Podcast
Questions and Answers
What is the first-line treatment for heart failure with reduced cardiac function?
What is the first-line treatment for heart failure with reduced cardiac function?
- Ivabradine
- ACE inhibitor plus a beta blocker (correct)
- Digoxin
- Mineralocorticoid receptor antagonist
Beta blockers, such as Bisoprolol, Carvedilol, and Nebivolol, can increase heart rate and contractility.
Beta blockers, such as Bisoprolol, Carvedilol, and Nebivolol, can increase heart rate and contractility.
False (B)
What is the name of the study that showed Spironolactone improves survival in chronic heart failure?
What is the name of the study that showed Spironolactone improves survival in chronic heart failure?
RALES study
Spironolactone is a ______ that blocks the action of ______ on the collecting ducts.
Spironolactone is a ______ that blocks the action of ______ on the collecting ducts.
Match the following medications with their class:
Match the following medications with their class:
Which of the following are commonly used treatments for patients with heart failure?
Which of the following are commonly used treatments for patients with heart failure?
Verapamil is recommended as a treatment option for patients with chronic heart failure.
Verapamil is recommended as a treatment option for patients with chronic heart failure.
What are loop diuretics used for in chronic heart failure?
What are loop diuretics used for in chronic heart failure?
Loop diuretics act on the ______ limb of the loop of Henle.
Loop diuretics act on the ______ limb of the loop of Henle.
Match the following loop diuretics with their corresponding characteristics:
Match the following loop diuretics with their corresponding characteristics:
Which of these is NOT a side-effect of loop diuretics?
Which of these is NOT a side-effect of loop diuretics?
Loop diuretics are contraindicated in patients with severe hypokalemia and severe hyponatremia.
Loop diuretics are contraindicated in patients with severe hypokalemia and severe hyponatremia.
What is the main mechanism of action of loop diuretics?
What is the main mechanism of action of loop diuretics?
Ivabradine is effective in treating patients with atrial fibrillation.
Ivabradine is effective in treating patients with atrial fibrillation.
Sacubitril Valsartan is a combination of an ARB and a ______ that breaks down natriuretic peptides.
Sacubitril Valsartan is a combination of an ARB and a ______ that breaks down natriuretic peptides.
Which of the following is NOT a common side-effect of Hydralazine with Nitrate treatment?
Which of the following is NOT a common side-effect of Hydralazine with Nitrate treatment?
What is the primary mechanism of action of Digoxin in treating heart failure?
What is the primary mechanism of action of Digoxin in treating heart failure?
Match the following medications with their primary indications for use:
Match the following medications with their primary indications for use:
Which of these medications is indicated for patients with acute porphyria?
Which of these medications is indicated for patients with acute porphyria?
Ivabradine is a beta blocker.
Ivabradine is a beta blocker.
What are the common side-effects of Sacubitril Valsartan?
What are the common side-effects of Sacubitril Valsartan?
Flashcards
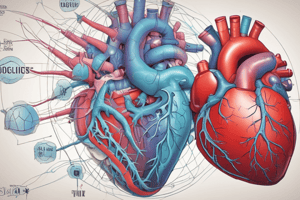
Heart Failure
Heart Failure
A condition where the heart's ability to pump blood is reduced, often leading to a decrease in ejection fraction.
ACE Inhibitor
ACE Inhibitor
First-line medication for heart failure that helps relax blood vessels and lower blood pressure.
Spironolactone
Spironolactone
An aldosterone antagonist used as add-on therapy in heart failure that retains potassium while promoting sodium and water loss.
Beta Blockers
Beta Blockers
Signup and view all the flashcards
Negative Ionotropic Effect
Negative Ionotropic Effect
Signup and view all the flashcards
Heart Failure Treatments
Heart Failure Treatments
Signup and view all the flashcards
Loop Diuretics
Loop Diuretics
Signup and view all the flashcards
Mechanism of Action of Loop Diuretics
Mechanism of Action of Loop Diuretics
Signup and view all the flashcards
Pharmacokinetics of Loop Diuretics
Pharmacokinetics of Loop Diuretics
Signup and view all the flashcards
Side Effects of Loop Diuretics
Side Effects of Loop Diuretics
Signup and view all the flashcards
Cautions for Loop Diuretics
Cautions for Loop Diuretics
Signup and view all the flashcards
Contraindications for Loop Diuretics
Contraindications for Loop Diuretics
Signup and view all the flashcards
Treatment of Heart Failure with Reduced Ejection Fraction
Treatment of Heart Failure with Reduced Ejection Fraction
Signup and view all the flashcards
Ivabradine
Ivabradine
Signup and view all the flashcards
Contraindications of Ivabradine
Contraindications of Ivabradine
Signup and view all the flashcards
Sacubitril Valsartan
Sacubitril Valsartan
Signup and view all the flashcards
Contraindications of Sacubitril Valsartan
Contraindications of Sacubitril Valsartan
Signup and view all the flashcards
Hydralazine with Nitrate
Hydralazine with Nitrate
Signup and view all the flashcards
Side Effects of Hydralazine with Nitrate
Side Effects of Hydralazine with Nitrate
Signup and view all the flashcards
Digoxin
Digoxin
Signup and view all the flashcards
Uses of Digoxin
Uses of Digoxin
Signup and view all the flashcards
Study Notes
Heart Failure Treatments
- Treatments for heart failure aim to improve cardiac output, reduce preload and afterload, and manage fluid retention.
- Vasodilators: Drugs that relax blood vessels, reducing the workload on the heart and improving cardiac output.
