Podcast
Questions and Answers
What is the primary function of hydrochloric acid secreted by parietal cells in the stomach?
What is the primary function of hydrochloric acid secreted by parietal cells in the stomach?
- To begin the digestion of dietary fats
- To initiate protein digestion
- To sterilize the meal and begin the hydrolysis of dietary macromolecules (correct)
- To absorb vitamin B12
What is the precursor of pepsin that initiates protein digestion?
What is the precursor of pepsin that initiates protein digestion?
- Pepsinogen (correct)
- Gastric lipase
- Gastrin
- Intrinsic factor
What is the role of histamine in gastric secretion?
What is the role of histamine in gastric secretion?
- To absorb vitamin B12
- To trigger parietal cell secretion (correct)
- To release pepsinogen
- To release gastrin
What is the primary stimulus for gastric secretion during the cephalic phase?
What is the primary stimulus for gastric secretion during the cephalic phase?
What is the approximate amount of gastric secretion added to the intestinal contents daily?
What is the approximate amount of gastric secretion added to the intestinal contents daily?
What is the function of the proton pump in parietal cells?
What is the function of the proton pump in parietal cells?
What is the role of somatostatin in gastric secretion?
What is the role of somatostatin in gastric secretion?
What is the function of intrinsic factor in the stomach?
What is the function of intrinsic factor in the stomach?
What triggers the release of gastrin in the stomach?
What triggers the release of gastrin in the stomach?
What is the primary function of the pancreatic juice?
What is the primary function of the pancreatic juice?
What is the consequence of the release of bicarbonate ions into the bloodstream?
What is the consequence of the release of bicarbonate ions into the bloodstream?
What is the purpose of the 'vago-vagal' reflex during the gastric phase?
What is the purpose of the 'vago-vagal' reflex during the gastric phase?
What is the effect of GIP on gastric secretion and motility?
What is the effect of GIP on gastric secretion and motility?
Which hormone, apart from GIP, also stimulates insulin secretion?
Which hormone, apart from GIP, also stimulates insulin secretion?
What is the name of the hormone that is secreted by enterochromaffin cells and Mo cells in the stomach, small intestine, and colon?
What is the name of the hormone that is secreted by enterochromaffin cells and Mo cells in the stomach, small intestine, and colon?
What stimulates the secretion of Somatostatin?
What stimulates the secretion of Somatostatin?
What is the effect of Somatostatin on the secretion of gastrin?
What is the effect of Somatostatin on the secretion of gastrin?
What is the name of the hormone that is also called glucose-dependent insulinotropic peptide?
What is the name of the hormone that is also called glucose-dependent insulinotropic peptide?
Which of the following is inhibited by somatostatin?
Which of the following is inhibited by somatostatin?
What is the primary function of the enteric nervous system?
What is the primary function of the enteric nervous system?
Which gastrointestinal peptide stimulates growth hormone secretion?
Which gastrointestinal peptide stimulates growth hormone secretion?
What is the location of the myenteric plexus in the gastrointestinal tract?
What is the location of the myenteric plexus in the gastrointestinal tract?
What is the approximate number of neurons in the enteric nervous system in humans?
What is the approximate number of neurons in the enteric nervous system in humans?
What is the primary function of the submucous plexus in the gastrointestinal tract?
What is the primary function of the submucous plexus in the gastrointestinal tract?
What is the primary mechanism controlling the secretion of pancreatic juice?
What is the primary mechanism controlling the secretion of pancreatic juice?
What is the purpose of the trypsin inhibitor secreted by the pancreas?
What is the purpose of the trypsin inhibitor secreted by the pancreas?
What is the approximate volume of pancreatic juice secreted per day?
What is the approximate volume of pancreatic juice secreted per day?
What is the role of bile acids in digestion?
What is the role of bile acids in digestion?
What is the pH of the duodenal contents after the secretion of pancreatic juice and bile?
What is the pH of the duodenal contents after the secretion of pancreatic juice and bile?
What is the mechanism by which digestive enzymes are released from the pancreas?
What is the mechanism by which digestive enzymes are released from the pancreas?
What is the primary function of the gastrointestinal tract?
What is the primary function of the gastrointestinal tract?
Which of the following glands does not drain into the oral cavity?
Which of the following glands does not drain into the oral cavity?
What is the purpose of lysozyme in saliva?
What is the purpose of lysozyme in saliva?
Which section of the gastrointestinal tract is responsible for the majority of nutrient absorption?
Which section of the gastrointestinal tract is responsible for the majority of nutrient absorption?
What is the primary function of salivary secretions in digestion?
What is the primary function of salivary secretions in digestion?
What is the term for the passage of food through the gastrointestinal tract?
What is the term for the passage of food through the gastrointestinal tract?
What is the primary energy source for the apical H+/K+/ATPase in parietal cells?
What is the primary energy source for the apical H+/K+/ATPase in parietal cells?
What is the effect of the meal's physical presence in the stomach during the gastric phase?
What is the effect of the meal's physical presence in the stomach during the gastric phase?
What is the role of somatostatin in terminating gastric secretion?
What is the role of somatostatin in terminating gastric secretion?
What is the effect of pancreatic juice on digestion?
What is the effect of pancreatic juice on digestion?
What is the consequence of bicarbonate ion release into the bloodstream?
What is the consequence of bicarbonate ion release into the bloodstream?
What is the primary stimulus for gastric secretion during the cephalic phase?
What is the primary stimulus for gastric secretion during the cephalic phase?
What is the mechanism by which secretin regulates pH in the duodenum?
What is the mechanism by which secretin regulates pH in the duodenum?
What is the primary stimulus for the secretion of secretin?
What is the primary stimulus for the secretion of secretin?
