Podcast
Questions and Answers
What is a consequence of platelet activation following adhesion?
What is a consequence of platelet activation following adhesion?
- Decreased platelet aggregation
- Secretion of calcium and ADP (correct)
- Enhanced red blood cell production
- Increased viscosity of blood
Which factor is NOT part of Virchow's triad, which influences thrombus formation?
Which factor is NOT part of Virchow's triad, which influences thrombus formation?
- Endothelial injury
- Blood hypercoagulability
- Stasis of blood flow
- Blood viscosity (correct)
What effect does endothelial injury have on the vascular system?
What effect does endothelial injury have on the vascular system?
- Promotes vasodilation
- Increases platelet adhesion (correct)
- Enhances local oxygen delivery
- Reduces coagulation factor activity
What condition is primarily associated with stasis in thrombus formation?
What condition is primarily associated with stasis in thrombus formation?
Which of the following is considered a primary hypercoagulable state?
Which of the following is considered a primary hypercoagulable state?
What is a consequence of turbulence in blood flow regarding thrombosis?
What is a consequence of turbulence in blood flow regarding thrombosis?
How does oral contraceptive use contribute to hypercoagulability?
How does oral contraceptive use contribute to hypercoagulability?
What role does thrombin play in the formation of a platelet plug?
What role does thrombin play in the formation of a platelet plug?
What is a characteristic of arterial thrombi compared to venous thrombi?
What is a characteristic of arterial thrombi compared to venous thrombi?
Which factor contributes to hypercoagulability according to the information provided?
Which factor contributes to hypercoagulability according to the information provided?
What is the primary distinction between ante mortem and post mortem clots?
What is the primary distinction between ante mortem and post mortem clots?
What do lines of Zahn in a thrombus represent?
What do lines of Zahn in a thrombus represent?
What is the fate of a thrombus that undergoes dissolution?
What is the fate of a thrombus that undergoes dissolution?
What is NOT true about thrombi that form in flowing blood?
What is NOT true about thrombi that form in flowing blood?
Where do thrombi generally begin to form?
Where do thrombi generally begin to form?
How do venous thrombi tend to extend?
How do venous thrombi tend to extend?
What is the primary role of endothelial cells in normal hemostasis?
What is the primary role of endothelial cells in normal hemostasis?
What initiates primary hemostasis following vascular injury?
What initiates primary hemostasis following vascular injury?
What is the role of thrombin in the hemostatic process?
What is the role of thrombin in the hemostatic process?
Which component is not involved in the process of hemostasis?
Which component is not involved in the process of hemostasis?
Which factor is released by platelets to promote aggregation at the site of injury?
Which factor is released by platelets to promote aggregation at the site of injury?
What occurs during secondary hemostasis after the formation of a platelet plug?
What occurs during secondary hemostasis after the formation of a platelet plug?
What triggers the activation of the coagulation cascade?
What triggers the activation of the coagulation cascade?
After endothelial cell injury, what is the first change that facilitates platelet adhesion?
After endothelial cell injury, what is the first change that facilitates platelet adhesion?
