Podcast
Questions and Answers
What role does the theca interna play in the synthesis of estradiol (E2)?
What role does the theca interna play in the synthesis of estradiol (E2)?
- It regulates the activity of granulosa cells through estrogen receptors.
- It converts cholesterol into androgens in response to FSH.
- It directly synthesizes estradiol from cholesterol.
- It produces testosterone in response to LH, serving as a substrate for E2. (correct)
How do granulosa cells synthesize E2?
How do granulosa cells synthesize E2?
- By directly converting cholesterol into E2.
- By converting cholesterol into testosterone.
- By producing androgens in response to LH.
- By converting androgens into E2 upon FSH stimulation. (correct)
What happens when LH binds to theca interna cells?
What happens when LH binds to theca interna cells?
- Cholesterol is converted into androgens through a cascade of events. (correct)
- Testosterone is produced from androgens.
- Granulosa cells undergo mitosis.
- E2 is synthesized directly from cholesterol.
Which hormone directly stimulates the granulosa cells to produce E2?
Which hormone directly stimulates the granulosa cells to produce E2?
Which statement about the anatomy and function of the follicles is correct?
Which statement about the anatomy and function of the follicles is correct?
What is the dominant structure in the ovary during the luteal phase of the estrous cycle?
What is the dominant structure in the ovary during the luteal phase of the estrous cycle?
Which hormone is primarily secreted by the dominant follicle during the follicular phase?
Which hormone is primarily secreted by the dominant follicle during the follicular phase?
What effect does progesterone (P4) have on GnRH release during the luteal phase?
What effect does progesterone (P4) have on GnRH release during the luteal phase?
What hormone is responsible for initiating the recruitment phase of folliculogenesis?
What hormone is responsible for initiating the recruitment phase of folliculogenesis?
What is the primary action of the tonic center in the hypothalamus?
What is the primary action of the tonic center in the hypothalamus?
What process marks the final step of follicular dynamics?
What process marks the final step of follicular dynamics?
During which stage of the estrous cycle is the corpus luteum the dominant structure?
During which stage of the estrous cycle is the corpus luteum the dominant structure?
What initiates the final growth and maturation of the dominant follicles?
What initiates the final growth and maturation of the dominant follicles?
What is the primary purpose of estradiol (E2) during the follicular phase?
What is the primary purpose of estradiol (E2) during the follicular phase?
In which phase does the preovulatory surge of GnRH occur?
In which phase does the preovulatory surge of GnRH occur?
What leads the surge center to release GnRH in a high amplitude surge?
What leads the surge center to release GnRH in a high amplitude surge?
What regulates the secretion of FSH from the anterior pituitary?
What regulates the secretion of FSH from the anterior pituitary?
What happens to most recruited follicles during the recruitment phase of folliculogenesis?
What happens to most recruited follicles during the recruitment phase of folliculogenesis?
During the folliculogenesis process, what does low FSH concentration lead to?
During the folliculogenesis process, what does low FSH concentration lead to?
What is the role of inhibin in ovarian function?
What is the role of inhibin in ovarian function?
Which factor has a primary role in promoting the LH surge leading to ovulation?
Which factor has a primary role in promoting the LH surge leading to ovulation?
In what order do the stages of the estrous cycle occur?
In what order do the stages of the estrous cycle occur?
What is the role of inhibin in folliculogenesis?
What is the role of inhibin in folliculogenesis?
Which process signals the end of luteal phase support for GnRH release?
Which process signals the end of luteal phase support for GnRH release?
What characterizes the basal secretion of GnRH from the tonic center?
What characterizes the basal secretion of GnRH from the tonic center?
Which follicle size classification is correct?
Which follicle size classification is correct?
Which hormones are primarily involved in antral follicle E2 synthesis regulation?
Which hormones are primarily involved in antral follicle E2 synthesis regulation?
What hormone level is typically high during the luteal phase?
What hormone level is typically high during the luteal phase?
What does the surge in LH during the preovulatory phase primarily indicate?
What does the surge in LH during the preovulatory phase primarily indicate?
What is the main function of the preovulatory surge of LH?
What is the main function of the preovulatory surge of LH?
How does the interaction between theca interna and granulosa cells impact folliculogenesis?
How does the interaction between theca interna and granulosa cells impact folliculogenesis?
During the entire estrous cycle, what remains constant in the release of FSH and LH?
During the entire estrous cycle, what remains constant in the release of FSH and LH?
What initiates luteolysis in the estrous cycle?
What initiates luteolysis in the estrous cycle?
Which hormone triggers the final follicular maturation and ovulation?
Which hormone triggers the final follicular maturation and ovulation?
During the estrous cycle, when does the endometrium need to be primed by P4 for E2 to stimulate PGF2⍺ release?
During the estrous cycle, when does the endometrium need to be primed by P4 for E2 to stimulate PGF2⍺ release?
What happens to follicles during the first follicular wave if the P4 levels are high?
What happens to follicles during the first follicular wave if the P4 levels are high?