What is the effect of secretin on pancreatic secretion?
What is the effect of secretin on pancreatic secretion?
What is the half-life of secretin?
What is the half-life of secretin?
What is the effect of secretin on gastric acid secretion?
What is the effect of secretin on gastric acid secretion?
What is the location of the cells that produce secretin?
What is the location of the cells that produce secretin?
What is the role of gastrin-releasing peptide in the regulation of gastric secretion?
What is the role of gastrin-releasing peptide in the regulation of gastric secretion?
What is the primary function of intrinsic factor in the stomach?
What is the primary function of intrinsic factor in the stomach?
What is the source of gastric lipase in the stomach?
What is the source of gastric lipase in the stomach?
What is the effect of histamine on parietal cells?
What is the effect of histamine on parietal cells?
What is the approximate volume of gastric secretion added to the intestinal contents daily?
What is the approximate volume of gastric secretion added to the intestinal contents daily?
What is the role of hydrochloric acid secreted by parietal cells in the stomach?
What is the role of hydrochloric acid secreted by parietal cells in the stomach?
What is the primary mechanism by which CCK exerts its trophic effect on the pancreas?
What is the primary mechanism by which CCK exerts its trophic effect on the pancreas?
What is the primary stimulus for the secretion of CCK in the small intestine?
What is the primary stimulus for the secretion of CCK in the small intestine?
What is the effect of CCK on the motility of the small intestine and colon?
What is the effect of CCK on the motility of the small intestine and colon?
What is the site of action of CCK in the regulation of food intake?
What is the site of action of CCK in the regulation of food intake?
What is the effect of CCK on the secretion of gastric acid?
What is the effect of CCK on the secretion of gastric acid?
What is the location of CCK receptors in the gut?
What is the location of CCK receptors in the gut?
Flashcards are hidden until you start studying
Study Notes
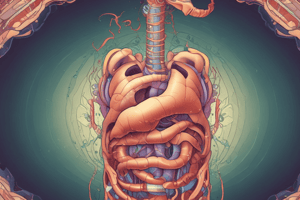
Gastrointestinal Function and Regulation
- The primary function of the gastrointestinal tract is to serve as a portal for the absorption of nutrients and water into the body.
- The gastrointestinal tract is divided into several parts, including the mouth, esophagus, stomach, duodenum, jejunum, ileum, cecum, colon, rectum, and anus.
Gastrointestinal Secretions
- Salivary Secretion:
- Produced by three pairs of salivary glands (parotid, submandibular, and sublingual glands) that drain into the oral cavity.
- Contains organic constituents that initiate digestion (particularly of starch, mediated by amylase) and protect the oral cavity from bacteria (such as immunoglobulin A and lysozyme).
- Gastric Secretion:
- Arises from glands in the wall of the stomach that drain into its lumen, and also from the surface cells that secrete primarily mucus and bicarbonate to protect the stomach from digesting itself.
- Adds about 2.5 L/day to the intestinal contents.
- Contains parietal cells that secrete hydrochloric acid and intrinsic factor, and chief cells that produce pepsinogens and gastric lipase.
- Acid secreted by parietal cells serves to sterilize the meal and begin the hydrolysis of dietary macromolecules.
- Pancreatic Secretion:
- Contains enzymes that are of major importance in digestion.
- About 1500 mL of pancreatic juice is secreted per day.
- Contains a range of digestive enzymes, most of which are released in inactive forms and only activated when they reach the intestinal lumen.
- Biliary Secretion:
- Arises from the liver and contains bile acids that are important in the digestion and absorption of fats.
- Stimulated by glucose and fat in the duodenum.
Hormonal Regulation of Gastrointestinal Function
- Gastrin:
- Released by G cells in the antrum of the stomach in response to a specific neurotransmitter released from enteric nerve endings, known as gastrin-releasing peptide (GRP).
- Stimulates parietal cell secretion and increases acid secretion.
- Histamine:
- Triggers parietal cell secretion, via binding to H2-receptors.
- Cholecystokinin (CCK):
- Secreted by endocrine cells known as I cells in the mucosa of the upper small intestine.
- Stimulates pancreatic enzyme secretion, contraction of the gallbladder, relaxation of the sphincter of Oddi, and inhibits gastric emptying.
- Exerts a trophic effect on the pancreas and enhances the motility of the small intestine and colon.
- Secretin:
- Secreted by S cells that are located deep in the glands of the mucosa of the upper portion of the small intestine.
- Increases the secretion of bicarbonate by the duct cells of the pancreas and biliary tract, and causes the secretion of a watery, alkaline pancreatic juice.
- Gastric Inhibitory Peptide (GIP):
- Produced by K cells in the mucosa of the duodenum and jejunum.
- Stimulates insulin secretion and inhibits gastric acid secretion and motility.
- Motilin:
- Secreted by enterochromaffin cells (EC) and Mo cells in the stomach, small intestine, and colon.
- Acts on G-protein–coupled receptors on enteric neurons in the duodenum and colon and produces contraction of smooth muscle in the stomach and intestines in the period between meals.
- Somatostatin:
- Secreted by D cells in the gastrointestinal mucosa.
- Inhibits the secretion of gastrin, VIP, GIP, secretin, and motilin, and acts in a paracrine fashion to mediate the inhibition of gastrin secretion produced by acid.
Enteric Nervous System
- The enteric nervous system is a network of nerve fibers that are intrinsic to the gastrointestinal tract.
- Consists of two major networks of nerve fibers: the myenteric plexus (Auerbach plexus) and the submucous plexus (Meissner plexus).
- Contains about 100 million sensory neurons, interneurons, and motor neurons in humans.
- Is connected to the CNS by parasympathetic and sympathetic fibers but can function autonomously without these connections.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.