Podcast
Questions and Answers
What is the primary goal of performing diagnostic analgesia in lameness investigation?
What is the primary goal of performing diagnostic analgesia in lameness investigation?
- To guide further imaging based on pain source (correct)
- To assess the efficacy of different local anaesthetics
- To desensitize structures distal to the injection site
- To completely eliminate pain before treatment
Which local anaesthetic is described as having the fastest onset and can irritate the skin?
Which local anaesthetic is described as having the fastest onset and can irritate the skin?
- Lidocaine (correct)
- Bupivicaine
- Mepivicaine
- Procaine
When evaluating the success of a diagnostic analgesia procedure, what indicates a positive response?
When evaluating the success of a diagnostic analgesia procedure, what indicates a positive response?
- A minimum of 50% improvement in lameness (correct)
- Less than 50% improvement in lameness
- No visible improvement in lameness
- Complete abolition of lameness
Which sequence is recommended for the investigation of lameness using diagnostic analgesia?
Which sequence is recommended for the investigation of lameness using diagnostic analgesia?
Which local anaesthetic is noted for being the least irritating to the skin?
Which local anaesthetic is noted for being the least irritating to the skin?
What is the generally recommended duration for re-examination following a nerve block?
What is the generally recommended duration for re-examination following a nerve block?
What complications may arise from administering local anaesthesia?
What complications may arise from administering local anaesthesia?
Which method should be used to ensure sterile preparation for intra-synovial analgesia?
Which method should be used to ensure sterile preparation for intra-synovial analgesia?
What is a common result of injecting local anaesthetic too soon after placement?
What is a common result of injecting local anaesthetic too soon after placement?
What is a critical consideration when performing perineural analgesia?
What is a critical consideration when performing perineural analgesia?
What indicates a 'head nod' when assessing lameness?
What indicates a 'head nod' when assessing lameness?
Which of the following describes a common sign of hindlimb lameness?
Which of the following describes a common sign of hindlimb lameness?
What occurs during flexion tests for forelimbs?
What occurs during flexion tests for forelimbs?
In the European Lameness Grading Scale, what does a score of 5 indicate?
In the European Lameness Grading Scale, what does a score of 5 indicate?
What does a positive flexion test indicate?
What does a positive flexion test indicate?
What is a key characteristic of bilateral lameness?
What is a key characteristic of bilateral lameness?
How can severe hindlimb lameness be mistaken for forelimb lameness?
How can severe hindlimb lameness be mistaken for forelimb lameness?
What describes a subtle sign of mild lameness in a horse?
What describes a subtle sign of mild lameness in a horse?
What is the first step when approaching a lame horse?
What is the first step when approaching a lame horse?
Which of the following factors should be included in the history taking of a lame horse?
Which of the following factors should be included in the history taking of a lame horse?
What does palpation focus on during a lameness evaluation?
What does palpation focus on during a lameness evaluation?
During a gait evaluation, which assessment can help determine the lameness severity?
During a gait evaluation, which assessment can help determine the lameness severity?
Why is it important to observe the horse walk in a straight line during a lameness evaluation?
Why is it important to observe the horse walk in a straight line during a lameness evaluation?
How does the surface on which the horse is lunged affect the assessment of lameness?
How does the surface on which the horse is lunged affect the assessment of lameness?
In examining the horse, what does a faulty conformation indicate?
In examining the horse, what does a faulty conformation indicate?
What is the main purpose of incorporating nerve and joint blocks in a lameness investigation?
What is the main purpose of incorporating nerve and joint blocks in a lameness investigation?
What is the appropriate needle size and length for a Tarsometatarsal joint block?
What is the appropriate needle size and length for a Tarsometatarsal joint block?
Which of the following is a common reason for performing a Tarsometatarsal joint block?
Which of the following is a common reason for performing a Tarsometatarsal joint block?
What approach is used for a Digital Flexor Tendon Sheath block?
