Podcast
Questions and Answers
Which of the following is the MOST common underlying cause of peripheral artery disease (PAD) in the lower limbs?
Which of the following is the MOST common underlying cause of peripheral artery disease (PAD) in the lower limbs?
- Atherosclerosis (correct)
- Thromboangiitis obliterans
- Vasculitis
- Fibromuscular dysplasia
A patient reports experiencing cramping muscle pain in their calf while walking, which is relieved by rest. This symptom is MOST indicative of:
A patient reports experiencing cramping muscle pain in their calf while walking, which is relieved by rest. This symptom is MOST indicative of:
- Thrombophlebitis
- Intermittent claudication (correct)
- Deep vein thrombosis
- Ischemic rest pain
A patient with suspected peripheral artery disease (PAD) reports experiencing leg pain that worsens at night when lying down and improves when sitting or standing. This is MOST consistent with:
A patient with suspected peripheral artery disease (PAD) reports experiencing leg pain that worsens at night when lying down and improves when sitting or standing. This is MOST consistent with:
- Restless leg syndrome
- Superficial thrombophlebitis
- Intermittent claudication
- Ischemic rest pain (correct)
Which of the following findings during a vascular examination is MOST indicative of advanced ischemia?
Which of the following findings during a vascular examination is MOST indicative of advanced ischemia?
A patient presents with the classic triad of high gluteal claudication and impotence. This presentation is MOST suggestive of which vascular condition?
A patient presents with the classic triad of high gluteal claudication and impotence. This presentation is MOST suggestive of which vascular condition?
A patient undergoing evaluation for upper limb ischemia is found to have dizziness, fainting, and visual disturbances, particularly with arm exercise. Which of the following conditions is MOST likely?
A patient undergoing evaluation for upper limb ischemia is found to have dizziness, fainting, and visual disturbances, particularly with arm exercise. Which of the following conditions is MOST likely?
During inspection of a patient's lower extremities, you observe that the affected limb is paler and colder than the unaffected limb. After the patient hangs their leg down, it becomes red. This color change is MOST indicative of:
During inspection of a patient's lower extremities, you observe that the affected limb is paler and colder than the unaffected limb. After the patient hangs their leg down, it becomes red. This color change is MOST indicative of:
Which of the following is a key characteristic of ulcers caused by arterial insufficiency?
Which of the following is a key characteristic of ulcers caused by arterial insufficiency?
A patient presents with sudden pain, pallor, pulselessness, and paresthesia in their left leg. These findings are MOST consistent with:
A patient presents with sudden pain, pallor, pulselessness, and paresthesia in their left leg. These findings are MOST consistent with:
During palpation of arterial pulses, a medical professional detects a vibration or buzzing sensation. This finding is BEST described as:
During palpation of arterial pulses, a medical professional detects a vibration or buzzing sensation. This finding is BEST described as:
When palpating the popliteal artery, which technique is MOST appropriate for accurate assessment?
When palpating the popliteal artery, which technique is MOST appropriate for accurate assessment?
A physician is attempting to palpate the dorsalis pedis artery. Where should they MOST accurately locate this pulse?
A physician is attempting to palpate the dorsalis pedis artery. Where should they MOST accurately locate this pulse?
During auscultation of a patient's abdomen, a physician hears a bruit. This finding suggests:
During auscultation of a patient's abdomen, a physician hears a bruit. This finding suggests:
While performing auscultation for vascular sounds, which location would be MOST appropriate to listen for a potential renal artery stenosis?
While performing auscultation for vascular sounds, which location would be MOST appropriate to listen for a potential renal artery stenosis?
A physician performs Allen's test on a patient. After releasing pressure on the ulnar artery, the hand does not flush within 3-5 seconds. What does this indicate?
A physician performs Allen's test on a patient. After releasing pressure on the ulnar artery, the hand does not flush within 3-5 seconds. What does this indicate?
During Ratschow's exercise test for suspected PAD, a patient performs plantar and dorsal flexion, and after hanging their feet down, the time to first redness on both legs is 8 seconds. According to the guidelines, this result would be:
During Ratschow's exercise test for suspected PAD, a patient performs plantar and dorsal flexion, and after hanging their feet down, the time to first redness on both legs is 8 seconds. According to the guidelines, this result would be:
Which of the following ankle-brachial index (ABI) values is indicative of moderate to severe peripheral arterial disease?
