Podcast
Questions and Answers
During which phase of meiosis is the secondary oocyte arrested?
During which phase of meiosis is the secondary oocyte arrested?
- Anaphase I
- Metaphase II (correct)
- Telophase II
- Prophase I
What is the role of granulosa cells in relation to oocyte maturation?
What is the role of granulosa cells in relation to oocyte maturation?
- Initiation of the second meiotic division
- Secretion of an inhibitor to arrest the oocyte in prophase I (correct)
- Stimulation of the completion of meiosis II
- Degeneration of the first polar body
Which event immediately follows the completion of the first meiotic division in oogenesis?
Which event immediately follows the completion of the first meiotic division in oogenesis?
- Fertilization by sperm
- Degeneration of the primary oocyte
- Formation of the second polar body
- Entry into the second meiotic division (correct)
What developmental stage characterizes a primary oocyte arrested in prophase I?
What developmental stage characterizes a primary oocyte arrested in prophase I?
A woman nearing menopause has a significant decrease in the number of viable ovarian follicles. How does this directly impact the hormonal regulation of her menstrual cycle?
A woman nearing menopause has a significant decrease in the number of viable ovarian follicles. How does this directly impact the hormonal regulation of her menstrual cycle?
Which of the following is the primary way that estrogens affect cells to promote secondary sex characteristics?
Which of the following is the primary way that estrogens affect cells to promote secondary sex characteristics?
How does the combined action of FSH and estrogen influence the ovarian cycle?
How does the combined action of FSH and estrogen influence the ovarian cycle?
The early growth of the follicle is significantly influenced by follicle-stimulating hormone (FSH). What specific action does FSH have on the ovarian follicle?
The early growth of the follicle is significantly influenced by follicle-stimulating hormone (FSH). What specific action does FSH have on the ovarian follicle?
How does the degeneration of the corpus luteum (luteolysis) initiate a new menstrual cycle if fertilization does not occur?
How does the degeneration of the corpus luteum (luteolysis) initiate a new menstrual cycle if fertilization does not occur?
What change in cervical mucus occurs around ovulation, facilitating sperm penetration?
What change in cervical mucus occurs around ovulation, facilitating sperm penetration?
What is the primary role of the progestins, specifically progesterone, in the female reproductive system?
What is the primary role of the progestins, specifically progesterone, in the female reproductive system?
What is the significance of atresia in the context of the menstrual cycle?
What is the significance of atresia in the context of the menstrual cycle?
Which hormone directly stimulates testosterone production in the theca cells of the ovarian follicle?
Which hormone directly stimulates testosterone production in the theca cells of the ovarian follicle?
Synthesis of 17β-estradiol requires the action of aromatase in granulosa cells. What role does FSH play in this process?
Synthesis of 17β-estradiol requires the action of aromatase in granulosa cells. What role does FSH play in this process?
How does the presence of a fertilized ovum affect the corpus luteum in the ovarian cycle?
How does the presence of a fertilized ovum affect the corpus luteum in the ovarian cycle?
How does inhibition of GnRH release impact the menstrual cycle?
How does inhibition of GnRH release impact the menstrual cycle?
Under what hormonal influence does one of the primordial follicles convert into a graffian follicle during each menstrual cycle?
Under what hormonal influence does one of the primordial follicles convert into a graffian follicle during each menstrual cycle?
What is the direct effect of rising estrogen levels on the uterus during the follicular phase of the menstrual cycle?
What is the direct effect of rising estrogen levels on the uterus during the follicular phase of the menstrual cycle?
What is the process wherein developing follicles involute, later becoming atretic?
What is the process wherein developing follicles involute, later becoming atretic?
What hormonal event triggers ovulation?
What hormonal event triggers ovulation?
How is the corpus luteum affected if fertilization of the ovum does not occur?
How is the corpus luteum affected if fertilization of the ovum does not occur?
