Podcast
Questions and Answers
Which area is more commonly affected by Crohn disease?
Which area is more commonly affected by Crohn disease?
- Rectum
- Terminal ileum (correct)
- Colon
- Duodenum
What type of stool characteristic is associated with ulcerative colitis?
What type of stool characteristic is associated with ulcerative colitis?
- Hard and pellet-like
- Loose, semiformed
- Frequent, watery with blood and mucus (correct)
- Thick and foul-smelling
Which of the following symptoms is common to both Crohn disease and ulcerative colitis?
Which of the following symptoms is common to both Crohn disease and ulcerative colitis?
- Fistula formation
- Bloody diarrhea (correct)
- Villus atrophy
- Strictures
What is a common diagnostic test for evaluating inflammation in suspected inflammatory bowel disease?
What is a common diagnostic test for evaluating inflammation in suspected inflammatory bowel disease?
Which characteristic is NOT associated with Crohn disease?
Which characteristic is NOT associated with Crohn disease?
Which serological test is considered the gold standard for diagnosing celiac disease?
Which serological test is considered the gold standard for diagnosing celiac disease?
What is a distinguishing feature of ulcerative colitis in terms of lesion distribution?
What is a distinguishing feature of ulcerative colitis in terms of lesion distribution?
What type of diet is necessary for managing celiac disease?
What type of diet is necessary for managing celiac disease?
What is a characteristic of the pylori antigen test?
What is a characteristic of the pylori antigen test?
Which statement accurately describes Zollinger-Ellison Syndrome?
Which statement accurately describes Zollinger-Ellison Syndrome?
Which of the following tests is NOT commonly used in the diagnosis of Malabsorption Syndrome?
Which of the following tests is NOT commonly used in the diagnosis of Malabsorption Syndrome?
What is the diagnostic criteria for gastrinoma associated with Zollinger-Ellison Syndrome?
What is the diagnostic criteria for gastrinoma associated with Zollinger-Ellison Syndrome?
Which symptom is commonly associated with malabsorption syndrome?
Which symptom is commonly associated with malabsorption syndrome?
Which of the following is NOT a cause of chronic diarrhea?
Which of the following is NOT a cause of chronic diarrhea?
Which laboratory test is useful for differentiating between maldigestion and malabsorption?
Which laboratory test is useful for differentiating between maldigestion and malabsorption?
What type of diarrhea is characterized by loose, watery stools lasting more than four weeks?
What type of diarrhea is characterized by loose, watery stools lasting more than four weeks?
What is the primary role of cholecystokinin in the gastrointestinal tract?
What is the primary role of cholecystokinin in the gastrointestinal tract?
Which part of the gastrointestinal tract is primarily responsible for the completion of protein digestion?
Which part of the gastrointestinal tract is primarily responsible for the completion of protein digestion?
What is the significance of the urea breath test in diagnosing H. pylori infections?
What is the significance of the urea breath test in diagnosing H. pylori infections?
Which nutrient category is primarily digested in the oral cavity?
Which nutrient category is primarily digested in the oral cavity?
Which laboratory test is considered most widely used for detecting active infections of H. pylori?
Which laboratory test is considered most widely used for detecting active infections of H. pylori?
What is a common cause of duodenal and gastric ulcers?
What is a common cause of duodenal and gastric ulcers?
Which of the following components is NOT part of the upper gastrointestinal tract?
Which of the following components is NOT part of the upper gastrointestinal tract?
What can trigger the inflammatory process leading to peptic ulcers?
What can trigger the inflammatory process leading to peptic ulcers?
Flashcards
Digestion
Digestion
The process of breaking down food into smaller molecules that can be absorbed by the body.
Upper GI tract
Upper GI tract
The part of the digestive system that includes the mouth, esophagus, stomach, and small intestine.
Lower GI tract
Lower GI tract
The part of the digestive system that includes the large intestine, rectum, and anus.
