Podcast
Questions and Answers
What is the role of tissue plasminogen activator (tPA) in blood clot management?
What is the role of tissue plasminogen activator (tPA) in blood clot management?
- It activates plasminogen into plasmin. (correct)
- It stabilizes the blood clot after formation.
- It prevents fibrinogen from converting to fibrin.
- It directly cleaves thrombin to inhibit clotting.
Which of the following is considered an endogenous inhibitor of primary haemostasis?
Which of the following is considered an endogenous inhibitor of primary haemostasis?
- Antithrombin III
- Activated protein C
- Nitric oxide (correct)
- Tissue factor pathway inhibitor (TFPI)
What does the breakdown of fibrin lead to in the process of fibrinolysis?
What does the breakdown of fibrin lead to in the process of fibrinolysis?
- Stabilization of fibrinogen
- Activation of thrombin
- Formation of tissue factor
- Generation of d-dimer fragments (correct)
How does thrombin contribute to the haemostasis process?
How does thrombin contribute to the haemostasis process?
Which statement correctly describes the role of Antithrombin III?
Which statement correctly describes the role of Antithrombin III?
What initiates secondary haemostasis?
What initiates secondary haemostasis?
Which of the following is a key function of thrombin in secondary haemostasis?
Which of the following is a key function of thrombin in secondary haemostasis?
What role do proenzymes play in secondary haemostasis?
What role do proenzymes play in secondary haemostasis?
Which factors are Vitamin K-dependent for their synthesis?
Which factors are Vitamin K-dependent for their synthesis?
What is the purpose of activated platelets expressing phospholipid complexes?
What is the purpose of activated platelets expressing phospholipid complexes?
What occurs during the second stage of secondary haemostasis?
What occurs during the second stage of secondary haemostasis?
Which statement correctly describes the overall process of secondary haemostasis?
Which statement correctly describes the overall process of secondary haemostasis?
What initiates the extrinsic pathway of coagulation?
What initiates the extrinsic pathway of coagulation?
Which protein is activated when tissue factor binds to FVII?
Which protein is activated when tissue factor binds to FVII?
What role does FXa play in the common pathway of coagulation?
What role does FXa play in the common pathway of coagulation?
Which of the following is NOT involved in the intrinsic pathway?
Which of the following is NOT involved in the intrinsic pathway?
How is FIX activated in the intrinsic pathway?
How is FIX activated in the intrinsic pathway?
Which substance plays an important role in primary hemostasis related to the intrinsic pathway?
Which substance plays an important role in primary hemostasis related to the intrinsic pathway?
What is the final product of the extrinsic pathway leading to the common pathway?
What is the final product of the extrinsic pathway leading to the common pathway?
What is the activation product of FX and FVa in the common pathway?
What is the activation product of FX and FVa in the common pathway?
Which cell types primarily express tissue factor during the initiation of the extrinsic pathway?
Which cell types primarily express tissue factor during the initiation of the extrinsic pathway?
What component is crucial for the activation of FIX in the common pathway?
What component is crucial for the activation of FIX in the common pathway?
Flashcards
Tissue Factor Release
Tissue Factor Release
The initial step in secondary haemostasis, where injured tissue releases tissue factor (TF), initiating the extrinsic pathway.
Phospholipid Complex Exposure
Phospholipid Complex Exposure
Activated platelets expose phospholipid complexes with a negative charge, allowing coagulation factors to bind and activate.
Prothrombin to Thrombin Conversion
Prothrombin to Thrombin Conversion
The conversion of prothrombin (Factor II) to thrombin (Factor IIa), a crucial step in the coagulation cascade.
Fibrinogen to Fibrin Conversion
Fibrinogen to Fibrin Conversion
Signup and view all the flashcards
Coagulation Cascade
Coagulation Cascade
Signup and view all the flashcards
Extrinsic Pathway
Extrinsic Pathway
Signup and view all the flashcards
Intrinsic Pathway
Intrinsic Pathway
Signup and view all the flashcards
What is plasminogen?
What is plasminogen?
Signup and view all the flashcards
What is fibrinolysis?
What is fibrinolysis?
Signup and view all the flashcards
What is a d-dimer?
What is a d-dimer?
Signup and view all the flashcards
What is nitric oxide?
What is nitric oxide?
Signup and view all the flashcards
What is antithrombin III?
What is antithrombin III?