A woman is tracking her basal body temperature to predict ovulation. What hormonal effect causes the slight increase in basal body temperature during the luteal phase?
A woman is tracking her basal body temperature to predict ovulation. What hormonal effect causes the slight increase in basal body temperature during the luteal phase?
What process is directly triggered by the luteinizing hormone (LH) surge during the menstrual cycle?
What process is directly triggered by the luteinizing hormone (LH) surge during the menstrual cycle?
During which phase of the uterine cycle does the endometrium thickness begin to increase?
During which phase of the uterine cycle does the endometrium thickness begin to increase?
What event characterizes the secretory phase of the uterine cycle?
What event characterizes the secretory phase of the uterine cycle?
What uterine state characterized by the endometrium breaking down, resulting in menstruation?
What uterine state characterized by the endometrium breaking down, resulting in menstruation?
In a 35-day menstrual cycle, on which day does ovulation typically occur?
In a 35-day menstrual cycle, on which day does ovulation typically occur?
What is the main source of progestron during the luteal phase?
What is the main source of progestron during the luteal phase?
Inhibin B secretion lowers FSH, LH output from where?
Inhibin B secretion lowers FSH, LH output from where?
Where does fertilization typically takes place?
Where does fertilization typically takes place?
Which part of the female reproductive system prepares the female's body to nourish a developing embryo?
Which part of the female reproductive system prepares the female's body to nourish a developing embryo?
Where are ova formed?
Where are ova formed?
What is the name of the lining of the uterus?
What is the name of the lining of the uterus?
Following ovulation, what ovarian structure forms?
Following ovulation, what ovarian structure forms?
Where does the blastula stage of the embryo implant during gestation?
Where does the blastula stage of the embryo implant during gestation?
What structure forms a primordial follicle?
What structure forms a primordial follicle?
At what stage of meiosis are primary oocytes arrested?
At what stage of meiosis are primary oocytes arrested?
How many primordial follicles are formed in the ovary during fetal life?
How many primordial follicles are formed in the ovary during fetal life?
What is the approximate number of primary oocytes that survive until birth?
What is the approximate number of primary oocytes that survive until birth?
Which of the following best describes the role of the fimbriae in the female reproductive system?
Which of the following best describes the role of the fimbriae in the female reproductive system?
How does the structure of the Graafian follicle support its function?
How does the structure of the Graafian follicle support its function?
During the follicular phase, what cellular mechanism is directly promoted by the increase in FSH levels?
During the follicular phase, what cellular mechanism is directly promoted by the increase in FSH levels?
What is the functional significance of the corpus hemorrhagicum in the ovary following ovulation?
What is the functional significance of the corpus hemorrhagicum in the ovary following ovulation?
How does increased estradiol production during the follicular phase affect the hypothalamus and anterior pituitary?
How does increased estradiol production during the follicular phase affect the hypothalamus and anterior pituitary?
What structural change in the uterus is primarily facilitated by the increase in estrogen during the proliferative phase?
What structural change in the uterus is primarily facilitated by the increase in estrogen during the proliferative phase?
Which of the following accurately describes the role of inhibin B in the female reproductive cycle?
Which of the following accurately describes the role of inhibin B in the female reproductive cycle?
What physiological change within the uterus defines the secretory phase of the menstrual cycle?
What physiological change within the uterus defines the secretory phase of the menstrual cycle?
A primary oocyte is characterized by which of the following conditions regarding meiosis?
A primary oocyte is characterized by which of the following conditions regarding meiosis?
What is the primary factor determining whether the corpus luteum will persist beyond its normal lifespan?
What is the primary factor determining whether the corpus luteum will persist beyond its normal lifespan?
What effect does increased progesterone secretion during the luteal phase have on the myometrial cells?
What effect does increased progesterone secretion during the luteal phase have on the myometrial cells?
How does the production of human chorionic gonadotropin (hCG) affect the ovarian cycle?
How does the production of human chorionic gonadotropin (hCG) affect the ovarian cycle?
