Podcast
Questions and Answers
What is the structure of a haemoglobin molecule?
What is the structure of a haemoglobin molecule?
- Six polypeptide chains, each bound to two haem groups
- Two polypeptide chains and one haem group
- Four polypeptide chains, each bound to a haem group (correct)
- Four polypeptide chains and a single haem group
How many binding sites does the iron atom in haemoglobin have?
How many binding sites does the iron atom in haemoglobin have?
- 5 binding sites
- 6 binding sites (correct)
- 4 binding sites
- 7 binding sites
Which statement best describes the concept of co-operative binding in haemoglobin?
Which statement best describes the concept of co-operative binding in haemoglobin?
- Haemoglobin can only bind oxygen when it is not bound to carbon dioxide
- The binding of one oxygen molecule increases the affinity of haemoglobin for additional oxygen molecules (correct)
- One oxygen molecule binds and reduces the affinity for more oxygen
- All haemoglobin molecules bind oxygen at the same time without any interaction
What role does iron play in the haemoglobin structure?
What role does iron play in the haemoglobin structure?
What are the components bound to each haem group in haemoglobin?
What are the components bound to each haem group in haemoglobin?
What is considered a normal haemoglobin level for women according to the World Health Organization?
What is considered a normal haemoglobin level for women according to the World Health Organization?
What type of haemoglobinopathy is caused by absent or decreased production of globin chains?
What type of haemoglobinopathy is caused by absent or decreased production of globin chains?
Which of the following symptoms is commonly associated with sickle cell disease when experiencing a sickling event?
Which of the following symptoms is commonly associated with sickle cell disease when experiencing a sickling event?
How does haemoglobin S differ from normal haemoglobin?
How does haemoglobin S differ from normal haemoglobin?
What is a potential genetic advantage conferred by the sickle cell trait?
What is a potential genetic advantage conferred by the sickle cell trait?
What can cause the red blood cells in sickle cell disease to obstruct blood flow?
What can cause the red blood cells in sickle cell disease to obstruct blood flow?
What laboratory finding is below the normal reference range for mean corpuscular volume (MCV) in the case presented?
What laboratory finding is below the normal reference range for mean corpuscular volume (MCV) in the case presented?
What is the role of haemoglobin in oxygen transport?
What is the role of haemoglobin in oxygen transport?
What is the oxygen saturation of normal arterial blood?
What is the oxygen saturation of normal arterial blood?
Which statement about the binding of oxygen to haemoglobin is true?
Which statement about the binding of oxygen to haemoglobin is true?
What is the primary type of haemoglobin in adults?
What is the primary type of haemoglobin in adults?
Which type of haemoglobin has a greater affinity for oxygen than Haemoglobin A?
Which type of haemoglobin has a greater affinity for oxygen than Haemoglobin A?
What is the composition of normal adult haemoglobin A (HbA)?
What is the composition of normal adult haemoglobin A (HbA)?
Which embryonic haemoglobin is commonly found at birth?
Which embryonic haemoglobin is commonly found at birth?
How much oxygen can 1g of haemoglobin carry?
How much oxygen can 1g of haemoglobin carry?
Flashcards
Haemoglobin Structure
Haemoglobin Structure
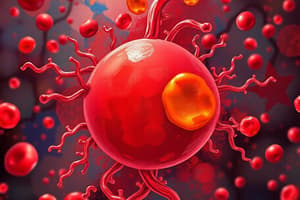
Haemoglobin, a protein in red blood cells, consists of four polypeptide chains, each one attached to a ring-shaped heme group. At the center of each heme is an iron atom.
Iron in Haemoglobin
Iron in Haemoglobin
The iron atom in the heme group of haemoglobin has six binding sites. Oxygen binds to the sixth site.
Haemoglobin Function
Haemoglobin Function
Haemoglobin's primary function is to transport oxygen throughout the body. It binds oxygen in the lungs and releases it in tissues.
Co-operative Binding
Co-operative Binding
Signup and view all the flashcards
Anaemia
Anaemia
Signup and view all the flashcards
Oxyhaemoglobin
Oxyhaemoglobin
Signup and view all the flashcards
Deoxyhaemoglobin
Deoxyhaemoglobin
Signup and view all the flashcards
O2 Saturation
O2 Saturation
Signup and view all the flashcards
Haemoglobin A (HbA)
Haemoglobin A (HbA)
Signup and view all the flashcards
Haemoglobin A2 (HbA2)
Haemoglobin A2 (HbA2)
Signup and view all the flashcards
Foetal Haemoglobin (HbF)
Foetal Haemoglobin (HbF)
Signup and view all the flashcards
Embryonic Haemoglobins
Embryonic Haemoglobins
Signup and view all the flashcards
What is anaemia?