- ACE Inhibitors: These drugs reduce renin release, decrease angiotensin II formation, and lower aldosterone release. This helps regulate sodium and water balance, and reduces fluid retention.
- Diuretics: Medications that increase urine production, removing excess fluid from the body and reducing swelling (edema).
- Positive Inotropes: Drugs that increase the force of cardiac contractions, boosting heart output.
Chronic Heart Failure Treatment
- Fluid retention: If patients experience fluid retention, a loop diuretic is prescribed.
- Thrombosis risk: If a risk of blood clots exists, an anticoagulant (blood thinner) may be considered.
- Verapamil avoidance: Verapamil should be avoided as it blocks cardiac calcium channels.
Loop Diuretics
- Examples include furosemide, bumetanide, and torsemide.
- Used in pulmonary edema due to acute left ventricular failure, chronic heart failure, and resistant hypertension.
- Given intravenously for rapid relief of breathlessness and reducing preload.
Mechanism of Action of Loop Diuretics
- Reduce electrolyte reabsorption in the thick ascending limb of Henle's loop.
- Increase excretion of sodium, chloride, potassium, and water through Na+/K+/2Cl− transporters
- High ceiling effect producing potent diuresis.
- Oral administration with a peak effect at around 30 minutes and a half-life of around 2 hours. The duration of action is about 4 to 6 hours.
- IV administration provides faster effects, lasting around 10 minutes.
- Metabolized mainly by the liver (cytochrome P450).
- Excretes 20-25% of filtered sodium (potent effect).
Side Effects, Cautions, and Contraindications of Loop Diuretics
- Side effects: Dizziness, electrolyte imbalance (fatigue, headache, metabolic alkalosis, muscle spasms, nausea).
- Cautions: Risk of urinary retention in patients with an enlarged prostate.
- Cautions: Risk of hypovolemia (low blood volume), hypotension, and hypokalemia (low potassium). Use lower doses in elderly patients to reduce these risks.
- Contraindications: Anuria, drug-induced renal failure, severe hypokalemia, severe hyponatremia.
Heart Failure with Reduced Ejection Fraction (HFrEF) Treatment
- First line treatment involves ACE inhibitors plus a beta-blocker.
- If symptoms persist, add a mineralocorticoid receptor antagonist (e.g., spironolactone).
- Additional treatments may include ivabradine, digoxin, SGLT2 inhibitors (such as dapagliflozin), sacubitril/valsartan, and hydralazine with nitrate.
Beta-Blockers (e.g., Bisoprolol, Carvedilol, Nebivolol)
- Inhibit beta-1 receptors, reducing adrenaline/noradrenaline effects.
- Slows heart rate, reduces cardiac contraction.
- Common side effects: dizziness, tiredness, blurred vision.
- Start treatment at a low dose and gradually increase for optimal effect.
Spironolactone
- An aldosterone antagonist, used as an add-on therapy for heart failure when first-line treatments aren't sufficient.
- Improves survival in heart failure patients.
- Contraindicated if hyperkalemia or renal impairment exists.
- Steroid pro-drug with effects via canrenone (longer half-life).
- Blocks aldosterone action, reducing sodium and water retention, and increasing potassium retention.
A K+ sparing diuretic; useful in conjunction with loop or thiazide diuretics.
Ivabradine
- Used to treat angina and mild-to-moderate chronic heart failure.
- Inhibits cardiac pacemaker activity.
- A useful alternative alongside or instead of beta blockers.
- Contraindications include MI, cardiogenic shock, heart blocks, and slow heart rates.
Sacubitril/Valsartan
- Combination of an angiotensin receptor-neprilysin inhibitor (ARNI).
- Used in patients who cannot take ACEIs.
- Reduce blood pressure (avoid if systolic BP <100 mmHg).
- Common side effects: anaemia, cough, diarrhoea, dizziness, electrolyte imbalance, headache, hypotension, syncope, vertigo, renal impairment, nausea.
Hydralazine with Nitrate
- Used for patients intolerant to both ACE inhibitors & ARBs.
- Venodilator, reducing preload (pulmonary congestion).
- Arterial vasodilator, increasing stroke volume.
- Contraindications: porphyrias, severe cor pulmonale, dissecting aortic aneurysms, tachycardia
Digoxin
- Positive inotrope, increasing the force of heart contractions to treat heart failure.
- Blocks Na+/K+ ATPase which increases Ca++ levels in myocardial cells, ultimately increasing the force of contraction.
- Indications include chronic heart failure, supraventricular arrhythmias, and chronic atrial fibrillation.
Digoxin Pharmacokinetics, Contraindications & Cautions
-
Orally administered, ~75% bioavailability, peak effect in 1-5 hours (IV), Half-life ~36 hours.
-
Narrow therapeutic range: Risk of toxicity.
-
Common side effects: Arrhythmias, Cardiac conduction problems, Impairment, dizziness, diarrhoea, nausea, skin reactions, vision disorders, vomiting
-
Cautions: Electrolyte imbalances, recent myocardial infarction.
SGLT2 Inhibitors (e.g., Dapagliflozin)
-
Used in type 2 diabetes and heart failure.
-
Mechanism blocks SGLT2, increasing glucose excretion in urine (glucosuria).
-
Reduced fluid and sodium retention, decreasing blood pressure
-
Improved pre-load and afterload, reducing cardiac workload.
-
Rare serious ketoacidosis is a potential side effect in some patients.
-
Contraindicated in diabetic ketoacidosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.