Podcast
Questions and Answers
Which of the following is the primary mechanism by which oxygen is transported in the blood?
Which of the following is the primary mechanism by which oxygen is transported in the blood?
- Attached to white blood cells
- Transported as bicarbonate
- Dissolved directly in the plasma
- Bound to hemoglobin within red blood cells (correct)
What percentage of oxygen in the blood is bound to hemoglobin?
What percentage of oxygen in the blood is bound to hemoglobin?
- 98.5% (correct)
- 70%
- 23%
- 1.5%
How many oxygen molecules can each hemoglobin molecule bind?
How many oxygen molecules can each hemoglobin molecule bind?
- Four (correct)
- One
- Eight
- Two
Which of the following factors does NOT contribute to the unloading of oxygen from hemoglobin in the tissues?
Which of the following factors does NOT contribute to the unloading of oxygen from hemoglobin in the tissues?
In what form is the majority of carbon dioxide transported in the blood?
In what form is the majority of carbon dioxide transported in the blood?
Which enzyme catalyzes the reaction between carbon dioxide and water to form carbonic acid?
Which enzyme catalyzes the reaction between carbon dioxide and water to form carbonic acid?
What is the effect of increased hydrogen ion concentration on the affinity of hemoglobin for oxygen?
What is the effect of increased hydrogen ion concentration on the affinity of hemoglobin for oxygen?
During exercise, what physiological change leads to increased oxygen unloading from hemoglobin?
During exercise, what physiological change leads to increased oxygen unloading from hemoglobin?
Where are the central chemoreceptors that regulate respiration located?
Where are the central chemoreceptors that regulate respiration located?
Which of the following stimuli primarily drives the increase in respiration rate during exercise?
Which of the following stimuli primarily drives the increase in respiration rate during exercise?
What is the primary cause of respiratory acidosis?
What is the primary cause of respiratory acidosis?
How does hyperventilation lead to respiratory alkalosis?
How does hyperventilation lead to respiratory alkalosis?
What is the primary compensatory mechanism for respiratory alkalosis?
What is the primary compensatory mechanism for respiratory alkalosis?
Which condition is characterized by inadequate oxygen delivery to the tissues due to impaired blood flow?
Which condition is characterized by inadequate oxygen delivery to the tissues due to impaired blood flow?
What is the underlying cause of anemic hypoxia?
What is the underlying cause of anemic hypoxia?
Which type of hypoxia is caused by the inability of tissues to effectively use oxygen, often due to poisoning?
Which type of hypoxia is caused by the inability of tissues to effectively use oxygen, often due to poisoning?
What is a common cause of hypoxemic hypoxia?
What is a common cause of hypoxemic hypoxia?
Which of the following is the primary characteristic of pulmonary hypertension?
Which of the following is the primary characteristic of pulmonary hypertension?
What is a pneumothorax?
What is a pneumothorax?
Why does oxygen diffuse from the alveoli into the blood?
Why does oxygen diffuse from the alveoli into the blood?
Which of the following would cause a rightward shift in the oxygen-hemoglobin dissociation curve?
Which of the following would cause a rightward shift in the oxygen-hemoglobin dissociation curve?
How would the body typically respond to respiratory alkalosis caused by hyperventilation at high altitude?
How would the body typically respond to respiratory alkalosis caused by hyperventilation at high altitude?
A patient presents with cyanosis and normal arterial $PO_2$. Which type of hypoxia is most likely?
A patient presents with cyanosis and normal arterial $PO_2$. Which type of hypoxia is most likely?
How does carbon monoxide (CO) lead to hypoxia?
How does carbon monoxide (CO) lead to hypoxia?
Which of the following parameters is most directly monitored by peripheral chemoreceptors?
Which of the following parameters is most directly monitored by peripheral chemoreceptors?
A patient with a history of COPD presents with increased dyspnea and a blood gas analysis showing a normal pH. Which of the following is MOST likely explanation of this blood gas result given their history?
A patient with a history of COPD presents with increased dyspnea and a blood gas analysis showing a normal pH. Which of the following is MOST likely explanation of this blood gas result given their history?
A climber ascending Mount Everest begins to hyperventilate. What is the primary physiological benefit of this response in the context of high altitude?
A climber ascending Mount Everest begins to hyperventilate. What is the primary physiological benefit of this response in the context of high altitude?
In a patient experiencing a panic attack, hyperventilation leads to tingling and muscle cramps. What is the underlying mechanism for these symptoms?
In a patient experiencing a panic attack, hyperventilation leads to tingling and muscle cramps. What is the underlying mechanism for these symptoms?
If a patient has a condition that increases the amount of fibrous tissue in their lungs, hindering their ability to fully expand their lungs, which of the following would be the MOST accurate description of their condition?
If a patient has a condition that increases the amount of fibrous tissue in their lungs, hindering their ability to fully expand their lungs, which of the following would be the MOST accurate description of their condition?
