Podcast
Questions and Answers
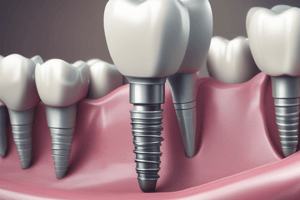
Why is titanium the material of choice for osseointegration dental implants?
Why is titanium the material of choice for osseointegration dental implants?
- It has excellent mechanical properties and is biocompatible with living tissues. (correct)
- It is weaker than cortical bone, allowing for more natural stress distribution.
- It undergoes significant changes in the biological environment over time.
- It is easily absorbed by the body, preventing any long-term integration.
What is a key disadvantage of Hydroxyapatite coating on dental implants?
What is a key disadvantage of Hydroxyapatite coating on dental implants?
- It is not suitable for use with synthetic bone material.
- It often shows cracks or complete loss of coating after five years, leading to peri-implantitis. (correct)
- It prevents rapid osseo-induction.
- It has a low initial success rate.
In the context of implant materials, what is Roxolid composed of?
In the context of implant materials, what is Roxolid composed of?
- Approximately 15% zirconium and 85% titanium. (correct)
- A ceramic material with a zirconia coating.
- Pure titanium with a corrosion-resistant alloy.
- A combination of titanium and hydroxyapatite.
Which of the following statements accurately describes osseointegration?
Which of the following statements accurately describes osseointegration?
What is a major disadvantage of subperiosteal implants?
What is a major disadvantage of subperiosteal implants?
Historically, dental implants can be traced back to which ancient civilizations?
Historically, dental implants can be traced back to which ancient civilizations?
According to the information, what percentage of dental implants might fail without primary stability?
According to the information, what percentage of dental implants might fail without primary stability?
Which of the following is a characteristic of blade implants?
Which of the following is a characteristic of blade implants?
What is the primary reason why Formiggini's spiral implant design failed?
What is the primary reason why Formiggini's spiral implant design failed?
Which of the following is NOT a disadvantage of sub-mucosal implants?
Which of the following is NOT a disadvantage of sub-mucosal implants?
Why should clinicians wait until after the age of 18 to place dental implants?
Why should clinicians wait until after the age of 18 to place dental implants?
Which of the following is generally considered an absolute contraindication for dental implants?
Which of the following is generally considered an absolute contraindication for dental implants?
How does the average intake and excretion rates of Titanium impact its accumulation in the human body?
How does the average intake and excretion rates of Titanium impact its accumulation in the human body?
What is the primary goal of implant coating materials?
What is the primary goal of implant coating materials?
According to the provided information, what is the primary difference between one-stage and two-stage surgical approaches for endosseous implant placement?
According to the provided information, what is the primary difference between one-stage and two-stage surgical approaches for endosseous implant placement?
What is the primary mechanical difference between bone-level and tissue-level implants?
What is the primary mechanical difference between bone-level and tissue-level implants?
What is the primary concern when performing dental implant procedures on heavy smokers?
What is the primary concern when performing dental implant procedures on heavy smokers?
What is the significance of the ADA’s recommendation for implant systems?
What is the significance of the ADA’s recommendation for implant systems?
Why is patient motivation and cooperation towards maintaining good oral hygiene important for implant success?
Why is patient motivation and cooperation towards maintaining good oral hygiene important for implant success?
According to the information, what force generated by para-functional habits can cause implant failure?
According to the information, what force generated by para-functional habits can cause implant failure?
The design of a subperiosteal implant should include how many rods emerging from the gingiva to insert into the denture?
The design of a subperiosteal implant should include how many rods emerging from the gingiva to insert into the denture?
When is a trans-mandibular implant (TMI) typically indicated?
When is a trans-mandibular implant (TMI) typically indicated?
Which of the following oral conditions is NOT an intraoral contraindication for dental implants?
Which of the following oral conditions is NOT an intraoral contraindication for dental implants?
In cases of radiation therapy, what measure can be taken to improve the success rate of dental implants?
In cases of radiation therapy, what measure can be taken to improve the success rate of dental implants?
Flashcards
What is a Greenfield implant?
What is a Greenfield implant?