How do estradiol levels affect the production of cervical mucus around the time of ovulation?
How do estradiol levels affect the production of cervical mucus around the time of ovulation?
With regards to primary follicle growth, describe the growth of the ovum?
With regards to primary follicle growth, describe the growth of the ovum?
What happens 6-9 hours after the Luteinizing Hormone surge?
What happens 6-9 hours after the Luteinizing Hormone surge?
Flashcards
Follicle
Follicle
Cluster of cells surrounding a single egg in the female reproductive system.
Ovulation
Ovulation
Process in which an ovum is released from the ovary.
Ovaries
Ovaries
Where meiosis occurs in the female reproductive system.
Fallopian tubes
Fallopian tubes
Signup and view all the flashcards
Uterus
Uterus
Signup and view all the flashcards
Vagina
Vagina
Signup and view all the flashcards
Cervix
Cervix
Signup and view all the flashcards
Endometrium
Endometrium
Signup and view all the flashcards
Oogenesis
Oogenesis
Signup and view all the flashcards
Granulosa cells
Granulosa cells
Signup and view all the flashcards
Primary oocyte
Primary oocyte
Signup and view all the flashcards
Secondary oocyte
Secondary oocyte
Signup and view all the flashcards
Prophase
Prophase
Signup and view all the flashcards
Menarche
Menarche
Signup and view all the flashcards
Follicular Phase
Follicular Phase
Signup and view all the flashcards
Luteal phase
Luteal phase
Signup and view all the flashcards
Atresia
Atresia
Signup and view all the flashcards
Primary follicle
Primary follicle
Signup and view all the flashcards
Corpus hemorrhagicum
Corpus hemorrhagicum
Signup and view all the flashcards
Ovulation
Ovulation
Signup and view all the flashcards
Follicle-stimulating hormone (FSH)
Follicle-stimulating hormone (FSH)
Signup and view all the flashcards
Granulosa cells
Granulosa cells
Signup and view all the flashcards
Graafian follicle
Graafian follicle
Signup and view all the flashcards
Vesicular Follicles
Vesicular Follicles
Signup and view all the flashcards
Estrogen
Estrogen
Signup and view all the flashcards
Theca cells
Theca cells
Signup and view all the flashcards
6 hours before ovulation
6 hours before ovulation
Signup and view all the flashcards
Shedding of ovum
Shedding of ovum
Signup and view all the flashcards
Estrogen
Estrogen
Signup and view all the flashcards
Ovulation
Ovulation
Signup and view all the flashcards
Luteinizing Hormone
Luteinizing Hormone
Signup and view all the flashcards
Corpus luteum
Corpus luteum
Signup and view all the flashcards
Human Chorionic Gonadotropin
Human Chorionic Gonadotropin
Signup and view all the flashcards
Menses
Menses
Signup and view all the flashcards
Progesterone
Progesterone
Signup and view all the flashcards
Endometrium
Endometrium
Signup and view all the flashcards
Proloferative Phase
Proloferative Phase
Signup and view all the flashcards
Secretory phase
Secretory phase
Signup and view all the flashcards
Estrogen.
Estrogen.
Signup and view all the flashcards
Luetenizing Hormone
Luetenizing Hormone
Signup and view all the flashcards
Follicle stimulating hormone
Follicle stimulating hormone
Signup and view all the flashcards
Progesterone
Progesterone
Signup and view all the flashcards
The primary Sex hormonse.
The primary Sex hormonse.
Signup and view all the flashcards
Progesterone
Progesterone
Signup and view all the flashcards
Estrogen
Estrogen
Signup and view all the flashcards
Corpus luteum & Placenta.
Corpus luteum & Placenta.