What effect does increasing concentrations of E2 have on the release of PGF2⍺?
What effect does increasing concentrations of E2 have on the release of PGF2⍺?
What is the role of inhibin during folliculogenesis?
What is the role of inhibin during folliculogenesis?
What does the surge center primarily regulate?
What does the surge center primarily regulate?
How does high P4 affect GnRH release from the tonic center?
How does high P4 affect GnRH release from the tonic center?
What is one requirement for small antral follicles to be recruited?
What is one requirement for small antral follicles to be recruited?
What is the final outcome after the drop in P4 due to luteolysis?
What is the final outcome after the drop in P4 due to luteolysis?
What occurs in the absence of P4 during folliculogenesis?
What occurs in the absence of P4 during folliculogenesis?
How do increasing levels of E2 influence the behavior of the dominant follicle?
How do increasing levels of E2 influence the behavior of the dominant follicle?
What indicates the dominance of a follicle during folliculogenesis?
What indicates the dominance of a follicle during folliculogenesis?
What characterizes the recruitment phase of follicular development?
What characterizes the recruitment phase of follicular development?
What phase follows the formation of spermatids in spermatogenesis?
What phase follows the formation of spermatids in spermatogenesis?
What process allows spermatogonia to revert to stem cells during the proliferation phase?
What process allows spermatogonia to revert to stem cells during the proliferation phase?
Where are the most immature germ cells, called spermatogonia, primarily located?
Where are the most immature germ cells, called spermatogonia, primarily located?
What is the purpose of intercellular bridges during spermatogenesis?
What is the purpose of intercellular bridges during spermatogenesis?
Which of the following statements correctly describes differentiation during the meiotic phase?
Which of the following statements correctly describes differentiation during the meiotic phase?
What happens to the spherical spermatid during spermiogenesis?
What happens to the spherical spermatid during spermiogenesis?
During the meiotic phase, what guarantees genetic diversity in sperm?
During the meiotic phase, what guarantees genetic diversity in sperm?
How many haploid spermatids are produced from one primary spermatocyte after the meiotic phase is complete?
How many haploid spermatids are produced from one primary spermatocyte after the meiotic phase is complete?
Which of the following best describes the structure of a spermatozoon?
Which of the following best describes the structure of a spermatozoon?
During which compartment of the seminiferous tubule do meiosis and differentiation occur?
During which compartment of the seminiferous tubule do meiosis and differentiation occur?
What is the main function of spermatogonial stem cells during spermatogenesis?
What is the main function of spermatogonial stem cells during spermatogenesis?
What happens to developing germ cells as they mature during spermatogenesis?
What happens to developing germ cells as they mature during spermatogenesis?
Which phase of spermatogenesis directly follows the formation of secondary spermatocytes?
Which phase of spermatogenesis directly follows the formation of secondary spermatocytes?
Which statement best describes the role of mitotic division in the proliferation phase of spermatogenesis?
Which statement best describes the role of mitotic division in the proliferation phase of spermatogenesis?
What role do Sertoli cells play in the process of spermatogenesis?
What role do Sertoli cells play in the process of spermatogenesis?
What is the outcome of DNA replication during the meiotic phase?
What is the outcome of DNA replication during the meiotic phase?
What is the primary function of Sertoli cells in the male reproductive system?
What is the primary function of Sertoli cells in the male reproductive system?
How do Leydig cells contribute to male reproductive function?
How do Leydig cells contribute to male reproductive function?
Which hormone regulates the functions of Sertoli and Leydig cells?
Which hormone regulates the functions of Sertoli and Leydig cells?
What is one critical function of testosterone in the male reproductive system?
What is one critical function of testosterone in the male reproductive system?
What is the final phase of spermatogenesis following the formation of spermatids?
What is the final phase of spermatogenesis following the formation of spermatids?
What occurs during the meiotic phase of spermatogenesis?
What occurs during the meiotic phase of spermatogenesis?
What type of cells are B-spermatogonia?
What type of cells are B-spermatogonia?
During which step do A-spermatogonia progress mitotically from A1 to A4?
During which step do A-spermatogonia progress mitotically from A1 to A4?
What is the primary function of Sertoli cells in the male reproductive system?
What is the primary function of Sertoli cells in the male reproductive system?
Which phase of spermatogenesis involves the formation of primary spermatocytes?
Which phase of spermatogenesis involves the formation of primary spermatocytes?
How do gonadotropins affect the function of Leydig cells?
How do gonadotropins affect the function of Leydig cells?
What are the three phases of spermatogenesis?
What are the three phases of spermatogenesis?
During which phase do A-spermatogonia undergo several mitotic divisions?
During which phase do A-spermatogonia undergo several mitotic divisions?
What is a role of estradiol produced by Sertoli cells?
What is a role of estradiol produced by Sertoli cells?
Which statement best describes Leydig cells?
Which statement best describes Leydig cells?
What characterizes the proliferation phase of spermatogenesis?
What characterizes the proliferation phase of spermatogenesis?
What is the primary transformation that occurs during spermiogenesis?