Which of the following ankle-brachial index (ABI) values is indicative of moderate to severe peripheral arterial disease?
When measuring the Ankle-Brachial Index (ABI), a medical assistant obtains blood pressure readings in both arms and both ankles. Which of the following protocols is MOST accurate?
When measuring the Ankle-Brachial Index (ABI), a medical assistant obtains blood pressure readings in both arms and both ankles. Which of the following protocols is MOST accurate?
Compared to angiography(AG), which imaging method is LEAST invasive for vascular examination?
Compared to angiography(AG), which imaging method is LEAST invasive for vascular examination?
Acral cyanosis, migratory phlebitis, and sensitivity to cold are MOST characteristic of which of the following conditions?
Acral cyanosis, migratory phlebitis, and sensitivity to cold are MOST characteristic of which of the following conditions?
Which of the following maneuvers is used to assess for compression of the neurovascular bundle in thoracic outlet syndrome (TOS)?
Which of the following maneuvers is used to assess for compression of the neurovascular bundle in thoracic outlet syndrome (TOS)?
In performing Adson's test, what indicates a positive result suggestive of thoracic outlet syndrome?
In performing Adson's test, what indicates a positive result suggestive of thoracic outlet syndrome?
A patient presents with episodes of sharply demarcated whitening and cooling of the fingers, followed by cyanosis and redness. These color changes are MOST suggestive of:
A patient presents with episodes of sharply demarcated whitening and cooling of the fingers, followed by cyanosis and redness. These color changes are MOST suggestive of:
During a vascular examination, which of the following best describes the typical flow pattern of the great saphenous vein (GSV)?
During a vascular examination, which of the following best describes the typical flow pattern of the great saphenous vein (GSV)?
A patient reports chronic leg swelling, discomfort, and skin changes around the ankles. These symptoms are MOST suggestive of:
A patient reports chronic leg swelling, discomfort, and skin changes around the ankles. These symptoms are MOST suggestive of:
Which of the following activities is a significant risk factor for the development of varicose veins and chronic venous insufficiency?
Which of the following activities is a significant risk factor for the development of varicose veins and chronic venous insufficiency?
A patient with chronic venous insufficiency reports that their symptoms are MORE pronounced in the evening, especially after prolonged standing. What is the MOST likely reason for this?
A patient with chronic venous insufficiency reports that their symptoms are MORE pronounced in the evening, especially after prolonged standing. What is the MOST likely reason for this?
During a physical examination of a patient with suspected chronic venous insufficiency, a healthcare provider observes small, dilated intradermal venules less than 1 mm in diameter. These are BEST described as:
During a physical examination of a patient with suspected chronic venous insufficiency, a healthcare provider observes small, dilated intradermal venules less than 1 mm in diameter. These are BEST described as:
Which of the following physical findings is MOST characteristic of lipodermatosclerosis in chronic venous insufficiency?
Which of the following physical findings is MOST characteristic of lipodermatosclerosis in chronic venous insufficiency?
A patient presents with unilateral leg swelling, pain, and tenderness along the course of a superficial vein. These findings are MOST suggestive of:
A patient presents with unilateral leg swelling, pain, and tenderness along the course of a superficial vein. These findings are MOST suggestive of:
A D-dimer test is ordered for a patient with suspected deep vein thrombosis (DVT). A negative D-dimer result is MOST useful for:
A D-dimer test is ordered for a patient with suspected deep vein thrombosis (DVT). A negative D-dimer result is MOST useful for:
In the diagnosis of DVT, venous ultrasonography reveals a vein that is dilated, noncompressible, and without blood flow. These findings are indicative of:
In the diagnosis of DVT, venous ultrasonography reveals a vein that is dilated, noncompressible, and without blood flow. These findings are indicative of:
A patient presents with edema of the neck and upper part of the chest and colaterals. Which of the following conditions is MOST likely to be the primary cause?
A patient presents with edema of the neck and upper part of the chest and colaterals. Which of the following conditions is MOST likely to be the primary cause?
A patient presents with pain and swelling in the arm following multiple attempts at intravenous catheter placement. Which of the following conditions is MOST likely?
A patient presents with pain and swelling in the arm following multiple attempts at intravenous catheter placement. Which of the following conditions is MOST likely?