An implant that consists of two pieces of hollow basket made of Platinum, soldered with a supra-structure, where the crown is placed. However, it eventually failed.
What implant did Stock (1939) develop?
What implant did Stock (1939) develop?
The first Co-Cr screw-shaped implant inserted in freshly extracted sockets, highlighting the importance of this for implant success.
What is osseointegration?
What is osseointegration?
Term for direct structural and functional connection between living bone and the surface of an alloplastic material achieved during functional loading at a microscopic level.
What is Formiggini (1947) Spiral design implant?
What is Formiggini (1947) Spiral design implant?
Signup and view all the flashcards
What are implant materials?
What are implant materials?
Signup and view all the flashcards
Why is Titanium the material of choice for dental implants?
Why is Titanium the material of choice for dental implants?
Signup and view all the flashcards
What is Titanium-Plasma-Spray implant coating?
What is Titanium-Plasma-Spray implant coating?
Signup and view all the flashcards
What is Sand-blasted-Long grit-Acid-etched implant coating?
What is Sand-blasted-Long grit-Acid-etched implant coating?
Signup and view all the flashcards
What is a Sub-mucosal implant insert?
What is a Sub-mucosal implant insert?
Signup and view all the flashcards
What are Trans-osseous implants?
What are Trans-osseous implants?
Signup and view all the flashcards
What is a Sub-periosteal implant?
What is a Sub-periosteal implant?
Signup and view all the flashcards
What are bone level and tissue level implants?
What are bone level and tissue level implants?
Signup and view all the flashcards
What about bisphosphonates usage on dental implant?
What about bisphosphonates usage on dental implant?
Signup and view all the flashcards
Para-functional habits as contraindication
Para-functional habits as contraindication
Signup and view all the flashcards
What are the indications for dental implants for completely edentulous individuals
What are the indications for dental implants for completely edentulous individuals
Signup and view all the flashcards
what is the IMZ implant system?
what is the IMZ implant system?
Signup and view all the flashcards
Why is patient oral hygiene important before implants?
Why is patient oral hygiene important before implants?
Signup and view all the flashcards
What implant did Scialom (1962) introduce?
What implant did Scialom (1962) introduce?
Signup and view all the flashcards
what implant did Dahl developed?
what implant did Dahl developed?
Signup and view all the flashcards
What are Linkow (1964) Vent-implants made from Cr-Nickel alloy?
What are Linkow (1964) Vent-implants made from Cr-Nickel alloy?
Signup and view all the flashcards
What are the absolute contraindications for implants?
What are the absolute contraindications for implants?
Signup and view all the flashcards
Study Notes
- Dental implants have been used for 25-30 years
- Implant materials include titanium, ivory, hydroxyapatite, and ceramics
- Over 50 implant systems are available in Jordan
- Dental implants can be traced back to the ancient Egyptian and South American cultures from the 18th century
- Dentists used alloplastic materials like gold, porcelain, ivory, and Indian rubber to replace lost teeth in the 19th century
- Poor people's teeth were used to replace rich people's teeth, splinted with gold wire in old times
Historical Implant Systems
- Greenfield (1913): Introduced the endosteal implant consisting of a hollow basket made of platinum, soldered with a supra-structure for crown placement, but it failed
- Stock (1939): Inserted the first Co-Cr screw-shaped implant in freshly extracted sockets, noting the need for primary stability, which impacts 80% of implant success
- Formiggini (1947): Introduced the spiral design, similar to basal implants and dependent on the mechanical lock of the screw in compact bone and failed due to the high rate of resorption
- Cherchieve (1962): Introduced a double-helical design (Co-Cr)
- Scialom (1962): Introduced a "street of needles" design with a bladelike supra-structure
- Dahl (1943): Introduced the use of subperiosteal dental implants in clinical trials, modified by Goldberg & Greshkoff (1949), which still exists in the US
- The Subperiosteal dental implant is made of a Co-Cr framework for highly resorbed lower ridges
- The shortest dental implant is 6 mm
- Subperiosteal dental implants can't be used in the maxilla
- A flap is opened from the retromolar pad to expose bone, then an impression is taken, and a Co-Cr denture is designed
- It is a mechanical implant, where there is no osseointegration, and retention is purely mechanical, as the implant sits on the alveolar ridge.
