Podcast
Questions and Answers
What is the primary advantage of casting over soldering in fixed prosthodontics?
What is the primary advantage of casting over soldering in fixed prosthodontics?
- It requires less technical expertise
- It allows for more uniform and controllable connections (correct)
- It is a more cost-effective method
- It produces stronger bridges
What is the purpose of soldering in fixed prosthodontics?
What is the purpose of soldering in fixed prosthodontics?
- To section a single unit pattern
- To connect multiple units together (correct)
- To create a single unit pattern
- To fabricate pontics and retainers separately
What is a characteristic of soldered connectors in fixed prosthodontics?
What is a characteristic of soldered connectors in fixed prosthodontics?
- They are less strong than cast connections
- They are more prone to galvanic corrosion
- They are more uniform, flat, and parallel (correct)
- They are more difficult to control
How are pontics and retainers fabricated in a fixed fixed bridge?
How are pontics and retainers fabricated in a fixed fixed bridge?
What is the term for a fixed bridge that is also removable?
What is the term for a fixed bridge that is also removable?
How many types of fixed bridges are listed in the lecture?
How many types of fixed bridges are listed in the lecture?
Why are electrosurgical procedures avoided in patients with pacemaker?
Why are electrosurgical procedures avoided in patients with pacemaker?
What is a consideration for patients with uncontrolled diabetes mellitus?
What is a consideration for patients with uncontrolled diabetes mellitus?
Why is it important to note medications a patient is currently taking?
Why is it important to note medications a patient is currently taking?
What is a potential consequence of xerostomia on dental restorations?
What is a potential consequence of xerostomia on dental restorations?
What is the primary purpose of obtaining a dental history?
What is the primary purpose of obtaining a dental history?
What is the purpose of clinical examination in dental evaluation?
What is the purpose of clinical examination in dental evaluation?
What is assessed during the general appearance evaluation of a patient?
What is assessed during the general appearance evaluation of a patient?
What is a potential consequence of not considering a patient's medical history in treatment planning?
What is a potential consequence of not considering a patient's medical history in treatment planning?
During the extraoral examination, which of the following muscles are palpated?
During the extraoral examination, which of the following muscles are palpated?
What is the maximum jaw opening indicative of jaw restriction?
What is the maximum jaw opening indicative of jaw restriction?
During the Temporo-mandibular joint (TMJ) examination, what is palpated?
During the Temporo-mandibular joint (TMJ) examination, what is palpated?
What is measured during the Temporo-mandibular joint (TMJ) examination?
What is measured during the Temporo-mandibular joint (TMJ) examination?
Why is pulpal health measured before restorative treatment?
Why is pulpal health measured before restorative treatment?
What is the purpose of the intraoral examination?
What is the purpose of the intraoral examination?
What is recorded during the intraoral examination?
What is recorded during the intraoral examination?
What is palpated during the extraoral examination?
What is palpated during the extraoral examination?
What is the primary purpose of recording the chief complaint in a patient's own words?
What is the primary purpose of recording the chief complaint in a patient's own words?
What type of information should be included in a patient's medical history?
What type of information should be included in a patient's medical history?
What is the significance of determining the prognosis of a patient?
What is the significance of determining the prognosis of a patient?
What is the purpose of a screening questionnaire in history taking?
What is the purpose of a screening questionnaire in history taking?
What is the benefit of including a patient's personal details in their history?
What is the benefit of including a patient's personal details in their history?
What is a characteristic of patients with cardiovascular conditions?
What is a characteristic of patients with cardiovascular conditions?
What is the primary purpose of a treatment plan?
What is the primary purpose of a treatment plan?
What is the significance of a realistic treatment plan?
What is the significance of a realistic treatment plan?
What is the primary focus when recording tooth mobility?
What is the primary focus when recording tooth mobility?
What should be examined carefully in a radiograph?
What should be examined carefully in a radiograph?
What is NOT a part of the supplement information provided by radiographic examination?
What is NOT a part of the supplement information provided by radiographic examination?
What is the purpose of evaluating the bone before implant placement?
What is the purpose of evaluating the bone before implant placement?
What is the primary purpose of vitality testing?
What is the primary purpose of vitality testing?
How is a diagnosis of non-vitality confirmed?
How is a diagnosis of non-vitality confirmed?
What is the primary goal of patient history taking in prosthodontics?
What is the primary goal of patient history taking in prosthodontics?
What is the significance of evaluating the crown-root ratio in radiographic evaluation?
What is the significance of evaluating the crown-root ratio in radiographic evaluation?
What is the primary purpose of diagnostic casts?
What is the primary purpose of diagnostic casts?
