Podcast
Questions and Answers
What are the two main types of hemoglobinopathy disorders?
What are the two main types of hemoglobinopathy disorders?
The two main types of hemoglobinopathy disorders are quantitative disorders, which involve reduced or absent synthesis of alpha or beta globin chains, and qualitative disorders, which involve the synthesis of an abnormal hemoglobin.
What is the molecular basis of sickle cell disease?
What is the molecular basis of sickle cell disease?
Sickle cell disease is caused by a single nucleotide substitution in the beta globin gene, resulting in the replacement of glutamate with valine at position 6.
What is the dominant type of hemoglobin found in adults after 3-6 months of age?
What is the dominant type of hemoglobin found in adults after 3-6 months of age?
The dominant type of hemoglobin found in adults after 3-6 months of age is HbA.
On which chromosomes are the genes for alpha and beta globin located?
On which chromosomes are the genes for alpha and beta globin located?
What are the three types of embryonic hemoglobin?
What are the three types of embryonic hemoglobin?
What are the consequences of deoxygenation of mutant hemoglobin (Hb)?
What are the consequences of deoxygenation of mutant hemoglobin (Hb)?
How does sickled red blood cells affect blood flow and vaso-occlusion?
How does sickled red blood cells affect blood flow and vaso-occlusion?
What factor is associated with the severity of sickle cell disease?
What factor is associated with the severity of sickle cell disease?
Name one factor that increases hemoglobin S polymerization.
Name one factor that increases hemoglobin S polymerization.
What effect does having sickle cell trait have on malaria infection in children?
What effect does having sickle cell trait have on malaria infection in children?
Flashcards
Hemoglobinopathy
Hemoglobinopathy
Genetic disorders affecting hemoglobin structure or production.
Sickle Cell Anemia
Sickle Cell Anemia
Chronic hemolytic anemia caused by a mutation in the β globin gene.
Normal Hemoglobin Types
Normal Hemoglobin Types
Majorly HbA, with minor types HbF and HbA2 present in adults.
Quantitative Disorder
Quantitative Disorder
Signup and view all the flashcards
Qualitative Disorder
Qualitative Disorder
Signup and view all the flashcards
Deoxygenation of mutant Hb
Deoxygenation of mutant Hb
Signup and view all the flashcards
Sickled cells adhesion
Sickled cells adhesion
Signup and view all the flashcards
Vicious cycle in sickle cell disease
Vicious cycle in sickle cell disease
Signup and view all the flashcards
Factors increasing Hb S polymerization
Factors increasing Hb S polymerization
Signup and view all the flashcards
Sickle trait and malaria
Sickle trait and malaria
Signup and view all the flashcards
Study Notes
Hemoglobinopathy Overview
- Hemoglobin is composed of heme and globin chains.
- Normal adult blood has three types of hemoglobin.
- HbA is the dominant type after 3-6 months of age. It has 2 alpha and 2 beta chains.
- HbF (2 alpha, 2 gamma) and HbA2 (2 alpha, 2 delta) are minor types of hemoglobin.
- Embryonic hemoglobin types include Hb Gower (Zeta 2, E2), Hb Portland (Zeta2, Gamma 2), and Hb Gower2 (2Alpha, 2E).
- Fetal hemoglobin is HbF (2Alpha, 2Gamma).
- Globin genes are located on chromosomes 11 (β) and 16 (α).
- There are typically 4 alpha globin genes and 2 beta globin genes.
- Hemoglobin abnormalities are common worldwide.
- They are frequently seen in tropical and subtropical areas.
Classification of Hemoglobinopathies
- Classification is based on either quantitative or qualitative changes.
- Quantitative disorders involve reduced or absent synthesis of alpha or beta globin chains.
- Qualitative disorders relate to synthesis of abnormal hemoglobin (Hb). Examples include Hb S, Hb C, Hb D, and Hb E.
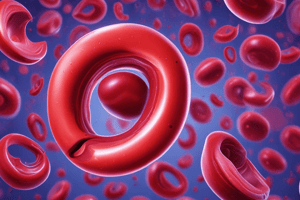
Sickle Cell Disease (SCD)
- SCD is a recessively inherited chronic hemolytic anemia.
- It results from a single nucleotide substitution in the β-globin gene (on chromosome 11, position 6).
- The substitution in the gene results in valine replacing glutamic acid in the beta-globin chain.
- This mutated hemoglobin (HbS) polymerizes under low-oxygen conditions.
- The polymerization causes red blood cells to change into a sickle (crescent) shape.
Pathophysiology of SCD
- Deoxygenation of HbS leads to K+ efflux, increasing cell density and dehydration, promoting polymerization.
- Sickled cells attach to endothelial cells, triggering vasoconstriction
- This creates a vicious cycle with reduced blood flow, hypoxia and acidosis, promoting further sickling.
- Some cells become irreversibly sickled.
- Severity of disease varies by individual and disease type.
- SS disease is the most severe.
- SC and S-beta thalº diseases result in intermediate severity.
- SA (one normal allele) is generally asymptomatic.
Factors Affecting Hb S Polymerization
- Decreased oxygen levels promote polymerization. intracellular HbS concentration (higher in SS than SC or S-thalassemia).
- Increased 2,3-DPG
- Decreased pH promotes polymerization
- Slowed transit time through the circulatory system, and
- Endothelial adhesion.
