Podcast
Questions and Answers
Which of the following describes a congenital abnormality characterized by an absence in the oesophagus?
Which of the following describes a congenital abnormality characterized by an absence in the oesophagus?
- Agenesis (correct)
- Motor dysfunction
- Fistula
- Atresia
What is the condition wherein the oesophagus is replaced by a thin, non-canalized cord?
What is the condition wherein the oesophagus is replaced by a thin, non-canalized cord?
- Fistula
- Agenesis
- Barrett’s oesophagus
- Atresia (correct)
Which of the following is NOT commonly associated with oesophagitis?
Which of the following is NOT commonly associated with oesophagitis?
- Haematemesis
- Dysphagia
- Heart burn
- Constipation (correct)
Tracheo-oesophageal fistula (TOF) is primarily related to which of the following malformations?
Tracheo-oesophageal fistula (TOF) is primarily related to which of the following malformations?
Which of the following is a clinical feature of tumours in the oesophagus?
Which of the following is a clinical feature of tumours in the oesophagus?
Barrett’s oesophagus is primarily associated with which pathological process?
Barrett’s oesophagus is primarily associated with which pathological process?
What is the typical morphology of a peptic ulcer based on macroscopic description?
What is the typical morphology of a peptic ulcer based on macroscopic description?
Which tissue characteristics are commonly seen in the adjacent mucosa of a peptic ulcer?
Which tissue characteristics are commonly seen in the adjacent mucosa of a peptic ulcer?
Which of the following is NOT a complication associated with peptic ulcers?
Which of the following is NOT a complication associated with peptic ulcers?
What percentage of patients with peptic ulcers typically experience bleeding as a complication?
What percentage of patients with peptic ulcers typically experience bleeding as a complication?
What is one of the potential consequences of pyloric channel ulcers?
What is one of the potential consequences of pyloric channel ulcers?
What is a common microscopic finding in a peptic ulcer?
What is a common microscopic finding in a peptic ulcer?
What is a significant characteristic of linitis plastica in gastric carcinoma?
What is a significant characteristic of linitis plastica in gastric carcinoma?
Which subtype of gastric carcinoma is known for not forming glands?
Which subtype of gastric carcinoma is known for not forming glands?
Which of the following is a typical demographic characteristic of the intestinal type of gastric carcinoma?
Which of the following is a typical demographic characteristic of the intestinal type of gastric carcinoma?
What is the 5-year survival rate for early gastric carcinoma?
What is the 5-year survival rate for early gastric carcinoma?
Which condition is associated with the presence of Helicobacter pylori?
Which condition is associated with the presence of Helicobacter pylori?
Which of the following is a common site for distant lymph node metastasis in gastric carcinoma?
Which of the following is a common site for distant lymph node metastasis in gastric carcinoma?
What type of cell is associated with diffuse type gastric carcinoma?
What type of cell is associated with diffuse type gastric carcinoma?
Which of the following statements about gastric carcinoma is true?
Which of the following statements about gastric carcinoma is true?
What is the role of spindle cells in gastrointestinal stromal tumors (GIST)?
What is the role of spindle cells in gastrointestinal stromal tumors (GIST)?
Which type of gastric carcinoma does not involve a specific precursor lesion?
Which type of gastric carcinoma does not involve a specific precursor lesion?
What is the primary consequence of a defect in MTP?
What is the primary consequence of a defect in MTP?
Which characteristic is associated with Whipple disease?
Which characteristic is associated with Whipple disease?
What is a common symptom of lipid malabsorption?
What is a common symptom of lipid malabsorption?
What is the primary infectious agent involved in Whipple disease?
What is the primary infectious agent involved in Whipple disease?
Which abnormality is associated with Whipple disease morphology?
Which abnormality is associated with Whipple disease morphology?
What mechanism underlies appendicitis?
What mechanism underlies appendicitis?
Which of the following is a systemic effect of Whipple disease?
Which of the following is a systemic effect of Whipple disease?
What is the effect of MTP deficiency on vitamin absorption?
What is the effect of MTP deficiency on vitamin absorption?
What characterizes Crohn disease in terms of lesions?
What characterizes Crohn disease in terms of lesions?
Which factor is NOT associated with increased risk for Crohn disease?