A patient has a pulmonary embolism that blocked the pulmonary artery going to the left lung. What would you expect to happen to the blood of the left atrium of the heart?
A patient has a pulmonary embolism that blocked the pulmonary artery going to the left lung. What would you expect to happen to the blood of the left atrium of the heart?
A large clot develops in the venous blood returning from the leg of a bedridden hospital patient. This clot dislodges and travels to the lungs, blocking a major pulmonary artery. What is the MOST immediate and life-threatening consequence of this event?
A large clot develops in the venous blood returning from the leg of a bedridden hospital patient. This clot dislodges and travels to the lungs, blocking a major pulmonary artery. What is the MOST immediate and life-threatening consequence of this event?
A researcher is studying the hemoglobin of deep-diving seals, which can maintain oxygen delivery to tissues under extreme pressure. Which adaptation is MOST likely to be found in seal hemoglobin compared to human hemoglobin?
A researcher is studying the hemoglobin of deep-diving seals, which can maintain oxygen delivery to tissues under extreme pressure. Which adaptation is MOST likely to be found in seal hemoglobin compared to human hemoglobin?
During strenuous exercise, muscle cells produce lactic acid, leading to a decrease in intracellular pH. How does this intracellular acidosis affect oxygen delivery?
During strenuous exercise, muscle cells produce lactic acid, leading to a decrease in intracellular pH. How does this intracellular acidosis affect oxygen delivery?
A patient with chronic kidney disease has a reduced production of erythropoietin (EPO). How does this MOST DIRECTLY affect oxygen transport?
A patient with chronic kidney disease has a reduced production of erythropoietin (EPO). How does this MOST DIRECTLY affect oxygen transport?
An individual ingests a poison that inhibits carbonic anhydrase in red blood cells. How would this affect carbon dioxide transport?
An individual ingests a poison that inhibits carbonic anhydrase in red blood cells. How would this affect carbon dioxide transport?
A patient develops a spontaneous pneumothorax. Besides the presence of air in the pleural space, what other immediate physiological change occurs?
A patient develops a spontaneous pneumothorax. Besides the presence of air in the pleural space, what other immediate physiological change occurs?
Flashcards
Gas Exchange
Gas Exchange
Exchange of O₂ and CO₂ in the alveoli and systemic tissues.
Oxygen in Blood
Oxygen in Blood
Hemoglobin is mostly bound to oxygen in blood, a small amount of oxygen is dissolved in blood
Carbon Dioxide in Blood
Carbon Dioxide in Blood
Carbon dioxide is transported in the blood as carbonic acid, carbamino compounds, and dissolved gas.
Systemic Circulation: Oxygen Unloading
Systemic Circulation: Oxygen Unloading
Signup and view all the flashcards
Differential Oxygen Delivery: PO₂
Differential Oxygen Delivery: PO₂
Signup and view all the flashcards
Differential Oxygen Delivery: Temperature
Differential Oxygen Delivery: Temperature
Signup and view all the flashcards
Differential Oxygen Delivery: pH
Differential Oxygen Delivery: pH
Signup and view all the flashcards
Respiratory Rhythm: Rate and Depth
Respiratory Rhythm: Rate and Depth
Signup and view all the flashcards
Respiratory Rhythm: Acidosis
Respiratory Rhythm: Acidosis
Signup and view all the flashcards
Respiratory Rhythm: Alkalosis
Respiratory Rhythm: Alkalosis
Signup and view all the flashcards
Exercise
Exercise
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Oxygen Imbalances: Hypoxemic hypoxia
Oxygen Imbalances: Hypoxemic hypoxia
Signup and view all the flashcards
Oxygen Imbalances: Ischemic hypoxia
Oxygen Imbalances: Ischemic hypoxia
Signup and view all the flashcards
Oxygen Imbalances: Anemic hypoxia
Oxygen Imbalances: Anemic hypoxia
Signup and view all the flashcards
Oxygen Imbalances: Histotoxic hypoxia
Oxygen Imbalances: Histotoxic hypoxia
Signup and view all the flashcards
Pulmonary Hypertension (PH)
Pulmonary Hypertension (PH)
Signup and view all the flashcards
Pneumothorax - Spontaneous
Pneumothorax - Spontaneous
Signup and view all the flashcards
Study Notes
- Chapter 22 covers gas transport, oxygen use, cellular respiration, and respiratory disorders.
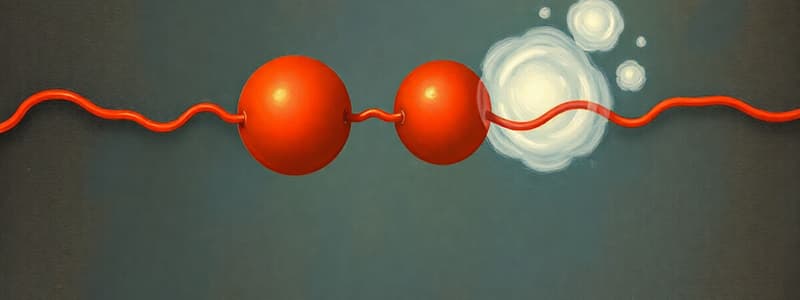
Gas Exchange
- Occurs in the alveoli and systemic tissues.