Which of the following is a benefit of including diagnostic photography in treatment planning?
Which of the following is a benefit of including diagnostic photography in treatment planning?
What is the goal of an ideal treatment plan?
What is the goal of an ideal treatment plan?
What is the first step in the mouth preparation sequence?
What is the first step in the mouth preparation sequence?
What is the purpose of evaluating the path of insertion in diagnostic casts?
What is the purpose of evaluating the path of insertion in diagnostic casts?
What can be evaluated using diagnostic casts?
What can be evaluated using diagnostic casts?
What is the primary goal of mouth preparation?
What is the primary goal of mouth preparation?
What is the benefit of using diagnostic casts to evaluate occlusion?
What is the benefit of using diagnostic casts to evaluate occlusion?
What is the primary advantage of a pontic with mucosal contact?
What is the primary advantage of a pontic with mucosal contact?
What is a characteristic of a pontic without mucosal contact (hygienic pontic)?
What is a characteristic of a pontic without mucosal contact (hygienic pontic)?
What is an indication for a pontic without mucosal contact (hygienic pontic)?
What is an indication for a pontic without mucosal contact (hygienic pontic)?
What is a characteristic of a complete metal crown?
What is a characteristic of a complete metal crown?
What is an advantage of minimal-preparation retainers?
What is an advantage of minimal-preparation retainers?
What is a characteristic of all ceramic crowns?
What is a characteristic of all ceramic crowns?
What is a consideration when choosing between creating space by reducing the opposing teeth, moving the abutment teeth orthodontically, and a combination of these approaches?
What is a consideration when choosing between creating space by reducing the opposing teeth, moving the abutment teeth orthodontically, and a combination of these approaches?
What is the primary advantage of partial veneer crowns?
What is the primary advantage of partial veneer crowns?
What is the classification of a fixed partial denture that extends both anteriorly and posteriorly?
What is the classification of a fixed partial denture that extends both anteriorly and posteriorly?
What type of abutment is used in a cantilever design?
What type of abutment is used in a cantilever design?
What type of connector allows for some vertical movement?
What type of connector allows for some vertical movement?
What is the term for a crown that is made of metal with a ceramic layer on top?
What is the term for a crown that is made of metal with a ceramic layer on top?
What type of restoration is fabricated using only ceramics with no metal component?
What type of restoration is fabricated using only ceramics with no metal component?
What type of prosthesis is developed by Dr. James Andrews?
What type of prosthesis is developed by Dr. James Andrews?
What is the purpose of the retainer in a fixed dental prosthesis?
What is the purpose of the retainer in a fixed dental prosthesis?
What is the main difference between a posterior and an anterior fixed partial denture?
What is the main difference between a posterior and an anterior fixed partial denture?
What is the primary advantage of using a cantilever design?
What is the primary advantage of using a cantilever design?
What type of crowns cover all the five surfaces of the abutment?
What type of crowns cover all the five surfaces of the abutment?
What is the main consideration when using a spring cantilever design?
What is the main consideration when using a spring cantilever design?
What type of retainers are indicated for extensively damaged teeth?
What type of retainers are indicated for extensively damaged teeth?
What is the main difference between metal with ceramic facing and metal with resin facings?
What is the main difference between metal with ceramic facing and metal with resin facings?
What type of restorations are used as provisional restorations?
What type of restorations are used as provisional restorations?
What is the purpose of the connector in a fixed dental prosthesis?
What is the purpose of the connector in a fixed dental prosthesis?
What type of retainers are used for minimal preparation bridges?
What type of retainers are used for minimal preparation bridges?
What is a characteristic of a full veneer crown?
What is a characteristic of a full veneer crown?
What is the primary purpose of a laminate veneer?
What is the primary purpose of a laminate veneer?
What is the difference between a retainer and an abutment?
What is the difference between a retainer and an abutment?
What is a post crown?
What is a post crown?
What is the term for a natural tooth that stands between and supports two pontics?
What is the term for a natural tooth that stands between and supports two pontics?
What is the purpose of a connector in a bridge?
What is the purpose of a connector in a bridge?
What is the term for a fixed bridge that consists of two retainers and one pontic?
What is the term for a fixed bridge that consists of two retainers and one pontic?
What type of retainer is always present at one end of the pontic in fixed-movable bridges?
What type of retainer is always present at one end of the pontic in fixed-movable bridges?
Which of the following is a consideration when selecting a retainer for a pontic?
Which of the following is a consideration when selecting a retainer for a pontic?
When abutment teeth are not parallel to each other, what is the solution to achieve a single path of insertion?
When abutment teeth are not parallel to each other, what is the solution to achieve a single path of insertion?