What is the primary transformation that occurs during spermiogenesis?
Which component of a spermatozoon is primarily responsible for motility?
Which component of a spermatozoon is primarily responsible for motility?
How are developing germ cells in the seminiferous tubule connected?
How are developing germ cells in the seminiferous tubule connected?
Where are spermatogonia primarily located within the seminiferous tubule?
Where are spermatogonia primarily located within the seminiferous tubule?
What occurs in the adluminal compartment of the seminiferous tubule?
What occurs in the adluminal compartment of the seminiferous tubule?
What is the result of intercellular bridges during spermatogenesis?
What is the result of intercellular bridges during spermatogenesis?
Which phase of spermatogenesis involves the mitotic divisions of spermatogonia?
Which phase of spermatogenesis involves the mitotic divisions of spermatogonia?
What type of cells are primarily located at the periphery of the seminiferous tubule?
What type of cells are primarily located at the periphery of the seminiferous tubule?
What is the primary role of spermatogonial stem cells during the proliferation phase of spermatogenesis?
What is the primary role of spermatogonial stem cells during the proliferation phase of spermatogenesis?
What happens during meiosis I of spermatogenesis that contributes to genetic diversity?
What happens during meiosis I of spermatogenesis that contributes to genetic diversity?
How many spermatids are formed from one primary spermatocyte after completing the meiotic phase?
How many spermatids are formed from one primary spermatocyte after completing the meiotic phase?
Which cellular process allows spermatogonia to revert to stem cells?
Which cellular process allows spermatogonia to revert to stem cells?
What is the chromosomal configuration of spermatids formed during spermatogenesis?
What is the chromosomal configuration of spermatids formed during spermatogenesis?
Which phase of spermatogenesis involves the transformation of secondary spermatocytes into spermatids?
Which phase of spermatogenesis involves the transformation of secondary spermatocytes into spermatids?
What is one major consequence of stem cell renewal in spermatogenesis?
What is one major consequence of stem cell renewal in spermatogenesis?
During which step are secondary spermatocytes generated from primary spermatocytes?
During which step are secondary spermatocytes generated from primary spermatocytes?
What is the primary function of Sertoli cells in spermatogenesis?
What is the primary function of Sertoli cells in spermatogenesis?
Which hormone binds to Leydig cells and stimulates testosterone production?
Which hormone binds to Leydig cells and stimulates testosterone production?
What is the significant consequence of extended LH secretion on Leydig cells?
What is the significant consequence of extended LH secretion on Leydig cells?
What does inhibin do in relation to FSH secretion?
What does inhibin do in relation to FSH secretion?
Which phase is characterized by the adhesion of spermatids to Sertoli cells?
Which phase is characterized by the adhesion of spermatids to Sertoli cells?
What regulates the release of GnRH in males?
What regulates the release of GnRH in males?
Which of the following compounds produced by Sertoli cells concentrates testosterone in the seminiferous tubules?
Which of the following compounds produced by Sertoli cells concentrates testosterone in the seminiferous tubules?
How often do pulses of LH occur in males within 24 hours?
How often do pulses of LH occur in males within 24 hours?
What protects Leydig cells from the negative feedback of testosterone?
What protects Leydig cells from the negative feedback of testosterone?
Which of the following is NOT produced by Sertoli cells?
Which of the following is NOT produced by Sertoli cells?
Which hormone is primarily responsible for initiating spermatogenesis?
Which hormone is primarily responsible for initiating spermatogenesis?
What is the result of testosterone synthesis being pulsatile?
What is the result of testosterone synthesis being pulsatile?
What role does estradiol play in relation to GnRH release?
What role does estradiol play in relation to GnRH release?
Which substance provides an iron-transport mechanism crucial for spermatogenesis?
Which substance provides an iron-transport mechanism crucial for spermatogenesis?
Which phase of the estrous cycle is characterized by the formation of the corpus luteum?
Which phase of the estrous cycle is characterized by the formation of the corpus luteum?
What is the primary action of LH during the process of ovulation?
What is the primary action of LH during the process of ovulation?
What role does progesterone play during the luteal phase of the estrous cycle?
What role does progesterone play during the luteal phase of the estrous cycle?
How do increasing levels of prostaglandin F2α (PGF2α) affect the estrous cycle?
How do increasing levels of prostaglandin F2α (PGF2α) affect the estrous cycle?
During which stage of oogenesis does the primary oocyte complete meiosis I?
During which stage of oogenesis does the primary oocyte complete meiosis I?
What occurs in the reproductive tract during estrus as a result of high estradiol levels?
What occurs in the reproductive tract during estrus as a result of high estradiol levels?
What is one primary function of progesterone produced during the ovulation process?
What is one primary function of progesterone produced during the ovulation process?
How does prostaglandin E2 (PGE2) facilitate ovulation?
How does prostaglandin E2 (PGE2) facilitate ovulation?
Which statement about oocyte maturation is correct?
Which statement about oocyte maturation is correct?
What anatomical change occurs in the vagina during estrus that aids in copulation?