What is anaemia?
Signup and view all the flashcards
What are the normal haemoglobin levels?
What are the normal haemoglobin levels?
Signup and view all the flashcards
What are haemoglobinopathies?
What are haemoglobinopathies?
Signup and view all the flashcards
What is sickle cell anaemia?
What is sickle cell anaemia?
Signup and view all the flashcards
What is the significance of the MCV (Mean Corpuscular Volume) in blood tests?
What is the significance of the MCV (Mean Corpuscular Volume) in blood tests?
Signup and view all the flashcards
What is the role of serum ferritin in diagnosing anaemia?
What is the role of serum ferritin in diagnosing anaemia?
Signup and view all the flashcards
What are some symptoms of anaemia?
What are some symptoms of anaemia?
Signup and view all the flashcards
What is the significance of the Hb level (haemoglobin level) in a blood test?
What is the significance of the Hb level (haemoglobin level) in a blood test?
Signup and view all the flashcards
Study Notes
Haemoglobin Lecture Notes
- Haemoglobin has a structure allowing it to load and unload oxygen
- Different types of haemoglobin exist, including:
- Haemoglobin A (HbA): 95-98% in adults, with two alpha and two beta chains (α₂β₂)
- Haemoglobin A2 (HbA₂): 1.5-3% in adults, with two alpha and two delta chains (α₂δ₂)
- Fetal haemoglobin (HbF): present at birth, at 0-0.5% in adults, with two alpha and two gamma chains (α₂γ₂). Has greater affinity for oxygen than HbA, which facilitates oxygen transfer from mother to foetus.
- Haemoglobin abnormalities can cause anaemia and reduced oxygen-carrying capacity in the blood due to insufficient or malformed haemoglobin. Examples include thalassemias (reduced or absent alpha or beta chains) and haemoglobinopathies (abnormal polypeptide chains like haemoglobin C, E, I, J, S).
- Haemoglobin S (sickle cell haemoglobin) results from a single amino acid substitution (valine for glutamic acid) in beta globin chains. Low oxygen causes the haemoglobin to change shape, causing cells to become stiff and deformed, clogging blood vessels, leading to pain and anaemia.
Haemoglobin Breakdown
- Old or damaged red blood cells (RBCs) are broken down by macrophages within the spleen.
- Haemoglobin is broken into haemoglobin and globin components.
- Globin is reused or broken down to amino acids.
- Haem molecules are broken down first into biliverdin then bilirubin.
- Iron is reused in haemoglobin synthesis
- Bilirubin is carried by albumin from the spleen to the liver and metabolised there, in the production of bile.
- Bilirubin buildup results in jaundice (yellowing skin and eyes).
Haemoglobin Levels and Anaemia
- The World Health Organization defines anaemia by haemoglobin levels below:
- 7.7 mmol/L (13 g/dL) in men
- 7.4 mmol/L (12 g/dL) in women.
- Abnormally low red blood cell count or haemoglobin concentration can also indicate anaemia.
Laboratory Test Results:
- Specific lab results were reported
-RBC count
-HGB / haemoglobin level
-HCT / haematocrit
-MCV / mean corpuscular volume
-MCH / mean corpuscular haemoglobin
-MCHC / mean corpuscular haemoglobin concentration
-WBC count
-Differential white blood cell count components (e.g., neutrophils, lymphocytes, monocytes, eosinophils, basophils)
- Platelets (PLT) -Serum iron -Total iron binding capacity (TIBC) -Serum Ferritin -Transferrin saturation
- Specific examples of results from a patient case were included.
Recommended Textbooks for Immunology
- Basic Immunology: Functions and Disorders of the Immune System by Abbas, Abul K., Andrew H. Lichtman, Shiv Pillai, and David L. Baker (7th ed., 2024, Elsevier)
- Immunology for Medical Students by Helbert, Matthew, and Roderick Nairn (3rd ed., 2017, Elsevier)
Other Important Points
- Co-operative binding: Binding of one oxygen molecule to haemoglobin causes a conformational change in the neighbouring polypeptide chains, increasing the affinity of the haemoglobin for further oxygen molecules.
- Oxygen uptake and release.
- Normal developmental profile of haemoglobins. This displays the relative percentage of different types of haemoglobin (Hb) throughout development from fetus to newborn.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.