A patient presents with recurrent episodes of inflammation in various segments of the superficial venous system without an apparent local cause. This is MOST suggestive of:
A patient presents with recurrent episodes of inflammation in various segments of the superficial venous system without an apparent local cause. This is MOST suggestive of:
The lymphatic vessels of the upper extremities drain primarily into which of the following lymph node groups?
The lymphatic vessels of the upper extremities drain primarily into which of the following lymph node groups?
Unlike lymphedema, which of the following physical characteristics is MOST likely associated with lipedema?
Unlike lymphedema, which of the following physical characteristics is MOST likely associated with lipedema?
A patient presents with chronic lower extremity swelling. On physical examination, the skin is thickened and rigid, and there is an inability to lift or pinch a skinfold at the base of the second toe. This finding is known as:
A patient presents with chronic lower extremity swelling. On physical examination, the skin is thickened and rigid, and there is an inability to lift or pinch a skinfold at the base of the second toe. This finding is known as:
Which imaging finding is MOST suggestive of lymphedema?
Which imaging finding is MOST suggestive of lymphedema?
A patient presents with lower limb pain exacerbated by walking, relieved with rest, and a history of smoking. Which of the following is the MOST likely underlying mechanism?
A patient presents with lower limb pain exacerbated by walking, relieved with rest, and a history of smoking. Which of the following is the MOST likely underlying mechanism?
A patient with confirmed peripheral artery disease (PAD) reports experiencing constant foot pain that is worse at night and relieved by dangling their foot off the bed. This symptom is MOST likely due to:
A patient with confirmed peripheral artery disease (PAD) reports experiencing constant foot pain that is worse at night and relieved by dangling their foot off the bed. This symptom is MOST likely due to:
Which of the following findings from a lower extremity examination is MOST concerning for advanced peripheral artery disease (PAD)?
Which of the following findings from a lower extremity examination is MOST concerning for advanced peripheral artery disease (PAD)?
A 62-year-old male presents with a history of smoking, hypertension, and diabetes. He reports pain in his buttocks and thighs when walking short distances, as well as impotence. This clinical picture is MOST suggestive of:
A 62-year-old male presents with a history of smoking, hypertension, and diabetes. He reports pain in his buttocks and thighs when walking short distances, as well as impotence. This clinical picture is MOST suggestive of:
A young athlete complains of dizziness and visual disturbances specifically when exercising the right arm. Auscultation reveals a subclavian bruit. Which condition is MOST likely?
A young athlete complains of dizziness and visual disturbances specifically when exercising the right arm. Auscultation reveals a subclavian bruit. Which condition is MOST likely?
A patient's lower extremity is pale and cool. Upon dependent positioning, the limb turns red. What is the MOST likely cause of these color changes?
A patient's lower extremity is pale and cool. Upon dependent positioning, the limb turns red. What is the MOST likely cause of these color changes?
A patient exhibits a painful, deep ulcer on their toe with a 'punched-out' appearance. The surrounding skin is cool and hairless. Which etiology is MOST likely?
A patient exhibits a painful, deep ulcer on their toe with a 'punched-out' appearance. The surrounding skin is cool and hairless. Which etiology is MOST likely?
A patient comes to the emergency room with acute onset of severe pain, pallor, pulselessness, and paresthesia in the left lower extremity. What is the MOST appropriate initial diagnostic step?
A patient comes to the emergency room with acute onset of severe pain, pallor, pulselessness, and paresthesia in the left lower extremity. What is the MOST appropriate initial diagnostic step?
During palpation of the femoral artery, a medical student notes a palpable rhythmic vibration. The attending physician explains that this finding is BEST described as:
During palpation of the femoral artery, a medical student notes a palpable rhythmic vibration. The attending physician explains that this finding is BEST described as:
What is the BEST technique for palpating the popliteal artery?
What is the BEST technique for palpating the popliteal artery?
To accurately palpate the dorsalis pedis artery, you should palpate:
To accurately palpate the dorsalis pedis artery, you should palpate:
Which of the following MOST accurately describes the significance of hearing a bruit during abdominal auscultation?
Which of the following MOST accurately describes the significance of hearing a bruit during abdominal auscultation?
A physician suspects renal artery stenosis in a hypertensive patient. Where should the physician auscultate to BEST assess for this condition?
A physician suspects renal artery stenosis in a hypertensive patient. Where should the physician auscultate to BEST assess for this condition?
Following performance of the Allen test, the hand flushes within 2 seconds after the release of the ulnar artery. What does this finding indicate regarding the patient's circulation?
