Podcast
Questions and Answers
Which of the following factors does NOT directly stimulate the synthesis of hepcidin?
Which of the following factors does NOT directly stimulate the synthesis of hepcidin?
- Bone morphogenetic protein 6 (BMP6)
- Diferric transferrin
- Matriptase 2 (TMPRSS6) (correct)
- Transferrin receptor 2 (TFR2)
In the context of iron deficiency, how does the absence of diferric transferrin affect hepcidin synthesis?
In the context of iron deficiency, how does the absence of diferric transferrin affect hepcidin synthesis?
- It prevents the formation of the signaling complex involving TFR2, HJV, and HFE, reducing hepcidin synthesis. (correct)
- It stimulates matriptase 2 activity, indirectly promoting hepcidin synthesis.
- It causes TFR1 to bind to HFE, leading to enhanced hepcidin synthesis.
- It leads to increased BMP synthesis, resulting in higher hepcidin levels.
What is the primary function of hepcidin in iron homeostasis?
What is the primary function of hepcidin in iron homeostasis?
- To inhibit iron release from storage sites. (correct)
- To promote iron absorption from the intestines.
- To stimulate the production of red blood cells.
- To increase iron utilization by cells.
Which of the following is NOT a consequence of elevated hepcidin levels?
Which of the following is NOT a consequence of elevated hepcidin levels?
How does the interaction between diferric transferrin and transferrin receptor 2 (TFR2) contribute to hepcidin synthesis?
How does the interaction between diferric transferrin and transferrin receptor 2 (TFR2) contribute to hepcidin synthesis?
Which factor predominantly favors the absorption of iron in the human body?
Which factor predominantly favors the absorption of iron in the human body?
What is the role of erythroferrone in relation to hepcidin secretion?
What is the role of erythroferrone in relation to hepcidin secretion?
Which of these conditions is likely to result in high levels of plasma hepcidin?
Which of these conditions is likely to result in high levels of plasma hepcidin?
How is iron absorption regulated in the enterocyte after dietary intake?
How is iron absorption regulated in the enterocyte after dietary intake?
What is a significant consequence of ineffective erythropoiesis on iron metabolism?
What is a significant consequence of ineffective erythropoiesis on iron metabolism?
Flashcards are hidden until you start studying
Study Notes
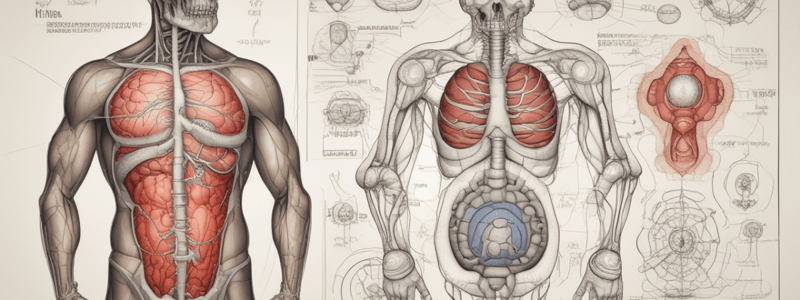
Hepcidin Overview
- Hepcidin is a liver-produced polypeptide and major hormonal regulator of iron homeostasis.
- It inhibits iron release from macrophages, intestinal epithelial cells, and other cells by interacting with ferroportin, a transmembrane iron exporter.
- Elevated hepcidin levels reduce both iron absorption and release from macrophages.
Control of Hepcidin Expression
- Hepcidin synthesis is influenced by factors such as iron status, cytokines during inflammation, erythropoiesis, and hypoxia.
- In iron overload, high plasma hepcidin levels are maintained via differentiation in liver sinusoidal cells stimulated by diferric transferrin.
- Bone morphogenetic proteins (BMPs), particularly BMP6, bind to BMPRs on liver cells, enhancing hepcidin synthesis through signaling proteins SMADs.
- In iron deficiency, reduced levels of diferric transferrin lead to decreased BMP synthesis, refusal of Hepcidin synthesis, and subsequent iron overload in cases of ineffective erythropoiesis.
Factors Affecting Hepcidin
- Erythroblasts release erythroferrone, suppressing BMP-mediated signaling, resulting in low hepcidin levels during increased erythroblast activity.
- Hypoxia inhibits hepcidin synthesis, while inflammation (via IL-6 and other cytokines) stimulates hepcidin production to lower plasma iron and inhibit bacterial growth.
Dietary Iron Sources
- Iron is present in food as ferric hydroxides and protein complexes, with meat (especially liver) providing better absorption than vegetables or dairy.
- A typical Western diet contains 10-15 mg of iron daily, with only 5-10% absorption, increased to 20-30% during pregnancy or deficiency.
Factors Influencing Iron Absorption
-
Factors Favoring Absorption:
- Inorganic iron in the ferrous form (Fe2+)
- Acids (hydrochloric acid, vitamin C) and solubilizing agents (sugars, amino acids)
- Reduced serum hepcidin and conditions of ineffective erythropoiesis
-
Factors Reducing Absorption:
- Haem iron and ferric iron (Fe3+)
- Alkaline conditions (antacids) and precipitating agents (phytates, phosphates, tea)
- Increased serum hepcidin and inflammation
Iron Absorption Mechanism
- Organic dietary iron is partially absorbed as haem and partially converted to inorganic iron in the stomach and duodenum.
- Absorption mainly occurs in the duodenum through enterocyte microvilli via the DMT-1 protein that transfers iron into the cell.
- Ferroportin regulates iron exit into portal plasma; its absorption is adjusted according to body needs by modulating DMT-1 and ferroportin levels.
- Enzymes like ferrireductase convert Fe3+ to Fe2+ in the gut lumen, and hephaestin oxidizes Fe2+ back to Fe3+ for binding to transferrin.
Daily Iron Requirements
- Iron requirements vary with age and sex, highest in pregnant women, adolescents, and menstruating females.
- These groups are at greater risk for iron deficiency due to additional losses or inadequate intake.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.