Podcast
Questions and Answers
What is the primary function of hemodialysis in the body?
What is the primary function of hemodialysis in the body?
- To stimulate the production of red blood cells
- To increase the level of protein in the blood
- To enhance nutrient absorption in the intestines
- To remove electrolytes, waste products, and excess water (correct)
What mechanism allows small molecules to pass through the dialyzer membrane?
What mechanism allows small molecules to pass through the dialyzer membrane?
- Filtration
- Diffusion (correct)
- Active transport
- Osmosis
How are excess water and electrolytes removed during hemodialysis?
How are excess water and electrolytes removed during hemodialysis?
- By increasing the blood flow rate
- By adding more water to the dialysate
- By using pressure differential through ultrafiltration (correct)
- By lowering the temperature of the dialysate
What determines the direction of movement for substances across the dialyzer membrane?
What determines the direction of movement for substances across the dialyzer membrane?
What happens to serum proteins and blood cells during hemodialysis?
What happens to serum proteins and blood cells during hemodialysis?
What role do the porous membranes of the dialyzer play in hemodialysis?
What role do the porous membranes of the dialyzer play in hemodialysis?
How does the process of ultrafiltration work in hemodialysis?
How does the process of ultrafiltration work in hemodialysis?
What can be added to the dialysate if the blood lacks specific substances during hemodialysis?
What can be added to the dialysate if the blood lacks specific substances during hemodialysis?
Which statement about the composition of dialysate is incorrect?
Which statement about the composition of dialysate is incorrect?
What determines the concentration gradient that influences diffusion across the membrane in hemodialysis?
What determines the concentration gradient that influences diffusion across the membrane in hemodialysis?
What is the most common complication experienced by patients undergoing hemodialysis?
What is the most common complication experienced by patients undergoing hemodialysis?
Which condition would likely prevent a patient from undergoing hemodialysis?
Which condition would likely prevent a patient from undergoing hemodialysis?
What can be a result of altered platelet function during hemodialysis?
What can be a result of altered platelet function during hemodialysis?
Patients on chronic hemodialysis have an increased risk of which infections compared to the general population?
Patients on chronic hemodialysis have an increased risk of which infections compared to the general population?
What can local or systemic infections during hemodialysis be primarily attributed to?
What can local or systemic infections during hemodialysis be primarily attributed to?
What is the initial frequency of hemodialysis sessions for patients with AKI?
What is the initial frequency of hemodialysis sessions for patients with AKI?
What complication is most frequently associated with hemodialysis?
What complication is most frequently associated with hemodialysis?
Which factor may contribute to hypotension during hemodialysis?
Which factor may contribute to hypotension during hemodialysis?
What can result from the use of heparin during hemodialysis?
What can result from the use of heparin during hemodialysis?
Which infection is commonly associated with contamination of the vascular access site in hemodialysis patients?
Which infection is commonly associated with contamination of the vascular access site in hemodialysis patients?
What is a primary benefit of using Continuous Renal Replacement Therapy (CRRT) for patients with unstable cardiovascular status?
What is a primary benefit of using Continuous Renal Replacement Therapy (CRRT) for patients with unstable cardiovascular status?
What substances are effectively removed by CRRT during the therapy process?
What substances are effectively removed by CRRT during the therapy process?
In Continuous Renal Replacement Therapy, what method is primarily used to transport blood during the process?
In Continuous Renal Replacement Therapy, what method is primarily used to transport blood during the process?
Which fluid replacement solution is commonly used during Continuous Renal Replacement Therapy?
Which fluid replacement solution is commonly used during Continuous Renal Replacement Therapy?
How long can CRRT be performed for a patient requiring the therapy?
How long can CRRT be performed for a patient requiring the therapy?
What is the primary difference between continuous arteriovenous hemofiltration (CAVH) and continuous arteriovenous hemodialysis (CAVHD)?
What is the primary difference between continuous arteriovenous hemofiltration (CAVH) and continuous arteriovenous hemodialysis (CAVHD)?
Which type of continuous renal replacement therapy (CRRT) utilizes a double-lumen venous catheter?
Which type of continuous renal replacement therapy (CRRT) utilizes a double-lumen venous catheter?
What is essential for reducing the risk of infection at the vascular access sites during continuous renal replacement therapy?
What is essential for reducing the risk of infection at the vascular access sites during continuous renal replacement therapy?
Which statement about continuous arteriovenous hemodialysis (CAVHD) is accurate?
Which statement about continuous arteriovenous hemodialysis (CAVHD) is accurate?
In which setting is continuous renal replacement therapy typically performed?
In which setting is continuous renal replacement therapy typically performed?
Flashcards are hidden until you start studying
Study Notes
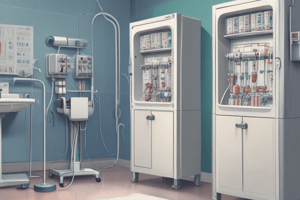
Hemodialysis
- Hemodialysis removes waste products, electrolytes, and excess water from the body.
- It relies on diffusion and ultrafiltration.