Following performance of the Allen test, the hand flushes within 2 seconds after the release of the ulnar artery. What does this finding indicate regarding the patient's circulation?
During Ratschow's test, a patient exhibits delayed redness in both legs (>10 seconds) after performing plantar and dorsiflexion exercises. This finding suggests:
During Ratschow's test, a patient exhibits delayed redness in both legs (>10 seconds) after performing plantar and dorsiflexion exercises. This finding suggests:
A patient's ankle-brachial index (ABI) is measured at 0.5. How would this result BEST be interpreted?
A patient's ankle-brachial index (ABI) is measured at 0.5. How would this result BEST be interpreted?
When performing the Ankle-Brachial Index (ABI), a reading of >1.4 may indicate:
When performing the Ankle-Brachial Index (ABI), a reading of >1.4 may indicate:
Which diagnostic imaging modality is considered the gold standard for evaluating peripheral arterial disease (PAD) but is also the MOST invasive?
Which diagnostic imaging modality is considered the gold standard for evaluating peripheral arterial disease (PAD) but is also the MOST invasive?
A patient presents with Raynaud's phenomenon, migratory superficial thrombophlebitis, and a history of heavy smoking. Which of the following is the MOST likely diagnosis?
A patient presents with Raynaud's phenomenon, migratory superficial thrombophlebitis, and a history of heavy smoking. Which of the following is the MOST likely diagnosis?
During the evaluation for thoracic outlet syndrome, a physician performs the costoclavicular maneuver. This maneuver BEST assesses:
During the evaluation for thoracic outlet syndrome, a physician performs the costoclavicular maneuver. This maneuver BEST assesses:
What finding indicates a positive Adson's test, suggestive of thoracic outlet syndrome?
What finding indicates a positive Adson's test, suggestive of thoracic outlet syndrome?
A patient experiences episodes of pallor, cyanosis, and rubor in their fingers upon exposure to cold. What is the MOST likely underlying cause of these color changes?
A patient experiences episodes of pallor, cyanosis, and rubor in their fingers upon exposure to cold. What is the MOST likely underlying cause of these color changes?
Which of the following BEST describes the usual direction of blood flow in the great saphenous vein (GSV)?
Which of the following BEST describes the usual direction of blood flow in the great saphenous vein (GSV)?
A patient with chronic venous insufficiency (CVI) reports increased leg swelling and discomfort after prolonged standing. What is the MOST accurate explanation?
A patient with chronic venous insufficiency (CVI) reports increased leg swelling and discomfort after prolonged standing. What is the MOST accurate explanation?
Which occupation is MOST strongly associated with an increased risk of varicose veins and chronic venous insufficiency?
Which occupation is MOST strongly associated with an increased risk of varicose veins and chronic venous insufficiency?
Elevating the legs typically provides relief for patients with CVI, but NOT for patients with advanced postthrombotic syndrome (PTS). Why does elevating the legs NOT typically provide relief for patients with advanced PTS?
Elevating the legs typically provides relief for patients with CVI, but NOT for patients with advanced postthrombotic syndrome (PTS). Why does elevating the legs NOT typically provide relief for patients with advanced PTS?
A patient with suspected chronic venous insufficiency exhibits small, dilated intradermal venules smaller than 1 mm in diameter. These are BEST described as:
A patient with suspected chronic venous insufficiency exhibits small, dilated intradermal venules smaller than 1 mm in diameter. These are BEST described as:
A patient with chronic venous insufficiency has developed firm, thickened skin around the ankle with a brownish discoloration. This is MOST consistent with:
A patient with chronic venous insufficiency has developed firm, thickened skin around the ankle with a brownish discoloration. This is MOST consistent with:
A patient presents with acute unilateral leg pain, swelling, and tenderness along the medial aspect of the calf. These signs and symptoms are MOST suggestive of:
A patient presents with acute unilateral leg pain, swelling, and tenderness along the medial aspect of the calf. These signs and symptoms are MOST suggestive of:
A patient with suspected deep vein thrombosis (DVT) has a negative D-dimer test result. The MOST appropriate next step is:
A patient with suspected deep vein thrombosis (DVT) has a negative D-dimer test result. The MOST appropriate next step is:
Which of the following ultrasound findings is MOST consistent with a diagnosis of acute deep vein thrombosis (DVT)?