What anatomical change occurs in the vagina during estrus that aids in copulation?
What role does luteinization play in the ovulation phase?
What role does luteinization play in the ovulation phase?
Which process marks the end of the first meiotic division in oocyte maturation?
Which process marks the end of the first meiotic division in oocyte maturation?
What is one of the primary roles of hyperemia in the reproductive tract during the luteal phase?
What is one of the primary roles of hyperemia in the reproductive tract during the luteal phase?
What initiates collagenase production in the ovulation process?
What initiates collagenase production in the ovulation process?
What is the physiological consequence of estradiol-induced cervical mucus secretion?
What is the physiological consequence of estradiol-induced cervical mucus secretion?
During which phase does the oocyte begin to resume meiosis?
During which phase does the oocyte begin to resume meiosis?
What occurs immediately after the preovulatory surge of LH?
What occurs immediately after the preovulatory surge of LH?
What is the developmental characteristic of oocytes during nuclear arrest?
What is the developmental characteristic of oocytes during nuclear arrest?
What is the primary action of Luteinizing Hormone (LH) in females?
What is the primary action of Luteinizing Hormone (LH) in females?
Which hormone is primarily responsible for lactation?
Which hormone is primarily responsible for lactation?
How does high estrogen levels affect FSH release during the menstrual cycle?
How does high estrogen levels affect FSH release during the menstrual cycle?
What is one of the main functions of follicle-stimulating hormone (FSH) in males?
What is one of the main functions of follicle-stimulating hormone (FSH) in males?
What role does oxytocin play during childbirth?
What role does oxytocin play during childbirth?
Which hormone produced by the anterior pituitary induces the formation of the corpus luteum?
Which hormone produced by the anterior pituitary induces the formation of the corpus luteum?
What hormone promotes milk ejection during breastfeeding?
What hormone promotes milk ejection during breastfeeding?
What primarily triggers the synthesis of prostaglandin F2 alpha (PGF2α)?
What primarily triggers the synthesis of prostaglandin F2 alpha (PGF2α)?
What is the role of receptors on target tissues in hormone action?
What is the role of receptors on target tissues in hormone action?
Which hormone's action requires the presence of specific receptors in target tissues?
Which hormone's action requires the presence of specific receptors in target tissues?
What is a characteristic of peptide hormones?
What is a characteristic of peptide hormones?
How do hormones typically regulate physiological processes?
How do hormones typically regulate physiological processes?
Which of the following is NOT a classification of hormones?
Which of the following is NOT a classification of hormones?
What is the origin of reproductive hormones?
What is the origin of reproductive hormones?
Which statement best describes prostaglandins?
Which statement best describes prostaglandins?
What is the primary function of hormones in reproduction?
What is the primary function of hormones in reproduction?
What mostly influences the biological response of a target cell to a hormone?
What mostly influences the biological response of a target cell to a hormone?
What type of hormone is synthesized from cholesterol?
What type of hormone is synthesized from cholesterol?
What is the main action of relaxin during parturition?
What is the main action of relaxin during parturition?
How does progesterone (P4) affect gonadotropin secretion during the luteal phase?
How does progesterone (P4) affect gonadotropin secretion during the luteal phase?
Which hormone primarily stimulates uterine motility?
Which hormone primarily stimulates uterine motility?
What is the role of inhibin in the reproductive hormone feedback system?
What is the role of inhibin in the reproductive hormone feedback system?
What happens to the secretion of GnRH when estradiol (E2) is high in the absence of progesterone?
What happens to the secretion of GnRH when estradiol (E2) is high in the absence of progesterone?
What is the main action of testosterone in males?
What is the main action of testosterone in males?
What effect does the corpus luteum (CL) have on progesterone levels?
What effect does the corpus luteum (CL) have on progesterone levels?
What feedback mechanism is involved when high levels of progesterone prevent the LH surge?
What feedback mechanism is involved when high levels of progesterone prevent the LH surge?
What action is primarily associated with prostaglandin F2⍺ (PGF2⍺)?
What action is primarily associated with prostaglandin F2⍺ (PGF2⍺)?
How does testosterone influence spermatogenesis?
How does testosterone influence spermatogenesis?
What does the surge center in the hypothalamus regulate during the reproductive cycle?
What does the surge center in the hypothalamus regulate during the reproductive cycle?
Which hormone is produced and acts at the ovaries to enhance uterine motility?
Which hormone is produced and acts at the ovaries to enhance uterine motility?
What is one main action of human chorionic gonadotropin (hCG)?
What is one main action of human chorionic gonadotropin (hCG)?
What occurs during positive feedback in the reproductive hormone regulation?
What occurs during positive feedback in the reproductive hormone regulation?
What source produces inhibin, and its primary action?
What source produces inhibin, and its primary action?
Flashcards are hidden until you start studying
Study Notes
Estrous Cycle Phases
- The estrous cycle is split into two phases: follicular and luteal; they are further divided into four stages: proestrus, estrus, metestrus, and diestrus.