Flashcards are hidden until you start studying
Study Notes
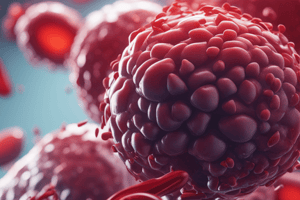
Normal Hemostasis
- Maintains blood in a fluid state in normal vessels
- Forms a localized hemostatic plug at the site of vascular injury
Thrombosis
- Pathologic counterpart of hemostasis
- Formation of a blood clot (thrombus) within intact vessels
Hemostasis and Thrombosis
- Both involve vascular wall, platelets and coagulation cascade
Normal Hemostasis
- Starts with arteriolar vasoconstriction
- Allows platelets to adhere and be activated
- Activated platelets change shape from small rounded disks to flat plates
- Release of secretory granules recruits additional platelets resulting in a hemostatic plug
- This is known as primary hemostasis
Tissue Factor
- Exposed at the site of injury
- Acts in conjunction with factor VII to activate the coagulation cascade
- Leads to thrombin generation, cleaving circulating fibrinogen into insoluble fibrin forming a meshwork
- This is secondary hemostasis
- Thrombin also induces further platelet recruitment and granule release
- Fibrin and platelet aggregates form a solid permanent plug to prevent further hemorrhage
Endothelial Cells and Coagulation
- Intact normal endothelial cells prevent platelet and coagulation factor activation
- Damaged or inflamed endothelial cells upregulate expression of procoagulant factors that promote clotting
- Decrease expression of anticoagulant factors
- Loss of endothelial integrity exposes subendothelial vWF and collagen, stimulating platelet adhesion, activation and clot formation
Platelet Adhesion, Activation, and Aggregation
- Endothelial injury exposes underlying basement membrane ECM
- Platelets adhere to ECM through platelet GpIb receptors binding to vWF
- Adhesion leads to platelet activation, which involves secretion of platelet granule contents, including calcium and ADP
- Platelet activation also results in dramatic changes in shape and membrane composition and activation of GpIIb/IIIa receptors
- GpIIb/IIIa receptors on activated platelets form bridging crosslinks with fibrinogen leading to platelet aggregation
- Concomitant activation of thrombin promotes fibrin deposition, cementing the platelet plug in place
Thrombosis
- Influenced by three primary factors (Virchow's triad):
- Endothelial injury
- Stasis or turbulence of blood flow
- Blood hypercoagulability
Endothelial Injury
- Important cause of thrombosis, particularly in the heart and arteries
- Ex: thrombosis occurs in cardiac chambers after myocardial infarction and over ulcerated plaques in atherosclerotic arteries
- Physical loss of endothelium exposes subendothelial ECM, releases tissue factor, and reduces local production of PGI2 and plasminogen activators
- Endothelial dysfunction occurs in hypertension, bacterial products, radiation injury, hypercholesterolemia, and toxins absorbed from cigarette smoke
Alterations in Normal Blood Flow
- Turbulence contributes to thrombosis by causing endothelial injury or dysfunction, and by forming local stasis
- Stasis is a major contributor to the development of venous thrombi
- Normal blood flow is laminar, with platelets flowing centrally in the vessel lumen and separated from the endothelium by a clear zone of plasma
Hypercoagulability
- Any alteration of the coagulation pathways that predisposes to thrombosis
- Divided into primary (genetic) and secondary (acquired) disorders
Primary (inherited) hypercoagulable states
- Ex: mutations in the prothrombin gene
Causes of Secondary Hypercoagulable states
- Cardiac failure and trauma in both stasis or vascular injury
- Oral contraceptive use and hyperestrogenic state of pregnancy, related to increased hepatic synthesis of coagulation factors and reduced synthesis of antithrombin III
- Advanced age due to increasing platelet aggregation
- Smoking and obesity promote hypercoagulability
Morphology
- Thrombi can develop anywhere in the cardiovascular system
- Size and shape depend on site of origin and cause
- Arterial or cardiac thrombi typically begin at sites of endothelial injury or turbulence
- Venous thrombi characteristically occurring at sites of stasis
- Thrombi are focally attached to the underlying vascular surface
- Arterial thrombi tend to grow in a retrograde direction
- Venous thrombi extend in the direction of blood flow
- Propagating portion of a thrombus tends to be poorly attached and therefore prone to fragmentation, generating an embolus
- Thrombi can have grossly (and microscopically) laminations called lines of Zahn, representing pale platelet and fibrin layers alternating with darker red cell–rich layers
- Important to note that lines of Zahn are only found in thrombi that form in flowing blood, usually distinguishing antemortem thrombosis from postmortem clots
Postmortem Clotting of blood
- Blood separates:
- Upper plasma layer: translucent, like chicken fat
- Lower red blood cell layer: very red and resembles red current jelly
Difference between post/ante mortem clotting:
- Post mortem: no damage to inner surface of vessel and clot can be easily removed
- Ante mortem: firmly attached to underlying vascular endothelium, has a white interior and is layered
Fate of the Thrombus
- Propagation: thrombi accumulate additional platelets and fibrin, eventually causing vessel obstruction
- Embolization: thrombi dislodge or fragment and are transported elsewhere in the vasculature
- Dissolution: thrombi are removed by fibrinolytic activity
- Organization and recanalization: thrombi induce inflammation and fibrosis (organization)
- This can eventually recanalize (re-establishing some degree of flow)
- Or be incorporated into a thickened vessel wall
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.