Signup and view all the flashcards
Progestron
Progestron
Signup and view all the flashcards
Cuboidal epithelium
Cuboidal epithelium
Signup and view all the flashcards
Ovarian Stroma
Ovarian Stroma
Signup and view all the flashcards
Primordial follicle
Primordial follicle
Signup and view all the flashcards
LH surge
LH surge
Signup and view all the flashcards
Mature graafian follicle
Mature graafian follicle
Signup and view all the flashcards
Study Notes
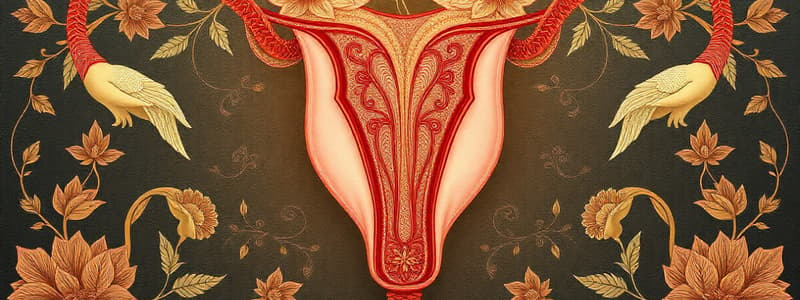
Female Reproductive System Overview
- The main structures are the ovaries, fallopian tubes (oviduct), uterus, vagina, cervix, and endometrium.
- Ovaries, or where meiosis occurs, produce ovums.
- Fallopian Tubes (Oviduct) is where fertilization occurs; after ovulation the ovum moves through the oviduct to the uterus
- The uterus is where the blastula stage of the embryo implants and develops during the 9 month gestation.
- Vagina serves as the birth canal.
- Cervix is the mouth of the uterus.
- Endometrium is the lining of the uterus.
- The female reproductive system prepares the female's body to nourish a developing embryo in addition to producing eggs.
Ovaries and Fallopian Tubes
- Follicles are clusters of cells that surround a single egg in the human female reproductive system.
- Ovulation is the process where an egg (ovum) is released from the ovary.
Ovary
- The Ovary is covered by a single layer of flattened cuboidal epithelium.
- Immature ova (primary oocytes) are present in large numbers in the stroma of the Ovary.
- The Primary Oocyte it surrounded by stromal cells called Granulosa Cells.
- The Primary Oocyte together with the Granulosa Cells forms a primordial follicle.
- At birth, each ovary of a girl has about one million primordial follicles.
- Most of these primordial follicles fail to mature and are lost through atresia.
- During a woman's reproductive years (approximately ages 11-50), she produces only one ovum each month and produces around 400 ova in her lifetime.
Oogenesis and Follicle Development
- A developing egg (oocyte) differentiates into a mature egg (ovum) through a series of steps called oogenesis
- The ova are all formed in fetal life and lie inside primordial follicles.
- As many as 7 million primordial follicles are formed in the ovary during fetal life, but only 2 million are present at birth due to degeneration.
- Only half of the primordial follicles are viable at birth.
- The ova in the primordial follicle undergoes the first phase of I Meiotic division & get arrested in the stage of prophase.
- Oocyte maturation inhibitor secreted from granulosa cells is presumed to be responsible for the arrest in prophase.
- This stage of arrest continue till the period just before the ovulation when the first meiotic division is completed with production of secondary oocyte & first polar body.
- The first polar body degenerates and disappears.
- The secondary oocyte immediately enters into the second meiotic division, which is arrested at metaphase stage until the sperm fertilizes the ovum.
- The second polar body is given off at the time of fertilization.
- The fertilized ovum is now ready to multiply into the new offspring.
- By birth only 2 million primary oocytes survive.
- At puberty this number falls to 300,000
- Only about 400-450 of these attain the mature stage in female reproductive life.
- Most of the ovarian follicles are exhausted at menopause.
- The development of primary oocytes arrests at the prophase stage of meiosis.
- Prophase stage of meiosis in a primary oocyte may persist for a period varying between 11-50 years, as ovulation may occur soon after menarche to just before menopause.