- Linkow (1964): Introduced the Vent-implants made from Cr-Nickel alloy
- Linkow didn't believe in osseointegration and used fibro-osteointegration.
- Vent implants are made of titanium or ivory for narrow ridges
- It has a blade that is inserted in the bone and an abutment where the crown is placed
- Blade implants exist and are made of titanium but mechanical retention only
- Roberts & Roberts (1970): Introduced the Ramus Frame Implant with a tripod shape, that failed
- Small (1975): Introduced the Mandibular-Stable Implant, similar to trans-fixation screws, that no longer exists
- Bosker (1986): Introduced the Trans-mandibular Implant (TMI) for severely atrophied mandibles from canine to canine posteriorly
TMI details
- TMI increases bone level due to compression and tension and is used when the mandible is resorbed to less than 4 mm
- TMI consists of pure gold using an extraoral approach commonly used if a conventional osseointegrated implant is not indicated.
- In TMI, seven screws are placed, with three staying in bone, and four exposed to the oral cavity
- It is performed under general anesthesia and depends on mechanical lock for stability.
- Branemark (1952): discovered the biocompatibility of titanium when investigating wound healing (titanium plates in a rabbit's femur)
- Branemark (1969): described osseointegration, followed by Schroeder et al (1977)
- There are approximately 600 implant systems from 146+ manufacturers worldwide
- An implant system should be recommended by the ADA with 5-year follow-up in 2 or 3 dental centers with 75% success, but most aren't
Integration Types
- Osseointegration: Direct structural and functional connection between living bone and the surface of alloplastic material at a microscopic level. A time-dependent healing process with rigid fixation achieved and maintained with functional loading
- Fibro-integration: The belief that fibrous tissue should mimic the PDL; failure rate of >75% after 5 years. This allows slight tooth movement
Implant Materials
- Metallic materials include gold, stainless steel, silver, platinum, iridium, and titanium
- Nonmetallic materials include Indian rubber, ivory, porcelain, polymers, ceramic, carbon, and zirconia
- Roxolid is composed of 15% zirconium and 85% titanium
- Pure titanium (99.6% Ti, 0.4% Ni) is the choice for osseointegration due to biocompatibility, mechanical properties, histological contact, and corrosion resistance
- Chemical properties are determined by the surface oxide layer. Ti ions are found near bone, in peri-implant mucosa, and in the liver, spleen, and kidney, the biological half-life of Ti is (320days)
- Titanium is used in maxillofacial fractures, mini-screws in ortho, and dental implants, while Zirconia is only for dental implants
Titanium Vs Zirconia
- Titanium has easy workability, while Zirconia is difficult
- Both have superior corrosion and wear resistance and are biocompatible -Titanium has High yield strength 895Mpa, while Zirconia has 1000 MPa
- Both have high tensile strength, high compressive strength
- Titanium has a high fracture toughness (66 MPa), while Zirconia has 6 – 8 MPa
Implant coating materials
- Materials introduced to roughen the implant surface for increased bone bond strength
- Titanium-Plasma-Spray (TPS) processed at 3000° C and used until the 90s but is not used anymore.
- Sand-blasted-Long grit-Acid-etched (SLA) reduces healing time to 2.5 months in the maxilla and 1.5 months in the mandible, and it is still used.
- Bioactive materials (SLA active) needs 2 weeks for the mandible and 3 weeks for the maxilla, but double the price of SLA
- Hydroxyapatite coating is a synthetic bone material, used since the mid-1980s has rapid Osseo-induction and has a high success rate in the first 3-years
- Hydroxyapatite coating has high failure rates after 5 years of function, shows cracks or loss of coating and invasion of micro-organisms leading to peri-implantitis/resorption
- The methods are coating include Sand-blasting, Acid-etch, and Laser
Implant classifications and materials
- Bio-tolerant materials: Stainless Steel, Co-Cr, Gold alloy, PMMA with Fibrous tissues Distant from bone.
- Bio-inert materials: Titanium, Ceramic that Contact bone
- Bio-active materials: Bio-ceramic, Hydroxyappatite that bond to bone
- Sub-mucosal implant is a buttonlike retention device inserted underneath the mucosa of the residual ridge that is discontinued
- Disadvantages of Sub-mucosal implants include poor retention, short survival rates, trapped food debris, and acute bacterial infection.