Factors Decreasing Hb S Polymerization
- Lower HbS concentration (e.g. compound heterozygosity for alpha thalassemia)
- Increased HbF levels. Genetic basis (e.g hydroxyurea) can contribute to increased HbF.
SCD and Malaria
- Children with sickle cell trait have a milder course of falciparum malaria. Children with SS disease have a more severe course, with a significant mortality rate.
Prognosis
- Median survival in developed countries (US, Europe) has improved significantly over the past 30 years in adults with SS disease (now 45-55 yrs).
- In Africa, approximately 50% of individuals with SS disease die before age 5.
- WHO estimates that SCD complicates up to 9% of under 5 deaths in West Africa.
Clinical Features of SCD
- Painful episodes
- Pneumococcal disease
- Acute chest syndrome
- Splenic infarction
- Splenic sequestration
- Stroke
- Osteonecrosis
- Priapism
- Retinopathy
- Leg ulcers
- Renal abnormalities (e.g osteopenia)
- Nutritional deficiencies
- Placental insufficiency
- Pulmonary hypertension
- Gallstones
Types of SCD Crises
- Painful crisis
- Sequestration crisis
- Acute chest syndrome
- Hemolytic crisis
- Aplastic crisis
Vaso-occlusive/Pain Crisis
- Occurs in approximately 60% of SS patients; tissue ischemia is the result of vaso-occlusion
- It can be triggered by infection, extremes of temperature, dehydration, or stress but usually without an identifiable cause.
- Characterized by severe, often painful episodes in extremities (long bones or abdomen) lasting from hours to days.
- Number of crises per year varies among individuals. Some individuals may experience constant low-level pain.
Infection (in SCD)
- Children with SCD often become asplenic by age 5 due to microinfarcts.
- Increased risk of infection with encapsulated organisms such as Streptococcus pneumoniae. The risk is approximately 400x higher than that for the general population
- Increased risk of osteomyelitis (bacterial bone infection) from Salmonella and Staphylococcus species.
Acute Chest Syndrome
- Characterized by new respiratory distress, pulmonary infiltrates (seen on X-ray), hypoxia (low O2), and/ or chest pain.
- Occurs in approximately 40% of patients with SS disease.
- Can rapidly progress to acute respiratory distress syndrome (ARDS)
- Potential causes include viral or bacterial infection, fat embolism from bone marrow infarction, unknown causes.
- Exchange transfusion is a treatment option.
Stroke
- Approximately 11% of SS patients will have a stroke by age 20, with peak incidence between age 2 and 10.
- Manifestations include focal neurologic deficit or seizure.
- Treatment involves transfusion.
Acute Splenic Sequestration
- Sudden enlargement of the spleen accompanied by a significant drop (more than 2 g/dL) in hemoglobin from baseline; often with thrombocytopenia.
- Typically occurs in children under 3 years old.
- Can lead to sudden circulatory collapse.
- Treatment involves immediate volume expansion, transfusions, and may require splenectomy if the episodes are frequent.
Aplastic Crisis
- Caused by viral infection (usually Parvovirus B19) or folate deficiency,
- Causing a suppression of red blood cell production.
- Characterized by fever, URI symptoms, and a drop in hemoglobin levels.
- RBC life expectancy in SS disease is 10–20 days, leading to significant reduction in red blood cell production.
- Bone marrow recovery is often within 7 to 10 days.
- Treatment involves transfusion if symptomatic.
Anemia
- Baseline anemia in SCD is often compensated.
- Baseline hemoglobin is typically 8-9 g/dL.
- Overtransfusion carries risks, including transmission of infections and iron overload.
- Treatment includes transfusion for hemoglobin levels below 5 g/dL or <6 g/dL, especially in cases of cardiac decompensation.
Other Complications
- Priapism (prolonged erection; may require surgical intervention or exchange transfusion)
- Dactylitis ( hand-foot syndrome, painful swelling in hands and feet, common in children)
- Avascular necrosis of humeral/femoral head
- Cholelithiasis (gallstones)
- Retinopathy
- Chronic leg ulcers
Treatment of SCD
- Opiates and hydration for painful crises
- Pneumococcal vaccination.
- Retinal surveillance.
- Transfusion for serious complications (e.g. stroke); exchange transfusions may be needed.
- Hydroxyurea.
- Stem cell transplant (in select cases).
Hydroxyurea Therapy
- Effective in some patients, especially those over 5 years of age with complications.
- Increases HbF, a type of hemoglobin less prone to polymerization,
- Decreases leukocytes, platelets, and reticulocytes to minimize inflammation and stress.
- Regular CBC monitoring is essential to assess for leukopenia (low white blood cell count).
Laboratory Findings and Diagnosis
- Hemolytic anemia characterized by low hemoglobin, elevated reticulocyte count, elevated LDH, and decreased haptoglobin.
- Peripheral blood smear reveals sickled cells.
- Sodium metabisulfite can be added to blood to stimulate sickling and confirm diagnosis.
- Hemoglobin electrophoresis differentiates between different types of hemoglobin abnormalities.
Hemoglobin C
- Glutamic acid in the beta chain is replaced by lysine at position six.
- HbC produces Hb that tends to crystallize.
- A homozygous state often presents with chronic hemolytic anemia.
- Compound heterozygosity with HbS produces a sickle cell phenotype.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.