Peptic ulcer
Peptic ulcer
Signup and view all the flashcards
Helicobacter pylori
Helicobacter pylori
Signup and view all the flashcards
Urea breath test
Urea breath test
Signup and view all the flashcards
Gastroscopy
Gastroscopy
Signup and view all the flashcards
Stool antigen test
Stool antigen test
Signup and view all the flashcards
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD)
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Celiac Disease
Celiac Disease
Signup and view all the flashcards
Villi
Villi
Signup and view all the flashcards
Biopsy
Biopsy
Signup and view all the flashcards
IgA-antitissue transglutaminase antibody (tTG)
IgA-antitissue transglutaminase antibody (tTG)
Signup and view all the flashcards
Endoscopy
Endoscopy
Signup and view all the flashcards
Zollinger-Ellison Syndrome
Zollinger-Ellison Syndrome
Signup and view all the flashcards
Serological tests for H.pylori
Serological tests for H.pylori
Signup and view all the flashcards
Gastrin levels test
Gastrin levels test
Signup and view all the flashcards
Malabsorption Syndrome
Malabsorption Syndrome
Signup and view all the flashcards
Lactose tolerance test
Lactose tolerance test
Signup and view all the flashcards
Stool cultures & parasite tests
Stool cultures & parasite tests
Signup and view all the flashcards
Fecal fat test
Fecal fat test
Signup and view all the flashcards
Study Notes
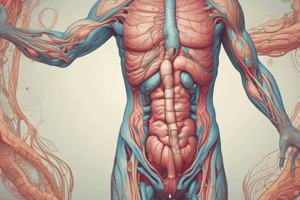
Gastrointestinal Disorders
- Salivary glands include parotid, submandibular, and sublingual glands.
- The oral cavity, pharynx, esophagus, stomach, small intestine (duodenum, jejunum, ileum), colon (ascending, transverse, descending, sigmoid), rectum, and anus are parts of the gastrointestinal tract.
- The liver, gallbladder, and pancreas play crucial roles in digestion.
Anatomy of the GI Tract
- The GI tract is divided into upper and lower portions.
- Key components include the mouth, esophagus, stomach (fundus, cardia, body, pylorus), mucosal lining, and parietal cells.
- The stomach also contains chief cells (pepsinogen), endocrine cells (gastrin), small intestine (duodenum, jejunum, ileum), and large intestine (cecum, ascending, transverse, descending, sigmoid colon, rectum).
- Pancreas, liver, and gallbladder are important for digestion.
Physiology of the GI Tract
- The purpose of the GI tract is ingestion, digestion, and absorption of nutrients.
- Carbohydrates are digested by amylase (from pancreas and brush border), gastrin, HCl (converting pepsinogen to pepsin), and cholecystokinin stimulating the pancreas and gallbladder.
- Proteins are digested in the duodenum.
- Lipids are digested by cholecystokinin stimulating the gallbladder (bile) and pancreas (lipase).
Peptic Ulcers
- Peptic ulcers are breaks in the stomach or duodenal mucosa.
- Helicobacter pylori is a leading cause of duodenal and gastric ulcers.
- Ulcers can lead to perforation.
- Diagnostic methods include gastroscopy, breath tests, stool antigen tests, and serological tests. Transmission is person-to-person, fecal-to-oral, or from contaminated food sources.
GI Ulcers - Diagnosis
- Gastroscopy involves tissue sampling, rapid urease testing (color changes), microbiological cultures, and histology.
- Urea breath tests are widely used, noninvasive, carbon-13 labeled urea.
- Pathogenic H. pylori breaks down urea, releasing labeled CO2 detectable.
- Elevated labeled CO2 indicates H. pylori.
- Tests can determine treatment monitoring and active infections
GI Ulcers - Diagnosis (Stool and Serological Tests)
- Stool tests are reliable, convenient, and noninvasive for H. pylori antigen detection.
- High sensitivity and specificity are common, identify recent infections.
- Serological tests analyze antibodies (IgM, IgA, IgG) to detect H. pylori.
Zollinger-Ellison Syndrome
- Associated with mutations in benign, non-beta-islet cell gastrin-secreting tumors.
- Gastrinomas originate in the pancreas or duodenum.
- Gastrinomas stimulates excess HCl.
- Peptic ulcers can occur in the stomach and duodenum; sometimes they become cancerous.
- Symptoms and signs of the syndrome include gastric pain, fulminant peptic ulcers, massive gastric hypersecretion, hypergastrinemia, diarrhea, and steatorrhea.
Zollinger-Ellison Syndrome - Diagnosis
- Gastrin levels are measured using immunoassays; levels above the reference interval (RI) are diagnostic, often combined with gastric acid hypersecretion.
- Fasting gastrin levels are helpful for diagnosis; this value is also associated with a good prognosis.
- CT scans and gastroscopy are used for imaging and diagnosis.