- The follicular phase is characterized by the growth and development of ovarian follicles, with high estradiol and low progesterone.
- The luteal phase is characterized by the presence of a corpus luteum, with high progesterone and low estradiol.
- Ovulation occurs during the transition from the follicular to the luteal phase, usually in metestrus in cows.
- The corpus luteum secretes progesterone while the dominant follicle releases estradiol.
Folliculogenesis
- Folliculogenesis is the continuous process of ovarian follicular growth and degeneration throughout the estrous cycle, except during anestrus.
- Antral follicles are classified based on their diameter into: small (1-5 mm), medium (5.1-7.9 mm), and large (>8 mm).
- Four key processes define follicular dynamics: recruitment, selection, dominance, and ovulation (or atresia).
- Recruitment refers to the emergence of small antral follicles beginning to grow and secrete estradiol.
- Selection involves the deviation of a few follicles to become dominant, while others undergo atresia.
- Dominance signifies the continued growth of the preovulatory follicle(s).
- Ovulation marks the rupture of the preovulatory follicle, releasing the oocyte.
Folliculogenesis Regulation
- The hypothalamus releases GnRH, stimulating the anterior pituitary to produce gonadotropins (FSH and LH).
- FSH triggers follicular recruitment.
- LH promotes final follicle growth and maturation, leading to ovulation.
- The ovary releases inhibin and progesterone, influencing GnRH secretion.
- Estradiol and progesterone act as negative feedback mechanisms on GnRH release, suppressing FSH and LH.
Hypothalamic Centers
- The hypothalamus has two centers for GnRH release: the tonic center for basal secretion and the surge center for preovulatory release.
- The tonic center releases GnRH in small pulses, stimulating basal levels of FSH and LH.
- The surge center is responsible for the release of a surge of LH, causing final follicular growth and ovulation.
- The surge center is sensitive to estradiol, responding with high amplitude GnRH pulses when estradiol exceeds a threshold level.
Steroid Influence on GnRH Release
- During the luteal phase, progesterone inhibits GnRH release from both tonic and surge centers, reducing FSH and LH levels.
- During the follicular phase, the absence of progesterone allows for increased GnRH release, resulting in final follicle growth and ovulation.
- Estradiol above a threshold level triggers a surge of GnRH, ultimately triggering ovulation.
Gonadotropin Regulation and Effects
- FSH is essential for follicular recruitment and estradiol secretion, but its release is inhibited by estradiol and inhibin.
- LH promotes final follicle growth and maturation, and its release is regulated by GnRH pulse frequency.
- Dominant and preovulatory follicles are LH-dependent, although they respond to basal FSH levels.
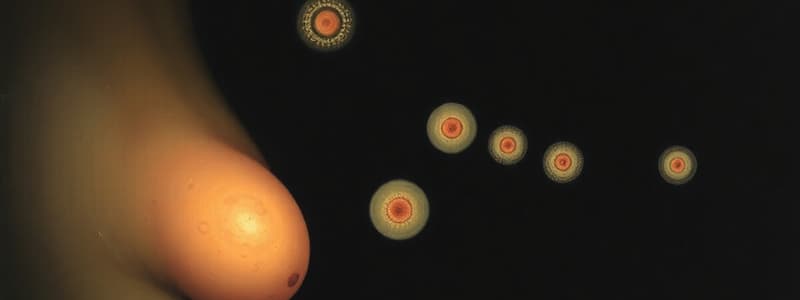
Estradiol Synthesis in Antral Follicles
- Estradiol plays a crucial role in regulating folliculogenesis.
- Estradiol production by antral follicles is regulated by FSH and LH.
- Communication between theca interna and granulosa cells is essential for estradiol production.
Folliculogenesis: Regulation of E2 Synthesis
- Theca interna cells produce androgens (testosterone) in response to LH, which are then converted to E2 by granulosa cells.
- Theca interna cells have LH receptors, while granulosa cells have FSH receptors.
- LH binding to theca interna cells facilitates the conversion of cholesterol into testosterone.
- FSH binding to granulosa cells facilitates the conversion of androgens into E2 through the action of aromatase.
- Dominant follicles also have LH receptors for final maturation.
Luteolysis
- Luteolysis (corpus luteum degeneration) initiates the follicular phase.
- This process stops the secretion of P4 (progesterone) from the corpus luteum, leading to an increase in gonadotropin secretion from the anterior pituitary.
- Luteolysis is induced by PGF2⍺ (prostaglandin F2 alpha) released by the endometrium.
- Rising E2 levels stimulate PGF2⍺ release, but only if the endometrium has been exposed to P4 for a certain period (P4 priming).
Ovarian Folliculogenesis in Waves
- Folliculogenesis occurs in waves, with the first wave not resulting in ovulation (becoming atretic) due to high P4 levels.
- FSH stimulates recruitment but is inhibited by E2 and inhibin from antral follicles.
- Rising E2 stimulates PGF2⍺ release, leading to luteolysis, decreasing P4 and increasing E2, LH and FSH levels.