Monthly Ovarian Cycle
- The effects of gonadotrophic hormones (LH and FSH) on ovaries starts with puberty.
- Menarche is the first menstrual cycle.
- The follicular phase lasts approximately 14 (+/- 7) days.
- The luteal phase lasts 14 days.
- The first half of the cycle ie @14 days of the cycle are occupied by development of follicles, called the follicular phase.
- The first stage of follicular growth is moderate enlargement of the ovum, which increases in diameter twofold to threefold.
- The first stage of growth is followed by proliferation of granulosa cells in some follicles which are known as primary follicles.
- The follicle that continue to develop has a cavity filled with follicular fluid & on one side is the ovum surrounded by granulosa cells.
- The granulosa cells are further surrounded by two layers of the theca cells: theca interna and theca externa.
- On the 14th day of the cycle the follicle ruptures, the ovum together with a few surrounding granulosa cells is shed into the abdominal cavity.
- The remaining follicle forms the corpus hemorrhagicum in the ovary.
- Ovulation is the process of ovum being discharged from the follicle.
- The early growth of the follicle results from the action of FSH, a hormone secreted by the anterior pituitary.
- The production of this hormone in childhood is negligible, increasing just before puberty.
- FSH acts on the primordial follicle of the ovary leading to proliferation and growth of granulosa cells & theca interna
- Under the influence of FSH during each menstrual cycle, one of the primordial follicle converts into graffian follicle.
- The early growth of the primary follicle, up to the antral stage, is stimulated mainly by FSH alone.
- More accelerated growth occurs, leading to still larger follicles called vesicular follicles.
- Granulosa cells and theca interna produce estradiol, one of the estrogens.
- Approximately a week or more before ovulation, one follicle outgrows all the others, and the remaining 5 to 11 developing follicles involute (atresia).
- Follicles that involute are said to become atretic
- Atresia normally allows just one follicle to grow large enough each month to ovulate and prevent the development of more than one child with each pregnancy.
- The single follicle reaches a diameter of 1 to 1.5 centimeters at the time of ovulation and is called the mature follicle.
- Estrogen increases the number of FSH receptors on granulosa cells, which in turn leads to the release of more estrogen, resulting in a positive feedback loop.
- The combined action of FSH and Estrogen leads to the expression of LH receptors on granulosa cells & theca cells.
- Availability of LH receptors leads to progesterone secretion towards the end of the follicular phase.
- Theca cells produce testosterone, which is stimulated at the first step by LH
- Testosterone diffuses to the nearby granulosa cells, which contain aromatase and convert testosterone to 17β-estradiol, which is stimulated by FSH
- A primordial follicle develops to the graafian stage, with atresia of neighboring follicles.
- LH and FSH receptors are up-regulated in theca and granulosa cells.
- Estradiol levels increase and cause proliferation of the uterus.
- FSH and LH levels are suppressed by the negative feedback effect of estradiol on the anterior pituitary.
- Progesterone levels are low.
LH Surge for Ovulation
- A finely programmed positive feedback mechanism leads to a sharp rise in LH secretion about 6 hours before ovulation.
- The LH surge is essential for ovulation.
- LH is produced by the basophil cells of the anterior pituitary.
- It acts on mature graafian follicle and leads to shedding of the ovum and conversion of graafian follicle into corpus luteum.
- This hormone is produced continuously in small quantities, but a sudden surge takes place in the middle of the cycle, leading to ovulation.
- The surge is due to positive feedback by oestrogens acting on the hypothalamus & anterior pituitary.
- Ovulation occurs 14 days before the next menses and is regardless of the cycle length.
- In a 28-day cycle, ovulation occurs on day 14; and day 22 for a 35-day cycle.
- A burst of estradiol synthesis at the end of the follicular phase has a positive feedback effect on the secretion of FSH and LH (LH surge).
- Ovulation occurs as a result of the estrogen-induced LH surge.
- Estrogen levels decrease just after ovulation but rise again during the luteal phase.
