement membrane which has filtration slits.
Things That Alter Filtration Rate
- Factors controlling glomerular filtration (GHP, BCOP, NFP, CsHP): Blood pressure, blood colloid osmotic pressure, net filtration pressure, and capsular hydrostatic pressure affect filtration.
Assessing Glomerular Filtration Rate
- Two interacting levels (autoregulation: local level, central regulation: endocrine/neural components) regulating GFR. Autoregulation with the nervous/endocrine system help stabilize GFR. The nervous system involves the sympathetic division of the autonomic nervous system(ANS). The endocrine component is regulated through the kidneys.
Autoregulation
- Immediate local response in the kidney that maintains adequate GFR in response to decreased filtration pressure; decreased filtrate, and urine production.
- Adjusting the contraction of intraglomerular mesangial cells for filtration.
- Constriction of efferent arterioles.
- Dilation of afferent arterioles.
- Homeostasis is maintained through decreased or increased blood flow to the kidneys..
Central Regulation – Renin & Juxtaglomerular Complex
- If autoregulation is ineffective, central regulation involves the release of renin by the juxtaglomerular complex; angiotensin II constricts peripheral arterioles and efferent arterioles, elevating blood pressure.
- Aldosterone increases Na+ retention, fluid consumption, thirst, increased antidiuretic hormone (ADH) production, and sympathetic motor tone.
Reabsorption
- Reabsorption in the PCT (proximal convoluted tubule)) includes the reabsorption of over 99% of glucose, amino acids, and other organic nutrients along with sodium, potassium, bicarbonate, magnesium, phosphate, and sulfate ions.
- Solute concentration in tubular fluid decreases/water moves into peritubular fluid along the PCT tubules.
Balance between Reabsorption and Secretion
- Movement of water and solutes from the peritubular fluid into the tubular fluid in the distal convoluted tubule (DCT)
- About 15-20% of initial filtrate reaches the DCT.
- Sodium ions reabsorbed in exchange for potassium ions (stimulated by aldosterone).
- Hydrogen ions are secreted.
- Carrier proteins can secrete toxins or drugs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.