- LH stimulates final follicle growth and maturation, culminating in ovulation.
Regulation of Folliculogenesis
- Small antral follicles are recruited in response to FSH, producing E2 and inhibin.
- High P4 inhibits GnRH release from both tonic and surge centers, leading to low LH pulse frequency.
- Follicles continue to grow due to basal FSH, while E2 and inhibin levels rise, further reducing FSH release.
- High P4 continues to negatively feedback on the surge center, maintaining low LH pulse frequency.
- One follicle ultimately becomes dominant, secreting enough E2 to stimulate PGF2⍺ release from the P4-primed endometrium.
- PGF2⍺ induces luteolysis, decreasing P4 and removing negative feedback on the hypothalamus.
- E2, freed from P4's influence, stimulates the preovulatory GnRH surge from the surge center, leading to FSH release and the LH surge from the anterior pituitary.
- LH stimulates final follicle growth and ovulation.
- E2 continues to rise, manifesting as estrous behavior, and LH triggers ovulation.
Follicular Phase - Discussion Points
- The four processes of folliculogenesis are recruitment, selection, dominance, and ovulation.
- Recruitment: Initial selection and growth of a pool of follicles.
- Selection: One follicle becomes dominant, suppressing growth of other follicles.
- Dominance: Dominant follicle continues to grow and secrete high levels of E2.
- Ovulation: Rupture of the dominant follicle and release of the egg.
Proliferation Phase
- Stem cell renewal is a key component of the proliferation phase.
- Through the loss of intercellular bridges, some spermatogonia revert to stem cells, ensuring a continuous supply of these cells for the production of new spermatogonia.
- A pool of stem cells is maintained to ensure spermatogenesis continues indefinitely.
- These stem cells undergo mitotic division to create a constant source of A-spermatogonia, sustaining spermatogenesis without interruption for years.
Meiotic Phase
- This phase begins with primary spermatocytes.
- During meiosis I, genetic diversity is ensured through DNA replication and crossing over during the formation of secondary spermatocytes.
- Each sperm cell is genetically distinct from others.
- Meiosis II concludes this phase.
- Secondary spermatocytes transform into spermatids.
Meiotic Phase (Cont.)
- The meiotic divisions generate 4 haploid (1N chromosomal content) spermatids during the meiotic phase of spermatogenesis.
- Each primary spermatocyte produces 4 spermatids.
- Each primary spermatocyte gives rise to 2 secondary spermatocytes, each of which produces 2 spermatids.
Differentiation Phase
- No further cell divisions occur during this phase.
- This stage is also known as "spermiogenesis."
- During this phase, spherical, undifferentiated spermatids undergo a transformation to form fully differentiated, specialized spermatozoa, comprised of:
- A head (containing nuclear material)
- A flagellum including a midpiece (with a mitochondrial helix)
- A principal piece
Spermatogenesis and Location
- The most immature germ cells, spermatogonia, are located at the periphery of a seminiferous tubule near the basement membrane.
- As these cells proliferate, they move toward the lumen, where they are released.
- Developing germ cells are connected by intercellular bridges.
- Groups of spermatogonia, spermatocytes, or spermatids are linked by intracellular bridges, creating cytoplasmic connections within each group.
- These bridges facilitate communication between cells, contributing to synchronized development within a cohort (group of cells).
- Each generation of cells is attached by intercellular cytoplasmic bridges, which divide the generations into cohorts.
Spermatogenesis and Location
- Meiosis and differentiation occur within the adluminal compartment of the seminiferous tubule.
Sertoli and Leydig Cells
- Sertoli cells regulate testosterone production.
- Leydig cells produce testosterone.
Gonadotropins and Sertoli/Leydig Cell Regulation
- Gonadotropins, such as FSH and LH, regulate the functions of Sertoli and Leydig cells.
Testosterone Function
- Testosterone plays various roles within the male reproductive system, including:
- Sperm production
- Development of secondary sexual characteristics
Regulation of GnRH and Gonadotropins Release in Males
- GnRH regulation, along with the release of gonadotropins, is influenced by several factors, including:
- Negative feedback mechanisms
- Feedback loops involving estradiol produced by Sertoli cells.
Spermatogenesis Summary
- Spermatogenesis is the process of producing spermatozoa.
- It occurs within the seminiferous tubules.
- It involves cell divisions and morphological changes in developing germ cells.
- Spermatogenesis is divided into three phases:
- Proliferation phase
- Meiotic phase
- Differentiation phase
Proliferation Phase Summary
- The proliferation phase involves all mitotic divisions of spermatogonia.
- Spermatogonia are the most primitive cells found within the seminiferous epithelium.
- They are specialized diploid cells (2N chromosomal content).
- They reside in the basal compartment of the seminiferous epithelium.
- There are three types of spermatogonia:
- A-spermatogonia
- I-spermatogonia (intermediate)
- B-spermatogonia
Proliferation Phase Summary (Cont.)
- Several generations of A-spermatogonia undergo mitotic divisions, leading to a large number of B-spermatogonia.