- Cervical mucus increases in quantity; it becomes less viscous and more penetrable by sperm.
Ovarian Cycle (Luteal Phase)
- A sudden surge of Luteinizing Hormone of the anterior pituitary takes place in the middle of the cycle.
- This hormone acts on the mature graafian follicles on 13 to 15th day of the ovarian cycle & cause rupture of the follicle and shedding of the ovum (ovulation).
- Empty graafian follicle is converted into corpus luteum
- If fertilization of ovum takes place the stage of degeneration is delayed & Corpus Luteum continues to function for 13-14 weeks of pregnancy.
- This is due to production of human chorionic gonadotropins by the trophoblast of the fertilized ovum.
- The placenta takes over the function from copus luteum completely.
Menses/Luteal Phase
- The endometrial is sloughed because of the abrupt withdrawal of estradiol and progesterone.
- The corpus luteum begins to develop, and it synthesizes estrogen and progesterone.
- Vascularity and secretory activity of the endometrium increase to prepare for receipt of a fertilized egg.
- Basal body temperature increases because of the effect of progesterone on the hypothalamic thermoregulatory center.
- If fertilization does not occur, the corpus luteum regresses at the end of the luteal phase and estradiol and progesterone levels decrease abruptly.
- Follicular phase is the first approx 14 days but variable
- An egg develops in follicle during the follicular phase, stimulated by FSH
The Ovarian Cycle
- Estrogen is produced during the follicular phase while the egg develops.
- The ovulation phase: egg is released from the follicle (LH surge) to the abdominal cavity, and gets picked up by fimbria fallopian tube.
- Luteal phase is the postovulatory phase lasts 14 days (more constant, with the corpus luteum develops from exploded follicle
- The corpus luteum develops and the produces progesterone as well as estrogen.
- Progesterone stimulates uterus to be ready for baby
- If there is no pregnancy, the corpus luteum degenerates into corpus albicans.
Uterine Cycle
- Towards the end of menstrual cycle, the corpus luteum degenerates to form corpus albicans.
- The degenerated corpus luteum cannot synthesize much estrogen and progestron.
- Withdrawal of these hormones leads to breakdown of the uterine wall &bleeding, resulting in menstruation .
- Conventionally, the onset of bleeding is considered the beginning of menstrual cycle.
- Bleeding continues for about 4 days.
- By day 5, the ovarian follicle is sufficiently developed to secrete a considerable quantity of estrogen.
- The uterine wall not only starts getting repaired, but also the endometrium thickness starts increasing.
- During menstrual cycle all superficial uterine epithelium is shed
- Accordingly, endometrium response is divided into two phases: proliferative & secretory.
- The Endometrial cycle corresponds to the ovarian cycle & it lasts for 28+/- 7 days
- The shedding of endometrium is due to necrosis of superficial and intermediate zone of endometrium.
- Withdrawal of hormones causes spasm of blood vessels which leads to ischaemic necrosis of the endometrium.
- The blood loss during menstruation is 5-80 ml
- After menstruation (reparative stage), most of the endometrium is lost with only basal layer and basal part of the glands surviving.
- The repair of the endometrium starts during the menstruation by proliferation of basal layer of the endometrium and epithelial lining of the glands.
- The cells of the basal layer proliferate under the influence of estrogen.
- The secretory phase constitutes the last 14 days of menstrual cycle & its duration is remarkably constant.
- During this phase the endometrium becomes thick & hypertropied.
- Glands undergo changes in shape to become elongated & coiled and secrete a thick, viscous glycogen rich fluid.
- The volume of stromal cells cytoplasm is increased during the secretory phase.
- Glycogen and lipid accumulate inside stromal cells & these can provide nourishment to the ovum after fertilization until it establishes alternative nutritive source
Hormonal Control of Menstrual Cycle
- FSH stimulates the development of ovarian follicles and oestrogen secretion from theca interna cells (proliferative changes in endometrium).