Which of the following ultrasound findings is MOST consistent with a diagnosis of acute deep vein thrombosis (DVT)?
A patient exhibits edema of the neck and upper part of the chest as well as visible collateral veins in the same region. Which condition is MOST likely?
A patient exhibits edema of the neck and upper part of the chest as well as visible collateral veins in the same region. Which condition is MOST likely?
A patient presents with arm pain and swelling following multiple attempts at intravenous catheter insertion. The MOST likely venous complication is:
A patient presents with arm pain and swelling following multiple attempts at intravenous catheter insertion. The MOST likely venous complication is:
A patient experiences recurrent episodes of inflammation in different segments of the superficial venous system, without any identifiable local cause. This presentation is characteristic of:
A patient experiences recurrent episodes of inflammation in different segments of the superficial venous system, without any identifiable local cause. This presentation is characteristic of:
The lymphatic vessels of the upper extremity primarily drain into which regional lymph node group?
The lymphatic vessels of the upper extremity primarily drain into which regional lymph node group?
A patient presents with bilateral, symmetrical swelling of the lower extremities up to the hips, with a normal Stemmer sign. The MOST likely condition is:
A patient presents with bilateral, symmetrical swelling of the lower extremities up to the hips, with a normal Stemmer sign. The MOST likely condition is:
What physical examination finding suggests a diagnosis of lymphedema?
What physical examination finding suggests a diagnosis of lymphedema?
Atherothrombosis is a frequent cause of stenosis or occlusion in peripheral artery disease (PAD). Which of the following BEST describes atherothrombosis?
Atherothrombosis is a frequent cause of stenosis or occlusion in peripheral artery disease (PAD). Which of the following BEST describes atherothrombosis?
A patient reports experiencing pain in their lower extremities, specifically in the calf muscle, after walking two blocks. The pain is relieved by resting for a few minutes. This pattern is MOST consistent with:
A patient reports experiencing pain in their lower extremities, specifically in the calf muscle, after walking two blocks. The pain is relieved by resting for a few minutes. This pattern is MOST consistent with:
Which of the following is the MOST appropriate next step after detecting a vibration or buzzing sensation through palpation of an artery?
Which of the following is the MOST appropriate next step after detecting a vibration or buzzing sensation through palpation of an artery?
After performing the Allen's test, the hand takes 6 seconds to flush after the release of the radial artery, but the ulnar artery is patent. This indicates:
After performing the Allen's test, the hand takes 6 seconds to flush after the release of the radial artery, but the ulnar artery is patent. This indicates:
Following a Ratschow's test, a patient has a time to first redness of 3 seconds after hanging their feet down. Next steps would include:
Following a Ratschow's test, a patient has a time to first redness of 3 seconds after hanging their feet down. Next steps would include:
When measuring the Ankle-Brachial Index (ABI), the systolic blood pressure at the ankle level must be divided by:
When measuring the Ankle-Brachial Index (ABI), the systolic blood pressure at the ankle level must be divided by:
A patient undergoing vascular examination complains of pain in the fingers upon exposure to cold, progressing through stages of pallor, cyanosis, and redness. This clinical scenario is MOST suggestive of:
A patient undergoing vascular examination complains of pain in the fingers upon exposure to cold, progressing through stages of pallor, cyanosis, and redness. This clinical scenario is MOST suggestive of:
A patient presents with chronic venous insufficiency and reports discomfort in the legs that worsens with prolonged standing and improves with elevation. This is MOST likely due to:
A patient presents with chronic venous insufficiency and reports discomfort in the legs that worsens with prolonged standing and improves with elevation. This is MOST likely due to:
In the evaluation of a patient for suspected deep vein thrombosis (DVT) using venous ultrasonography, which of the following findings is MOST indicative of a thrombus?
In the evaluation of a patient for suspected deep vein thrombosis (DVT) using venous ultrasonography, which of the following findings is MOST indicative of a thrombus?
What is the MOST likely cause of lower limb edema with thickened, rigid skin, and Stemmer's sign?
What is the MOST likely cause of lower limb edema with thickened, rigid skin, and Stemmer's sign?
Flashcards
Peripheral Artery Disease (PAD)
Peripheral Artery Disease (PAD)
A common disease where arteries in the legs narrow, reducing blood flow.
Intermittent Claudication
Intermittent Claudication
A symptom of cramping muscle pain during activity, relieved by rest, due to reduced blood flow.