- Blood is taken from the patient and pumped to the dialyzer.
- The dialyzer has porous membranes that allow small molecules to pass through, but block larger molecules.
- Dialysate, a solution similar to normal extracellular fluid, flows on the other side of the membrane.
- Diffusion drives the movement of small solute molecules across the membrane, moving from higher concentration to lower.
- Waste products and electrolytes move from the blood into the dialysate due to concentration differences.
- Substances like calcium can be added to the dialysate to diffuse into the blood.
- Excess water is removed by ultrafiltration. This involves creating a higher hydrostatic pressure in the blood compared to the dialysate.
- The pressure gradient drives water from the blood into the dialysate.
Hemodialysis
- Hemodialysis is a process that relies on diffusion and ultrafiltration to remove waste products, electrolytes, and excess water from the body.
- Blood is taken from the patient through vascular access and pumped to the dialyzer.
- The dialyzer contains semi-permeable membranes that allow smaller molecules, like water, glucose, and electrolytes, to pass through, while blocking larger molecules, like serum proteins and blood cells.
- The dialysate, a solution with a composition and temperature similar to the extracellular fluid (ECF), flows on the other side of the membrane.
- Diffusion drives the movement of small solute molecules across the membrane, with the direction determined by concentration gradients between the blood and dialysate.
- Electrolytes and waste products, including urea and creatinine, diffuse from the blood into the dialysate.
- Calcium, or other required substances, can be added to the dialysate to diffuse into the blood.
- Ultrafiltration removes excess water by maintaining a higher hydrostatic pressure in the blood flow within the dialyzer compared to the dialysate, which flows in the opposite direction.
Hemodialysis for AKI
- Patients with AKI initially undergo daily hemodialysis, which may be reduced to three to four sessions per week as their condition improves.
- Hemodialysis is not used if the patient is hemodynamically unstable, such as experiencing hypotension or low cardiac output.
- Hypotension, the most frequent complication of hemodialysis, might result from fluid shifts, vasodilation, and other factors.
- Bleeding can be a complication due to altered platelet function from uremia and heparin usage during dialysis.
- Infection, both local and systemic, can occur due to damaged white blood cells and immune system suppression.
- Staphylococcus aureus septicemia is a common infection linked to vascular access site contamination.
- Chronic hemodialysis patients have higher rates of hepatitis B, hepatitis C, cytomegalovirus, and HIV infection compared to the general population.
AKI and Hemodialysis
- Patients with AKI typically undergo daily hemodialysis at the start of treatment.
- As their condition improves, they may switch to three to four hemodialysis sessions per week.
- Hemodialysis is not used for hemodynamically unstable patients (low blood pressure, or low heart output).
Complications of Hemodialysis
- Hypotension: Most common complication during hemodialysis.
- Result from changes in serum osmolality, rapid fluid removal from blood vessels, vasodilation, and other factors.
- Bleeding: May occur due to altered platelet function in individuals with uremia, and the use of heparin during dialysis.
- Infection (local or systemic): Can result from damaged white blood cells (WBCs) and weakened immune system.
- Staphylococcus aureus septicemia is often linked to vascular access site contamination.
- Patients on chronic hemodialysis are more likely to have hepatitis B, hepatitis C, cytomegalovirus, and HIV infection compared to the general population.
Continuous Renal Replacement Therapy (CRRT)
- CRRT is a form of dialysis that uses a highly porous hemofilter to remove excess water and solutes from the blood over a prolonged period (12 hours or more).
- CRRT is used for patients with acute kidney injury (AKI) who cannot tolerate hemodialysis due to unstable cardiovascular status, such as trauma, major surgery, or heart failure.
- CRRT removes excess fluids and solutes, including electrolytes, urea, creatinine, uric acid, and glucose.
- Fluid replacement during CRRT is typically done with normal saline or a balanced electrolyte solution.
- The slower fluid and solute removal in CRRT helps maintain hemodynamic stability and prevent complications caused by rapid changes in extracellular fluid (ECF) composition.
Continuous Renal Replacement Therapy (CRRT)
- CAVH (Continuous Arteriovenous Hemofiltration) removes fluid and some solutes using a hemofilter. Arterial blood circulates through the filter, then returns to the patient through a venous line. Ultrafiltrate collects in a drainage bag.
- CAVHD (Continuous Arteriovenous Hemodialysis) removes fluid and waste products using a hemofilter surrounded by dialysate. Arterial blood circulates through the filter, then returns to the patient via a venous line. Ultrafiltrate collects in a drainage bag.
- CVVHD (Continuous Venovenous Hemodialysis) removes fluid and waste products using a hemofilter surrounded by dialysate. Venous blood circulates through the filter, then returns to the patient through a double-lumen venous catheter. Ultrafiltrate collects in a drainage bag.
- CRRT is typically performed in an ICU or specialized nephrology unit.
- Some CRRT methods require both arterial and venous lines.
- Other CRRT methods utilize a double-lumen venous catheter.
- Aseptic technique is essential when caring for vascular access sites to minimize infection risk.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.