- FSH and oestrogen to reach a peak at 12-13 days is called called the oestrogen surge, which responsiveness of pituitary to GnRH which triggers a burst of LH secretion (LH Surge) within 24 hours.
- Ovulation occurs about 6-9 hours after LH Surge. LH is the ovulating Hormone.
- FSH also suddenly peaks at the same time as LH (FSH Surge)
- Serum LH & FSH concentration falls to very low values after ovulation, but as, the corpus luteum is formed, serum progestron levels increase; serum oestrogen & inhibin B also reduce FSH & LH secretion via negative feedback effect on hypothalamus.
- Progestron acts on endometrium primed by oestrogen secretory phase of endometrium development.
- If pregnancy occurs, the corpus luteum persists & continue to secrete Estrogen & Progestron however its function begins to decline after 8 weeks. Failure to secrete those hormones results in spontaneous abortion.
- If there is no fertilization, the corpus luteum regresses causing a sharp fall in levels of progestrone and estrogen to trigger witdrawal bleeding
- Once luteolysis of corpus luteum begins, progestron and estrogen decreases, along with an increase in secretion of FSH & LH to begin a new cycle.
Functions of Ovarian Hormones
- The two types of ovarian sex hormones are estrogens and progestins.
- Estradiol is the most important of the estrogens, and progesterone is the most important progestin.
- Estrogens mainly promote proliferation and growth of specific cells in the body that are responsible for the development of most secondary sexual characteristics of the female.
- Progestins function mainly to Prepare the uterus for pregnancy and the breasts for lactation.
Estrogens
- Three estrogens are present in significant quantities in the plasma of the human female: β-estradiol, estrone, and estriol.
- The principal estrogen secreted by the ovaries is β-estradiol.
- The estrogenic potency of β-estradiol is 12 times that of estrone and 80 times that of estriol.
- β-estradiol is considered the major estrogen, although the estrogenic effects of estrone are not negligible.
- Estrogen stimulates the growth of ovary and follicles local effects.
- Stimulates growth of smooth muscle and proliferation of epithelial linings of reproductive tract. In addition, fallopian tubes increase contractions and ciliary activity, uterus increases contractions and responsiveness to oxytocin and vagina increases layering of cells.
- Estrogen stimulates external genitalia growth, particularly during puberty
- Stimulates breast growth, particularly ducts and fat deposition during puberty
- Stimulates female body configuration development during puberty to include narrow shoulders, broad hips, female fat distribution via deposition on hips and breasts
- Stimulates a more-fluid secretion from lipid (sebum)-producing skin glands ; ("anti-acne" effect opposes the acne-producing effects of androgen.)
- Stimulates bone growth and ultimate cessation of bone growth causing epiphyseal plates to close; protects against osteoporosis; without having an anabolic effect on skeletal muscle
- Deficiency in estrogen creates Vascular effects ("hot flashes")
- Has feedback effects on hypothalamus and anterior pituitary
- Stimulates prolactin secretion but inhibits prolactin's milk-inducing action on the breasts
- Protects against atherosclerosis by effects on plasma cholesterol , blood vessels, and blood clotting
Progestron
- Progestron is provided by the corpus luteum and the placenta.
- They are also provided by the testis and Adrenal Cortex, although in small amounts.
- The plama Level for levels in men are =0.3ng/ml, and for women are =0.09ng/ml During follicular phase of menstrual cycle & increases by 20 folds during luteal phase.
- It is converted to pregnediol in the liver and it conjugated to glucuronic acid and exreted in urine during metabolism.
- Progestrone antagonizes the action of oestrogen.
- It also leads to excitability of myometrial cells, sensitivity of myometrium to oxytocine, and reduction in number of estrogen receptors in the endometrium
- Increases basal body temperature slightly.
- Inhibits ovulation by inhibiting release of GnRH from the hypothalamus with it leading to potency in the inhibitory effect of estrogen on secretion of GnRh.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.