What is a characteristic of partial veneer crowns?
What is a characteristic of partial veneer crowns?
Why is a complete crown retainer chosen in some cases?
Why is a complete crown retainer chosen in some cases?
What is the least conservative type of dental crown?
What is the least conservative type of dental crown?
Why is it important to conserve the buccal/facial surface of the tooth?
Why is it important to conserve the buccal/facial surface of the tooth?
What should be considered when deciding between a partial crown and a complete crown retainer?
What should be considered when deciding between a partial crown and a complete crown retainer?
Flashcards are hidden until you start studying
Study Notes
Types of Fixed Bridges
- There are 12 types of fixed bridges: Fixed Fixed Bridge, Fixed Movable Bridges, Cantilever Fixed Bridges, Spring Cantilever Fixed Bridges, Fixed Removable Bridges, Modified Fixed Removable Bridges, All Metal Fixed Bridges, Metal-ceramic Fixed Bridges, All Ceramic Fixed Bridges, All Acrylic Fixed Bridges, Fiber-reinforced Composite Resin Bridges, and Resin-bonded Fixed Bridges
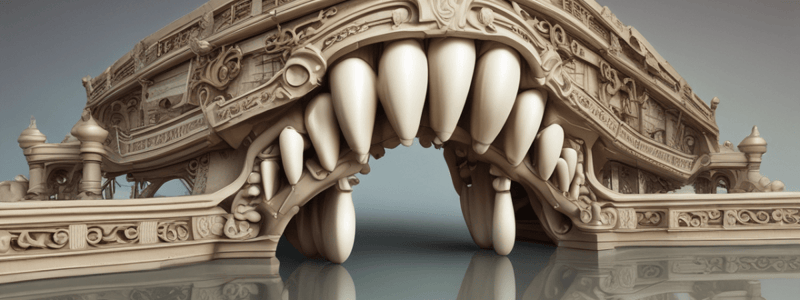
Fabrication of Fixed Bridges
- The pontics and retainers are fabricated as a single unit pattern
- Multiunit wax patterns are cast separately and approximated against each other and soldered together using a different soldering alloy
- Alternatively, a single unit wax pattern is cast, sectioned using a saw, and then soldered
Soldering in Fixed Bridge Fabrication
- Used to join multiple units together
- Preferred because it avoids galvanic corrosion
- Soldered connectors are uniform, flat, and parallel due to the controllable flow of the solder alloy
Electrosurgical Procedures and Medical Conditions
- Electrosurgical procedures are avoided in patients with pacemakers.
- Adrenaline may be avoided in local anesthetic and during retraction procedures in patients with hypertension.
- Uncontrolled diabetes mellitus can lead to periodontal breakdown and affect prognosis.
- Xerostomia (dry mouth) can lead to caries affecting restoration margins.
- Patients with certain medical conditions, such as pacemakers, may need to discontinue medications before surgical procedures.
Dental History
- Obtaining a dental history provides information about previously rendered dental treatment.
- It highlights genetic predisposition to periodontal disease, malocclusion, and facial deformities.
- It also reveals cause for tooth loss, complications following dental procedures, and patient attitude towards oral hygiene measures.
Clinical Examination
- Clinical examination involves the clinician's use of sight, touch, and hearing to detect conditions outside the normal range.
- General appearance includes gait, weight, skin color, and vital signs (respiration, pulse, temperature, and blood pressure).
- Fixed Prosthodontics involves diagnosis and treatment planning.
Diagnosis and Treatment Planning
- Diagnosis is the determination of the nature of the disease process.
- A good diagnostic work-up includes seven elements: chief complaint, vitality testing, history, extra-oral examination, intra-oral examination, diagnostic casts, and radiographic evaluation.
Chief Complaint
- The chief complaint should be recorded in the patient's own words.
- It should analyze the patient's primary reason for seeking treatment and reveal problems and conditions of which the patient is often unaware.
- Complaints usually belong to one of the following categories: comfort, function, social, or appearance.
History
- A patient's history should include necessary information concerning the reasons for seeking treatment, as well as personal details and past medical and dental experiences.
- A screening questionnaire is useful for history taking.
- Medical history should include any medication the patient is taking and all relevant medical conditions.
Extra-Oral Examination
- Facial asymmetry, cervical lymph nodes, TMJ, and muscles of mastication are assessed.
Diagnostic Aids
- Radiographs, vitality tests, diagnostic casts, and periodontal probes are used as diagnostic aids.
Intra-Oral Examination
- The patient's general oral hygiene is observed, and the presence or absence of inflammation, gingival architecture, and stippling are noted.