Which factor is NOT associated with increased risk for Crohn disease?
What is a key microscopic feature observed in Crohn disease?
What is a key microscopic feature observed in Crohn disease?
Which of the following statements about ulcerative colitis is true?
Which of the following statements about ulcerative colitis is true?
Which of the following clinical features is associated with ulcerative colitis?
Which of the following clinical features is associated with ulcerative colitis?
What is a common complication of Crohn disease?
What is a common complication of Crohn disease?
Which feature is a distinguishable characteristic of Crohn disease compared to ulcerative colitis?
Which feature is a distinguishable characteristic of Crohn disease compared to ulcerative colitis?
Which histological change is typically not seen in ulcerative colitis?
Which histological change is typically not seen in ulcerative colitis?
Which of the following best describes the epidemiology of Crohn disease?
Which of the following best describes the epidemiology of Crohn disease?
What type of inflammatory response is unregulated in individuals with inflammatory bowel disease?
What type of inflammatory response is unregulated in individuals with inflammatory bowel disease?
Flashcards are hidden until you start studying
Study Notes
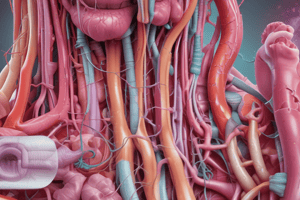
Gastrointestinal Tract Overview
- Objectives include understanding congenital abnormalities, symptoms, motor dysfunctions, and causes of oesophagitis.
- Clinical features of oesophagitis include heartburn, dysphagia, pain, and haematemesis.
Congenital Abnormalities of the Oesophagus
- Agenesis: Complete absence of the oesophagus.
- Atresia: Present as a thin, non-canalized cord.
- Tracheoesophageal Fistula (TOF): Connection of oesophagus with the trachea, often associated with cardiovascular, gastrointestinal, or central nervous system anomalies.
Oesophagitis
- Common causes include hyperacidity, medications like corticosteroids, and inflammation.
- Pathogenesis involves mucosal damage leading to symptoms such as dysphagia and heartburn.
Morphology of Peptic Ulcers
- Macroscopic features: Round to oval punched-out defects with smooth, clean bases and even margins.
- Microscopic features: Necrotic debris, inflammatory cells, scarring, adjacent red, and oedematous mucosa.
Complications of Peptic Ulcers
- Potential complications include bleeding (15-20%), perforation (5%), obstruction (2%), and iron deficiency anemia.
- Occurrence of pyloric channel and duodenal ulcers is significant.
Gastric Carcinoma Overview
- Two main types: Intestinal type (higher incidence, associated with precursor lesions) and Diffuse type (no precursor lesions, more common in younger patients).
- Histology distinguishes between adenocarcinoma subtypes: intestinal (neoplastic glands) and diffuse (individual cells infiltrating).
Prognosis of Gastric Carcinoma
- Five-year survival rates vary significantly: 90-95% for early detection, 15% for advanced stages.
- Common spread includes regional and distant lymph nodes, liver, and peritoneum.
Inflammatory Bowel Disease (IBD)
- IBD encompasses Crohn's disease and ulcerative colitis, characterized by chronic inflammation and relapsing symptoms.
- Strong immune response against normal gut flora with genetic predisposition affecting roughly 15-50% of patients.
Crohn's Disease
- Can affect any part of the gastrointestinal tract; common symptoms include mild diarrhea, abdominal pain, and weight loss.
- Characterized by “skip lesions” and transmural inflammation presenting with granulomas and strictures.
Ulcerative Colitis
- Limited to colon and rectum, progresses continuously without skip lesions.
- Symptoms include bloody mucoid diarrhea and lower abdominal pain. An extraintestinal disorder with systemic effects.
Common Complications and Features
- Granulomas in Crohn’s disease can lead to serious complications like fistulas, strictures, and protein-losing enteropathy.
- Unique features of ulcerative colitis include pseudo polyps and the potential for spread to the distal ileum.
Whipple Disease
- Rare systemic infection caused by Tropheryma whippelii, resulting in malabsorption and systemic symptoms.
- Histological characteristics include foamy macrophages in the lamina propria.
Appendicitis
- Characterized by acute inflammation of the appendix, often due to increased luminal pressure and potential obstruction.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.