Signup and view all the flashcards
Common Pathway
Common Pathway
Signup and view all the flashcards
Tissue Factor (TF)
Tissue Factor (TF)
Signup and view all the flashcards
Factor IXa (FIXa)
Factor IXa (FIXa)
Signup and view all the flashcards
Factor Xa (FXa)
Factor Xa (FXa)
Signup and view all the flashcards
Thrombin (Factor IIa)
Thrombin (Factor IIa)
Signup and view all the flashcards
Factor Va (FVa)
Factor Va (FVa)
Signup and view all the flashcards
Factor VIII (FVIII)
Factor VIII (FVIII)
Signup and view all the flashcards
Factor XI (FXI)
Factor XI (FXI)
Signup and view all the flashcards
Study Notes
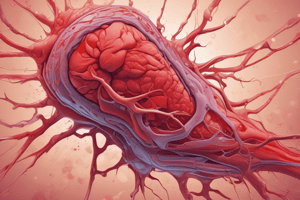
Haemostasis - Part II: Secondary Haemostasis
- Secondary haemostasis is a crucial part of the overall haemostasis process, following primary haemostasis. It strengthens the initial platelet plug.
- Secondary haemostasis involves a cascade of coagulation factors.
- Coagulation factors are primarily proenzymes (zymogens), requiring activation to function.
- Several coagulation factors (Factors II, VII, IX, and X) are vitamin K-dependent and synthesised in the liver.
- The active form of a coagulation factor is denoted with an 'a' suffix (e.g., FVIIa).
Preparation for the Lecture
- Students need to have completed the previous lecture on Haemostasis Part I.
- Students should prepare a written out summary/diagram of the pathways. The method of presentation should help the student to best understand the pathways.
- Students need to understand the importance of the previous lecture to the current topic, which is Secondary Haemostasis.
- Caffeine is shown as a visual aid in the presentation.
Aims and Objectives
- The lecture aims to outline the processes in normal haemostasis.
- The learner will be able to explain the significance of effective haemostasis.
- Learners will describe the key components of haemostatic mechanisms.
- Learners will illustrate how secondary haemostasis works.
Primary and Secondary Haemostasis
- Primary haemostasis involves platelet activation, adhering to the vessel wall and forming a plug.
- Secondary haemostasis:
- Involves activation of intrinsic and extrinsic coagulation pathways.
- Activates the common pathway.
- Forms a fibrin strand to strengthen the platelet plug.
- All phases of haemostasis are interconnected and often occur simultaneously.
Secondary Haemostasis Details
- A weak platelet plug needs strengthening by the coagulation factors of secondary haemostasis.
- Most coagulation factors are proenzymes (zymogens) synthesised in the liver.
- Vitamin K dependent factors (II, VII, IX, and X) are vital to the process.
- Proenzymes need activation to do their job.
Secondary Haemostasis - Four Stage Process
- Secondary haemostasis occurs in a four-stage process:
- Tissue factor expression or release.
- Activated platelets form phospholipid complexes, where coagulation factors bind and become activated.
- Prothrombin converts to thrombin.
- Fibrinogen converts to fibrin.
The Coagulation Cascade
- The coagulation cascade includes three pathways:
- Extrinsic pathway.
- Intrinsic pathway.
- Common pathway.
- These pathways are essential in understanding how medicines that prevent blood clots function. Also vital to understand in-vitro diagnostic tests.
Extrinsic Pathway
- The extrinsic pathway is initiated by vascular injury, for example; physical injury, inflammation, and atherosclerotic plaques.
- Tissue factor (TF) is exposed following the initiation.
- TF binds to FVII, activating it to FVIIa.
- TF-FVIIa complex then activates factor X (FX), initiating the common pathway.
Intrinsic Pathway
- The intrinsic pathway is initiated by contact with negatively charged surfaces. This includes subendothelial matrix, collagen and negatively charged phospholipids on platelets.
- Contact with these surfaces activate factor XII (FXII).
- A series of activations occurs through factors XI, IX, VIII, and eventually activate factor X.
Common Pathway
- FXa, along with factor Va and calcium ions, activate prothrombin (Factor II).
- Prothrombin converts into thrombin (Factor IIa).
- Thrombin catalyzes the conversion of fibrinogen to fibrin.
- Fibrin and activated platelets create a thrombus (blood clot).
- The clot is stable and strengthened.
What Happens to the Clot Afterwards?
- When the injury heals, the clot is broken down by fibrinolysis.
- Tissue plasminogen activator (tPA) is released by endothelial cells.
- tPA converts plasminogen to plasmin.
- Plasmin breaks down fibrin into small fragments (d-dimers)
Why Don't We Get Clots All The Time?
- Haemostasis is tightly regulated.
- The intrinsic and extrinsic pathways lead to thrombin generation, activating platelets.
- Endogenous inhibitors prevent excessive clotting.
- Nitric oxide and prostacyclin are produced by endothelial cells, inhibiting platelet activity.
- Endogenous inhibitors of secondary haemostasis include:
- Tissue factor pathway inhibitor (TFPI).
- Antithrombin III.
- Protein C.
Summary
- Secondary haemostasis is divided into extrinsic, intrinsic, and common pathways.
- Clotting factors work in a cascade to generate a fibrin clot.
- Fibrin and activated platelets create a thrombus.
- The thrombus is broken down by plasmin, creating d-dimers.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.