- (016): they are inserted underneath the mucosa after the elevation of a flap and consist of a button-like retention device.
- Titanium mucosal insert are mm in the bone, where the bone is drilled to achieve the minimum preparation that is not recommended to be used
- The sub-periosteal implant consists of a metallic framework placed on the superior surface of the bone jaw and kept in place by the overlying periosteum with low success rates with time
- A flap is reflected, an impression is taken, and a cast is poured where a another flap is reopened (major surgery) and the framework is inserted, which has posts for an overdenture
- Nowadays, an extraoral scanner can get a 3D impression of the mandible, so the flap is only opened once
- Trans-osseous implants: are inserted full thickness, for the atrophic mandible
- A. Mandibular Stable Bone Plate implants (MSBP) need GA, and results in an extra-oral scar made from pure gold
- Trans-Mandibular Implant (TMI) needs GA, is limited to the lower jaw, and needs an extra-oral surgical approach often done on old patients
- Endosseous implant classification depends on the number of surgical steps
- One surgical step with ITI by Straumann is non-submerged, with a gingival former in the oral cavity
- With Two surgical steps withBranemark system that is submerged, with a second to place gingival former
- Implants systems based on Branemark system, such as steri-Oss, Astra, IMZ (not available anymore), Tubingen ( Frialit1 / Frialit2 / Frialit+ / Friadent / Frialoc / Frios / Xiv), Bicone, Piteasy, 3i. Biomet 3i: Osseotite / Nanotite, Zimmer: Calcitek / Integral / Omniloc, Biohorizons.
- Osseointegration was introduced by Dr. Branemark
- Bone level and tissue level are the most popular implants worldwide. The bone level implant ends at the alveolar ridge, 0.5mm above the bone. The tissue extends 1.5 mm above the bone part, where the remaining part is a smooth collar
- Nowadays, the bone level implant is used used in posterior areas. For missing 6 teeth, if the abutment teeth have drifted decreasing the dimension, the bone level implant is used
- It is also used when we have a limited amount of over-eruption, with a .5mm collar, that's in the anterior area
- Implants used to be one piece where the fixture and abutment were connected but are now separate allowing angles from 5° to 30°
- IMZ was the first to allow connecting with natural teeth and the root has intra-mobile element mimics the PDL that acts as a stress breaker that prevents harmful effects, but has to change every 8 months.
- Normal endosseous implants cannot connects to teeth because they cause drift (titanium is 6x stronger than cortical bone
- There are implants with a taper that is narrow apically and wide coronally
- Branemark system is characterized by the threads on the implant.
Implant Candidates
- Good oral hygiene and bone growth after 18
- Proper indications are required
Indications for Implants
- Completely edentulous individuals in both or one arches, If more than 6-fixtures the choice is implant supported prosthesis (fixed bridges). If less 2; implant remained over dentures
- Partially edentulous individuals where restoration is not possible means of bridges
- A Kennedy Class I may be considered, when you can not restore teeth due to osseointegration
- Tooth replacement where the patient refused to prepare the adjacent sound teeth, especially esthetic area
- Patients with compromised denture bearing area
- Hyperactive gagging reflex
- Psychological and emotional problems and unrealistic expectations
- Par function
- Poor oral muscular coordination
- Hypodontia
Contraindications
- Intra and Relative
Contraindications (Intraoral)
- Skeletal III
- Alveolar infectin Pathological lesion
- Acute ginguvitis
- Refer oral medicine to department
Contraindications (Relative)
- Insufficient poor bone quantity
- Hematology
- Metabolic disorders
- Psychological
- HIV is is not a contra indicator if they are honest
- Aging should not be ignored unless there are signs of life expecting
Radiation Issues
- Oral effects Radiation cause zero stoma.
- Hyper baric
- Diabetes cause Alveolar bone loss
Osteoperosis
- no relationship between osteoporosis bisphosphonates & Paget disease
- smoking is a risk factor protocol 1 week prior should stop smoking and at least 8 weeks after
Absolute
- cardio vascular
- angina 1 tear wait Are not contraindicated
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.