- Pockets and tooth mobility are recorded with special attention to any relationship with occlusal prematurities and potential abutment teeth.
Radiographic Evaluation
- Radiographs are examined for caries, P.A lesions, previous endodontic treatment, alveolar bone level, crown-root ratio, root configuration, and direction of root.
- The presence of retained root in edentulous areas is recorded.
Vitality Testing
- Pulpal health must be assessed, usually by measuring the response to percussion, thermal, and electrical stimulation.
Diagnostic Casts
- Diagnostic casts are mounted on a semi-adjustable articulator to assess the edentulous space, abutment teeth, and path of insertion.
- They are used for diagnostic wax-up, constructing special trays, and provisional restorations.
Ideal Treatment Plan
- An ideal treatment plan achieves the best possible long-term outcomes for the patient while addressing all patient concerns and active problems with the minimum necessary intervention.
Occlusion
- In some cases, the abutment teeth are sound, but there is insufficient space for a minimal-preparation retainer, so the choice is between creating space by reducing the opposing teeth, moving the abutment teeth orthodontically, or a combination of these approaches.
Cost
- Partial crowns and complete metal crowns may be less expensive than metal-ceramic crowns.
- Minimal-preparation retainers are the least expensive.
- All-ceramic crowns are the most expensive.
Pontics
- A pontic is an artificial tooth that replaces a missing natural tooth, restoring its function and usually filling the space previously occupied by the clinical crown.
- Ideal requirements of a pontic:
- Restore function of the replaced tooth.
- Provide aesthetics and comfort.
- Be biologically acceptable.
- Permit effective oral hygiene.
- Preserve the underlying residual ridge and mucosa.
- Have adequate strength to withstand occlusal forces.
- Classification of pontics based on the amount of contact with the underlying mucosa:
- With mucosal contact:
- Advantage: Aesthetically superior.
- Disadvantages: Difficulty in cleaning, potential tissue inflammation.
- Without mucosal contact (hygienic pontic):
- Advantage: Good access for oral hygiene.
- Disadvantage: Poor aesthetics.
- With mucosal contact:
Crowns
- A crown is a fixed extra-coronal restoration that restores missing tooth structure by surrounding most or all of the remaining structure with material.
- Types of crowns:
- Full veneer crown: Involves all surfaces of the clinical crown.
- Partial veneer crown: Covers some of the tooth crown and leaves the other intact (e.g., 3/4 crown, 7/8 crown, pin ledge, etc.).
- Laminate veneers: A conservative method of restoring the appearance of discolored, pitted, or fractured anterior teeth, consisting of bonding thin ceramic laminates onto the labial surfaces of affected teeth.
- Complete replacement (Post crown): Replaces the natural crown entirely, retaining itself by means of a dowel (post) extended inside the root canal space of the tooth.
Abutment and Retainer
- An abutment is a tooth to which a bridge (or partial denture) is attached.
- A retainer is a crown or other restoration that is cemented to the abutment.
- The terms 'retainer' and 'abutment' should not be confused or used interchangeably.
Bridge Components
- A span is the space between natural teeth that is to be filled by the bridge.
- A unit, when applied to bridgework, means either a retainer or a pontic.
- A connector (or joint) connects a pontic to a retainer, or two retainers to each other.
- Connectors may be fixed or allow some movement between the components that they join.
Retainer Selection
- Criteria for selecting a particular retainer include:
- Alignment of abutment teeth and retention.
- Appearance.
- Condition of abutment teeth.
- Conservation of tooth tissue.
- Occlusion.
- Cost.
Classification of Fixed Partial Dentures
- According to the location of the edentulous space:
- Posterior: Fixed partial denture confined to the posterior region.
- Anterior: Fixed partial denture confined to the anterior region.
- Combination: Fixed partial denture extending both anteriorly and posteriorly.
- According to the location of the abutment:
- Conventional: Abutment is located adjacent to the edentulous space and pontic is supported on both sides.
- Cantilever: Abutment is located adjacent to the edentulous space but pontic is supported on one side only.
- Spring cantilever: Abutment is not located adjacent to the edentulous space and pontic receives support from one side only.
Types of Connectors
- Fixed-fixed: Connectors on both sides of the pontic are rigid with no scope for any movement.
- Fixed-movable: One of the connectors of the FPD assembly is non-rigid and is made of a precision or semiprecision attachment which allows some vertical movement.
- Fixed-removable: This prosthesis was developed by Dr. James Andrews and is called 'Andrews Bridge'.
Materials Used
- All metal: Used only to replace posterior teeth, not aesthetic.
- Metal ceramic: Also termed as 'porcelain fused to metal' (PFM) crowns/retainers.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.