- A-spermatogonia progress mitotically from A1 through A4.
- Mitotic divisions of spermatogonia A4 produce I-spermatogonia.
- Mitotic divisions of I-spermatogonia result in B-spermatogonia.
- Ultimately, mitotic divisions of B-spermatogonia give rise to primary spermatocytes.
Endocrinology of Male Reproduction
- The seminiferous tubules and interstitial tissue make up the parenchyma of the testis.
- Sertoli cells reside within seminiferous tubules and function like follicular granulosa cells, depending on FSH.
- Leydig cells, located in interstitial tissue adjacent to the seminiferous tubules, produce testosterone and are equivalent to the theca interna cells.
- Sertoli cells:
- Produce androgen binding protein (ABP), which concentrates testosterone in the seminiferous tubules, supporting spermatogenesis.
- Produce sulfated glycoproteins (SGP-1 and SGP-2).
- SGP-1 aids in fertility acquisition.
- SGP-2 provides a detergent effect for sperm and fluid movement through the testis.
- Produce transferrin, a vital iron-transport protein for successful spermatogenesis.
- Regulate testosterone production by binding to FSH, converting testosterone into estradiol, which inhibits GnRH release by the hypothalamus.
- Produce inhibin, which suppresses FSH production by the anterior pituitary.
- Leydig cells:
- Synthesize testosterone in response to LH.
- Bind to LH, produce progesterone, and convert it into testosterone.
- Respond to LH in short, pulsatile bursts lasting 20-60 minutes.
- Secrete testosterone pulsatile because LH secretion is pulsatile, maintaining adequate testosterone levels.
- If LH secretion becomes constant, Leydig cells reduce LH receptors, resulting in decreased testosterone secretion.
- If LH secretion is prolonged, Leydig cells secrete testosterone for hours, leading to sustained negative feedback on GnRH release and decreased testosterone levels.
- Testosterone is crucial for spermatogenesis, supporting sperm cell meiosis completion, elongated spermatid adhesion to Sertoli cells, and sperm release from seminiferous tubules.
Endocrine Control of Spermatogenesis
- For spermatogenesis, adequate secretion of GnRH, FSH, and LH from the anterior pituitary, and steroid secretion (testosterone and estradiol) are necessary.
- Hypothalamus, in males, lacks a surge center, relying on the tonic center for GnRH release.
- GnRH discharge from the hypothalamus occurs frequently and intermittently in males, unlike females where high amplitude GnRH pulses are released only during the preovulatory surge due to progesterone's negative feedback.
- GnRH bursts in males last several minutes and trigger nearly simultaneous FSH and LH discharges.
- LH episodes last 10-20 minutes and occur 4-8 times daily.
- FSH pulses last 100 minutes and occur 4-8 times daily.
- FSH concentrations are lower but have a longer half-life than LH, due to the testis' relatively constant inhibin production.
Differences in LH between Male and Female
- In males:
- GnRH from the tonic center stimulates LH release.
- Pulsatile LH binds to Leydig cells, producing testosterone.
- LH episodes last 10-20 minutes, occurring 4-8 times daily.
- There is no surge center in the male hypothalamus.
- Progesterone does not regulate GnRH release.
- In females:
- GnRH from the tonic center stimulates basal LH levels throughout folliculogenesis.
- Basal LH levels bind to theca cells to produce testosterone.
- The preovulatory LH surge is stimulated by GnRH from the surge center and regulated by progesterone.
- The LH surge promotes final growth and maturation of dominant follicles and ovulation.
Spermatogenesis
- Spermatogenesis is the process of producing spermatozoa in the seminiferous tubules, involving cell divisions and germ cell morphologic changes.
- It consists of three phases:
- Proliferation phase:
- Includes all mitotic divisions of spermatogonia.
- Spermatogonia are the most primitive cells in the seminiferous epithelium.
- They are diploid cells (2N chromosomal content) located in the basal compartment.
- Three types of spermatogonia exist: A-spermatogonia, I-spermatogonia (intermediate), and B-spermatogonia.
- Several generations of A-spermatogonia undergo mitotic divisions to form B-spermatogonia.
- A-spermatogonia divide mitotically from A1 to A4.
- Spermatogonia A4 mitosis results in I-spermatogonia.
- I-spermatogonia divide mitotically to form B-spermatogonia.
- B-spermatogonia divide mitotically to form primary spermatocytes.
- An important aspect is stem cell renewal.
- Some spermatogonia return to stem cells (spermatogonial stem cells), ensuring stem cell renewal and continuous spermatogenesis.
- Stem cells divide mitotically to provide a continuous source of A-spermatogonia, allowing uninterrupted spermatogenesis over years.
- Meiotic phase:
- Begins with primary spermatocytes.
- Meiosis I involves DNA replication and crossing over, guaranteeing genetic diversity in secondary spermatocyte production.
- This ensures each sperm is genetically unique.
- Meiosis II concludes this phase, converting secondary spermatocytes into spermatids.