Ischemic Rest Pain
Ischemic Rest Pain
Leg pain that occurs even when resting, often worse at night, relieved by sitting or standing.
Leriche Syndrome
Leriche Syndrome
Signup and view all the flashcards
Subclavian Steal Syndrome
Subclavian Steal Syndrome
Signup and view all the flashcards
Trophic Changes in PAD
Trophic Changes in PAD
Signup and view all the flashcards
Acute Limb Ischemia (ALI)
Acute Limb Ischemia (ALI)
Signup and view all the flashcards
Palpation: Skin Temperature
Palpation: Skin Temperature
Signup and view all the flashcards
Arterial Thrill
Arterial Thrill
Signup and view all the flashcards
Allen's Test
Allen's Test
Signup and view all the flashcards
Ratschow's Exercise Test
Ratschow's Exercise Test
Signup and view all the flashcards
Distal (Ankle) Pressure
Distal (Ankle) Pressure
Signup and view all the flashcards
Ankle-Brachial Index (ABI)
Ankle-Brachial Index (ABI)
Signup and view all the flashcards
Thromboangiitis Obliterans
Thromboangiitis Obliterans
Signup and view all the flashcards
Thoracic Outlet Syndrome (TOS)
Thoracic Outlet Syndrome (TOS)
Signup and view all the flashcards
Adson's Test
Adson's Test
Signup and view all the flashcards
Raynaud's Phenomenon
Raynaud's Phenomenon
Signup and view all the flashcards
Chronic Venous Insufficiency (CVI)
Chronic Venous Insufficiency (CVI)
Signup and view all the flashcards
Varices
Varices
Signup and view all the flashcards
Spider Veins (telangiectasias)
Spider Veins (telangiectasias)
Signup and view all the flashcards
Venous Hypertension
Venous Hypertension
Signup and view all the flashcards
Skin Changes in CVI
Skin Changes in CVI
Signup and view all the flashcards
Superficial Thrombophlebitis
Superficial Thrombophlebitis
Signup and view all the flashcards
Migratory Thrombophlebitis
Migratory Thrombophlebitis
Signup and view all the flashcards
Lymphoedema
Lymphoedema
Signup and view all the flashcards
Stemmer sign
Stemmer sign
Signup and view all the flashcards
Study Notes
Vascular Examination
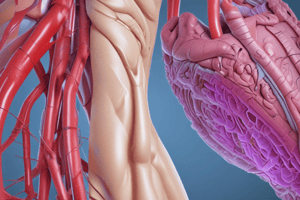
- Vascular examination encompasses the assessment of both arteries and veins, alongside lymphatic vessels
Exploration of Arteries
- Right and left common carotid arteries supply the head and neck
- Vertebral arteries contribute to brain blood supply
- The right subclavian artery branches off the brachiocephalic artery
- The brachiocephalic artery is only on the right side
- Renal arteries supply the kidneys
- The abdominal aorta feeds the common iliac arteries, which then supply the legs
- The brachial artery is in the upper arm
- The radial artery is also in the arm
- Femoral arteries supply the thighs
- Popliteal arteries are situated behind the knees
- Dorsalis pedis and posterior tibial arteries are located in the feet
Peripheral Artery Disease (PAD)
- PAD is marked by narrowing or blockage of arteries in the lower limbs
- Atherosclerosis and atherothrombosis are frequent causes of arterial narrowing and blockage
Key components of an Arterial Examination
- Gathering medical history, including family history and risk factors
- Includes lifestyle, like smoking
- Physical inspection, involving observation
- Palpation of pulses to assess arterial flow
- Auscultation to listen for abnormal sounds
Patient History in PAD Assessment
- Family history and lifestyle factors such as smoking are relevant
- Symptoms include intermittent claudication, rest pain in lower limbs, and cool, white fingers
- Ulcers or gangrene
- Pain in the arms after exercise is also a symptom
Details on PAD Symptoms
- Intermittent claudication is cramping muscle pain associated with muscle use, like walking
- Rapid relief occurs 3-4 minutes after rest
- Claudication pain location depends on where the arterial occlusion has occurred
- Ischemic rest pain is localized in the legs and worsens at night or when lying down
- It improves or disappears when sitting or standing
- Ischaemic defects mark the final stage of PAD development
Leriche Syndrome
- Leriche syndrome involves isolated atherosclerotic involvement of the aortic bifurcation and common iliac arteries
- High gluteal claudication and impotence are signs
Upper Limb Ischemia
- Upper limb ischemia presents as tiredness or pain in the arms after exercise and pain in the hand and fingers