- H. pylori investigations are commonly negative.
Malabsorption Syndrome
- Malabsorption syndrome involves the defective absorption of nutrients, single or multiple.
- Single nutrient malabsorption, such as lactase deficiency, can lead to lactose excretion.
- Widespread nutrient deficiency can result from conditions like Crohn's disease and celiac disease.
- Common symptoms include diarrhea, abdominal discomfort, and weight loss.
Malabsorption Syndrome - Diagnosis
- Diagnostic tests include CBC, prothrombin time, vitamin and mineral assays, and serologic tests (celiac disease).
- Pancreatic elastase-1 analysis helps distinguish between various digestive issues (maldigestion vs malabsorption).
- Stool cultures check for parasites or bacteria.
- Fecal fat tests help assess the fat content of stools.
- Lactose tolerance tests can identify malabsorption issues.
- Blood glucose levels usually remain normal.
Diarrhea
- Diarrhea is characterized by loose, watery, and frequent stools; it's chronic when lasting beyond 4 weeks.
- Acute diarrhea can result from bacterial, parasitic, viral causes, and antibiotics.
- Chronic diarrhea is linked to inflammatory bowel disease, irritable bowel syndrome, celiac disease, food intolerances (e.g., lactose), chemotherapy, and radiation.
- It may lead to dehydration and low potassium levels.
Diarrhea - Laboratory Tests
- Stool cultures identify infectious agents like C. difficile, rotavirus, and E. coli.
- Immunoassays are used to look for specific pathogens.
- Ova and parasite tests check for parasitic infections.
- Fecal fat tests (nonspecific) help diagnose fat malabsorption.
Inflammatory Bowel Disease (IBD)
- IBD encompasses ulcerative colitis and Crohn's disease.
- IBD etiologies are varied, including unknown autoimmune, genetic, environmental, medications, or infectious factors.
- IBD features intermittent periods of remission and exacerbation.
- Key symptoms include abdominal pain, cramping, anorexia (poor appetite), bloody diarrhea, and anemia.
Crohn's Disease and Ulcerative Colitis Comparison
- Crohn's disease involves the terminal ileum and colon, while ulcerative colitis affects the rectum and colon.
- Crohn's disease involves transmural inflammation affecting all intestinal layers; ulcerative colitis is limited to the mucosa.
- Skip lesions are characteristic of Crohn's disease.
- Presence of granulomas is typical for Crohn's disease and infrequent in ulcerative colitis.
- Fistulas, fissures, abscesses, strictures, and obstructions are more common in Crohn's disease.
- Malabsorption is more common in Crohn's disease.
Inflammatory Bowel Disease (IBD) - Diagnosis
- Comprehensive blood analysis (CBC) and C-reactive protein levels, calprotectin stool tests help identify inflammation.
- Fecal examinations often reveal increased white and red blood cells.
- Stool tests for blood help confirm presence of bleeding.
- Imaging techniques, e.g., MRI or CT scans, identify internal abnormalities.
- Endoscopy and biopsy provide a direct view and sample tissue for analysis.
Celiac Disease
- Celiac disease is an autoimmune disorder triggered by gluten, a protein present in wheat, barley, and rye.
- Symptoms include digestive upset, diarrhea, or significant weight loss.
- It's different from allergies, marked by antibodies to gluten (gliadin).
- Inflammation and malabsorption are hallmarks of celiac disease.
- Gluten-free diets manage symptoms effectively.
Celiac Disease - Diagnosis
- Diagnosis often starts with a detailed medical history and physical exam, evaluating signs and symptoms.
- Biopsies (often endoscopic) of the small intestine are important, enabling assessment of villus atrophy (structural damage).
- Serological blood tests are used to screen for antibodies such as IgA-antiendomysial antibody (EMA), IgA-antigliadin antibody (AGA), IgA-antitissue transglutaminase antibody (tTG), and IgA-deamidated gliadin peptide antibody (DGP).
- These tests aid in accurate diagnosis and monitor disease activity and response to treatment.
Gastrointestinal Function Tests
- Gastrointestinal (GI) function tests evaluate the digestive system.
- Fecal fat analysis can identify abnormalities connected to celiac disease, cystic fibrosis, or pancreatitis.
- 24-hour pH monitoring measures stomach acidity.
- D-Xylose absorption tests diagnose issues with nutrient absorption.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.