- Meiotic divisions produce four haploid (1N chromosomal content) spermatids from each primary spermatocyte.
- Each primary spermatocyte produces two secondary spermatocytes, and each secondary spermatocyte produces two spermatids.
- Differentiation phase:
- No further cell divisions occur, also called "spermiogenesis".
- A spherical spermatid undergoes a transformation into a fully differentiated spermatozoon containing:
- A head (nuclear material).
- A flagellum with a midpiece (mitochondrial helix).
- A principal piece.
- Proliferation phase:
- The most immature germ cells (spermatogonia) are located at the periphery of seminiferous tubules near the basement membrane.
- As these germ cells proliferate, they move towards the lumen.
- Developing germ cells are connected by intercellular bridges.
- Groups of spermatogonia, spermatocytes, or spermatids are interconnected by intercellular bridges.
- These bridges facilitate communication between cells, ensuring synchronized development of a cohort (group of cells).
Sertoli & Leydig Cell Functions
- Sertoli cells:
- Support spermatogenesis by regulating testosterone production (not producing it themselves), producing various supporting substances, and converting testosterone into estradiol.
- Leydig cells:
- Produce testosterone in response to LH, maintaining adequate testosterone levels.
- Gonadotropins regulate Sertoli and Leydig cell functions:
- FSH stimulates Sertoli cell functions, while LH stimulates Leydig cell testosterone production.
Testosterone Functions
- Testosterone is crucial for:
- Completing sperm cell meiosis.
- Adhering elongated spermatids to Sertoli cells.
- Releasing sperm from seminiferous tubules.
Regulation of GnRH and Gonadotropin Release in Males
- GnRH release is primarily regulated by the tonic center in the male hypothalamus.
- Estradiol, produced by Sertoli cells, plays a role in negative feedback on GnRH release by the hypothalamus.
- The tonic center's constant output of GnRH leads to frequent and intermittent GnRH discharges, which in turn trigger FSH and LH release.
- The absence of a surge center in the male hypothalamus means there is no preovulatory GnRH surge like in females.
Learning Objectives
- Understand the functions of estradiol (E2) during the follicular phase.
- Comprehend the process of ovulation.
- Understand the process of oocyte maturation.
- Know how the corpus luteum is formed.
Estrous Cycle
- The estrous cycle is comprised of distinct stages, each characterized by specific hormonal profiles and physiological changes.
- Anestrus: A period of reproductive inactivity, often influenced by environmental factors like seasonality.
- Monoestrus: Animals exhibit a single estrous cycle per year.
- Polyestrus: Animals experience multiple estrous cycles throughout the year.
- Seasonal Polyestrus: Animals exhibit multiple estrous cycles during specific seasons.
Stages of the Estrous Cycle
- Proestrus: Follicles begin to grow and develop, estradiol levels increase.
- Estrus: The period of sexual receptivity, characterized by high levels of estradiol and ovulation.
- Metestrus: The period following estrus, marked by the formation of the corpus luteum and progesterone production.
- Diestrus: The longest stage of the estrous cycle, characterized by high progesterone levels and the preparation for pregnancy.
Folliculogenesis
- Recruitment: A pool of primordial follicles are activated in the ovary.
- Selection: A few recruited follicles are selected for further development.
- Dominance: A single dominant follicle continues to grow and develop.
- Ovulation: The dominant follicle ruptures, releasing the egg.
Hormonal Regulation of the Estrous Cycle
- Gonadotropin-Releasing Hormone (GnRH): Regulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland.
- FSH: Stimulates follicle growth and development, including estradiol production.
- LH: Triggers ovulation and promotes corpus luteum formation and progesterone secretion.
Estradiol Synthesis
- Estradiol is synthesized by the antral follicles.
- FSH: Promotes the production of aromatase, an enzyme that converts testosterone to estradiol.
- LH: Stimulates the production of testosterone.
- Both FSH and LH play critical roles in the production of estradiol.
Hormones and Endocrine Glands
- Hormones are signaling molecules secreted by endocrine glands, delivered to target tissues via the bloodstream, regulating physiology and behavior.
- Endocrine glands are ductless glands that secrete hormones directly into the blood.
- Reproductive hormones are produced by various endocrine glands, including the hypothalamus, pituitary, gonads, uterus, and placenta.
Classification of Hormones
- Hormones are classified based on their biochemical structure:
- Peptides and proteins:
- Peptides are small molecules with < 50 amino acids joined by peptide bonds.
- Proteins are polypeptide chains with > 50 amino acids.
- Glycoproteins: Polypeptide hormones containing carbohydrate moieties.
- Steroids: Synthesized from cholesterol.
- Prostaglandins: Lipids derived from arachidonic acid, consisting of 20-carbon unsaturated hydroxy fatty acids.
- Peptides and proteins:
Target tissues
- Target tissues contain specific receptors for hormones.
- Receptors bind to specific hormones, triggering a specific cellular response.
- Hormone actions require the presence of specific receptors on target cells.
- Only target tissues for a specific hormone can respond to it.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.