- Subclavian steal syndrome involves reversed blood flow in the vertebral artery due to subclavian artery occlusion
Signs revealed through Inspection
- Inspection reveals trophic changes in the skin and its appendages
- In PAD, affected lower limbs may be paler and colder or turn red when hanging down
- Cyanotic coloring may be present in chronic ischaemia
- Swelling may develop with resting pain, worsening limb dependence and advanced ischemia
- Ulcers are usually located on the toes, heels, and bone protrusions, with finger ulcers in affected upper limbs
Acute Limb Ischemia (ALI)
- Acute arterial occlusion leads to ALI
- Characterized by sudden pain, pallor, poikilothermia, paresthesia, paralysis, and pulselessness
- Gangrene can result
Palpation Technique
- Palpation involves estimating skin temperature using the dorsal surface of fingers for comparison
Essential arterial Pulse Points
- Subclavian artery above the clavicle's center
- Axillary artery in the armpit, more palpable after abduction
- Brachial artery in the distal third of the arm, between the biceps and triceps
- Radial artery on the thumb side of the wrist
- Ulnar artery on the medial wrist side
- Femoral artery in the groin, just below the ligament
- Popliteal artery located deep in the knee.
- Relax knee with hands hugging knee
- Thumb above patella and fingers joining at the back of the knee
Pulses of the Lower Limb
- Posterior tibial artery behind the inner ankle
- Dorsalis pedis artery usually between the 1st and 2nd metatarsals
Auscultation Technique
- Auscultation identifies murmurs, signaling a change from laminar to turbulent flow
Auscultation Points
- Common carotid artery
- Above and below the clavicle
- In the groin
- In the medial thigh
- Over the popliteal artery
- Over the abdominal aorta, in the hypogastrium, and above the groin
Allen's Test
- Allen's test assesses blood flow to the hands and fingers
- Patient raises arms, and the examiner compresses forearm arteries
- Patient rhythmically opens and closes fists until the palms are pale, then relaxes arms
- Pressure is released to one, then the other, artery
- Normal color restoration in 3-5 seconds indicates patent arteries and palmar arches
Ratschow's Exercise Test
- Ratschow's test identifies suspected PAD
- With lower limbs bent, the patient performs plantar and dorsal flexion for 2 minutes
- Observe pale limbs
- Exercise stops prematurely due to pain
- Time is measured for first redness to appear on legs
- The normal time is < 5 seconds
- Vein filling time on the dorsal side of the leg should be < 10 seconds
- Diffuse skin redness on the entire leg < 15 seconds
Ankle Pressure Assessment
- ABI detects PAD
- Ankle-Brachial Index (ABI) is the systolic ankle pressure divided by the arm systolic pressure
- ABI correlates with severity
ABI Ranges
- Normal ABI: 1-1.4
- Mild to moderate impairment: 0.7-0.9
- Moderate to severe impairment: 0.4-0.69
- Severe to critical ischemia: ≤0.4
- Borderline: 0.9-0.99
- Add an exercise test
- Rigid arteries from diabetes or renal failure produce a value of >1.4
Hand-held Doppler device use
- Use doppler device on both arms and use the higher value
- Bilaterally measure ADP and ATP
- Use the higher value
Claudication interval
- Using a treadmill test to measure Claudication interval
Imaging methods
- USG (ultrasonography)
- AG (angiography)
- CTAG (computed tomographic angiography)
- MRAG (magnetic resonance angiography)
Thromboangiitis Obliterans (Buerger's Disease)
- Morbus Winiwarter
- Buerger affects the arteries segmentally, causing secondary thrombosis
- Primarily in men under 40 who smoke
- It presents with acral cyanosis, pain, coldness, migratory phlebitis, necroses, gangrenes, and screw-like collateral vessels
Thoracic Outlet Syndrome (TOS)
- TOS involves compression of the neurovascular bundle in the superior thoracic aperture
- Symptoms presents as pain, paraesthesia, swelling, discoloration.
- Vein enlargement can occur
- Various positional maneuvers are used in examination
Adson's Test
- Adson's test involves turning the head back towards the affected side
- Look for compression of the subclavian artery in the fissura scalenorum
- Scanlene syndrome or cervical rib syndrome can occur
Costoclavicular Maneuver
- Costoclavicular involves maximum shoulder contraction downwards and backwards.