- Focus is on the exchange of oxygen (O₂) and carbon dioxide (CO₂).
Oxygen in Blood
- 98.5% of oxygen is bound to hemoglobin within red blood cells (RBCs).
- Only 1.5% of oxygen is dissolved in blood.
- Hemoglobin consists of 4 globin chains and 4 heme groups.
- Each heme group binds one O₂ molecule to an iron atom.
- 100% saturation means all available oxygen binding sites on hemoglobin are occupied.
- Binding of O₂ causes hemoglobin to change shape, enhancing its affinity for more O₂.
Carbon Dioxide in Blood
- 90% of carbon dioxide is transported as carbonic acid.
- Carbonic acid forms from CO₂ and H₂O, which then dissociates into H+ and HCO₃-.
- 5% of carbon dioxide is transported as carbamino compounds bound to plasma proteins, including hemoglobin.
- Hemoglobin can bind CO₂ (HbCO₂), but it binds to a polypeptide rather than heme.
- Carbon dioxide can bind along with oxygen inhibiting the oxygen.
- 5% of carbon dioxide is transported as dissolved gas.
- Blood gives up dissolved and HbCO₂ more readily.
- 70% of exchanged CO₂ is from H. CO.
Systemic Circulation
- Oxygen is unloaded from hemoglobin in systemic circulation, where CO₂ enters the blood.
- CO₂ combines with H₂O to form H₂CO₃, which dissociates into HCO₃- and H+.
- H+ can bind to hemoglobin inside RBCs.
- This process lowers hemoglobin's affinity for O₂.
- Tissues using O₂ undergo aerobic respiration.
- This maintains a low O₂ level of about 40 mm Hg.
- O₂ diffuses into tissues from hemoglobin and dissolved oxygen.
Differential Oxygen Delivery
- PO₂ affects oxygen delivery.
- Cells using more O₂ maintain a steeper partial pressure gradient, which promotes more oxygen unloading.
- Temperature influences oxygen release.
- Higher temperatures in metabolizing tissues result in more O₂ unloading.
- pH affects oxygen affinity.
- More CO₂ means more H+, which weakens the O₂-Hb bond, meaning lower saturation.
- BPG (Bisphosphoglycerate) influences oxygen delivery.
- RBCs have no mitochondria, and anaerobic glycolysis produces BPG.
Respiratory Rhythm
- Rate and depth of breathing are influenced by pH, PCO₂, and PO₂.
- pH is first and should be between 7.35-7.45.
- PCO₂ is second with a level of 40 mm HG.
- PO₂ is third with a level of 95 mm Hg.
- Chemoreceptors detect changes in pH, CO₂, and O₂.
- 75% of chemoreceptors are central receptors.
- H+ does not cross the brain-barrier, thus C02 becomes H₂CO₃ in CSF.
- There are few buffers to hind with H= and they are more sensitive to pH.
- 25% are peripheral receptors.
- Integration occurs in the Dorsal Respiratory Group (DRG) and VRG.
Respiratory Rate and Rhythm Disorders
- Acidosis occurs when pH is below 7.35.
- Respiratory acidosis is caused by hypoventilation and can be corrected by hyperventilating.
- CO₂ is expired + H₂O becomes H₂CO₃, then HCO₃ + ↓ H+.
- Alkalosis occurs when pH is above 7.45.
- Respiratory alkalosis is caused by hyperventilating and can be corrected by hypoventilating.
- CO₂ + H₂O becomes H₂CO₃, then HCO3- + ↑H+.
- It can also be corrected by rebreathing from a bag.
Exercise
- Exercise leads to heavy breathing, due to an increased CO2 level, by maintaining normal conditions.
- Anticipatory effect: The brain sends motor commands to muscles. Signals are also sent to respiratory centers. Increase respiration anticipating activity.
Oxygen Imbalances
- Hypoxia is an oxygen deficiency.
- Hypoxemic hypoxia: This occurs due to inadequate pulmonary exchange, often due to high elevation, impaired ventilation and/or lung disease.
- Ischemic hypoxia: Poor blood circulation, and/or heart failure.
- Anemic hypoxia: Low RBC count, and/or hemoglobin deficiency.
- Histotoxic hypoxia: Metabolic poison. Prevents tissues from using oxygen.
Pulmonary Hypertension (PH)
- High blood pressure in pulmonary vessels.
- Causes include narrowed, blocked or destroyed blood vessels in the lungs, COPD, blood clots and genetics.
- It also causes disproportionate effect on heart, more specifically the right side. Increased heart failure.
Pneumothorax- Spontaneous
- Air in the pleural cavity.
- Visceral pleura punctured, and blebs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.