- Look for compression between the 1st rib and collarbone
Hyperabduction Maneuver
- The hyperabduction maneuver involves elevation and turning the head to the opposite side of the affected part.
- Look for evidence of compression under the pectoralis minor.
- During the examination, detect the pulse of the radialis (weakening or disappearing of the pulse)
- Look for an abnormal murmur in the subclavian region
Raynaud's Phenomenon
- Raynaud's is caused by inadequate reactivity of finger arterioles to cold or emotional stress.
- Vasoconstriction occurs in the fingers, less frequently on the toes or ears, nose, or knees
- Sharply demarcated whitening begins
- Cyanosis will be followed 15-20 minutes later by erythema
- Patients can only have white fingers during seizure
- Colour changes are accompanied by pain and paraesthesia
Vein Examination
- Focuses on veins of the legs
- The venous system includes deep veins, superficial veins, and connection between surface systems.
Deep Veins
- Deep veins: vena femoralis communis, v. femoralis, v. profunda femoris, v. poplitea, double calf veins
- vv. tibiales posteriores, vv. tibiales anteriores, vv. fibulares ;
Superficial veins
- Superficial veins consist of great saphenous vein (GSV), small saphenous vein (SSV) and their branches GSV flows into femoral vein (saphenofemoral junction) SSV usually into popliteal vein (saphenopopliteal junction)
Varices and Chronic Venous Insufficiency (CVI)
- Varices of the legs and chronic venous insufficiency (chronic venous disease)
- Chronic venous insufficiency (CVI) is a common condition.
- It occurs because chronic failure of the venous system function in the legs
- Accumulation of blood in the veins (stasis)
- A permanent increase of venous pressure (venous hypertension)
Risk Factors/Triggers for Venous Insufficiency
- Risk factors include sustained static effort, lack of exercise, tight clothing, high heels, and smoking
- Hormonal Changes can trigger the disease
Subjective Complaints in CVI
- Heaviness, tension, and pain during the day
Objective Signs of CVI
- Objective signs: Dilated veins, oedema, and skin changes
CVI Skin Changes
- Skin changes usually affect the area of the inner ankle and lower third of the lower leg
- Look for hyperpigmentaton, white atrophy, lipodermatosclerosis, and venous eczema
Instrumental and Imaging Tests
- Photopletysmography provides information on venous function
- A blood refill time is determined via this test
Ultrasound Use
- To determine velocity and direction of blood flow, venous reflux, and obstruction
Deep Vein Thrombosis (DVT)
- Is total or partial occlusion of deep vein by a blood clot (thrombus)
- It is relevant to know the previous incidence from the patient or relative and family
- Gynaecological history can be important - the risk of VTE increases significantly during pregnancy
- Physical findings feature swelling, pain (worse while standing and walking)
- Look for Colour changes
Symptoms of a Pulmonary Embolism Comlication
- Shortness of breath, chest pain, cough, and haemoptysis
Superficial Veins Thrombosis/Trombophlebitis
- Superifical Thrombosis in the lumen of superficial vein segment(s)
- There is inflammation of the wall and perivenous skin and subcutaneous tissue
- High temperature of the surrounding tissue, redness, painful to palpation
- Occurs due to varices and the segment usually varies
Migratory Thrombophlebitis
- Migratory thrombophlebitis is recurrent and migratory inflammation on various segments of the superficial venous system
- It occurs without apparent local cause with autoimmune diseases and malignancies
Examination of Lymphatic Vessels
- Lymphatic vessels divide into superficial and deep lymphatic vessels
- Upper limbs lead into the axillary nodes and lower limbs into inguinal nodes
Lymphedema
- Lymphedema is dysfunction of lymphatic drainage which may result in the following conditions.
- It occurs when accumulation of lymph in the interstitium and high-protein swelling.
Primary vs secondary Lymphoedema
- In primary cases look for insufficient development of vessels
- In secondary cases, look for Lesion of the lymphatic system (tumour cells, injury, or surgery)
- Look for a stemmer sign or columnar appearance of the calf and limbs
Imaging Tests for Lymphedema
- Ultrasound can be used to look for a 'honeycomb' structure underneath superficial issue
- Lymphoscintigraphy also can be performed to administer a radionuclide-labelled carrie
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.