What approach is used for a Digital Flexor Tendon Sheath block?
How far should the needle be inserted for the deep branch of the lateral plantar nerve block?
How far should the needle be inserted for the deep branch of the lateral plantar nerve block?
What amount of local anesthetic is typically used for the deep branch of the lateral plantar nerve block?
What amount of local anesthetic is typically used for the deep branch of the lateral plantar nerve block?
What is a critical outcome to assess after performing a deep branch of the lateral plantar nerve block?
What is a critical outcome to assess after performing a deep branch of the lateral plantar nerve block?
Which joint compartments should be blocked to ensure proper diffusion of local anesthetic into the stifle?
Which joint compartments should be blocked to ensure proper diffusion of local anesthetic into the stifle?
Which option describes the technique of performing a Tarsometatarsal joint block?
Which option describes the technique of performing a Tarsometatarsal joint block?
Which of the following is a contraindication for performing perineural analgesia?
Which of the following is a contraindication for performing perineural analgesia?
What is the main nerve blocked in a palmar digital nerve block?
What is the main nerve blocked in a palmar digital nerve block?
What structures are desensitized by the abaxial sesamoid nerve block?
What structures are desensitized by the abaxial sesamoid nerve block?
During a low 4-point nerve block, which anatomical landmarks are primarily used?
During a low 4-point nerve block, which anatomical landmarks are primarily used?
What is the correct needle size for performing an abaxial sesamoid nerve block?
What is the correct needle size for performing an abaxial sesamoid nerve block?
Which structure may be desensitized if the palmar digital nerve block is effective?
Which structure may be desensitized if the palmar digital nerve block is effective?
In a distal limb perineural analgesia, which block is used for desensitizing the fetlock joint?
In a distal limb perineural analgesia, which block is used for desensitizing the fetlock joint?
What is the volume of local anesthetic typically used for a palmar digital nerve block?
What is the volume of local anesthetic typically used for a palmar digital nerve block?
Which location is NOT a site for intra-synovial diagnostic analgesia?
Which location is NOT a site for intra-synovial diagnostic analgesia?
What is a risk when placing a low 4-point nerve block too high?
What is a risk when placing a low 4-point nerve block too high?
Which structure is NOT desensitized during a distal interphalangeal joint block?
Which structure is NOT desensitized during a distal interphalangeal joint block?
What is the purpose of rechecking the site after administering a palmar digital nerve block?
What is the purpose of rechecking the site after administering a palmar digital nerve block?
In which block is the needle inserted just proximal to the coronary band?
In which block is the needle inserted just proximal to the coronary band?
Flashcards
Lameness Evaluation
Lameness Evaluation
The process of gathering information about a horse's history, physical condition, and gait to determine the cause of lameness.
Signalment
Signalment
The age, breed, sex, and use of the horse. This information can help narrow down the potential causes of lameness.
Clinical Examination
Clinical Examination
A systematic examination of a horse's body, focusing on areas that may be affected by lameness, such as temperature, tenderness, swelling, and range of motion.
Observation
Observation
Signup and view all the flashcards
Palpation
Palpation
Signup and view all the flashcards
Hoof Tester Examination
Hoof Tester Examination
Signup and view all the flashcards
Gait Evaluation
Gait Evaluation
Signup and view all the flashcards
Flexion Tests
Flexion Tests
Signup and view all the flashcards
Diagnostic Analgesia
Diagnostic Analgesia
Signup and view all the flashcards
Perineural Analgesia
Perineural Analgesia
Signup and view all the flashcards
Intra-synovial Analgesia
Intra-synovial Analgesia
Signup and view all the flashcards
Positive Diagnostic Analgesia
Positive Diagnostic Analgesia
Signup and view all the flashcards
Negative Diagnostic Analgesia
Negative Diagnostic Analgesia
Signup and view all the flashcards
Head nod
Head nod
Signup and view all the flashcards
Asymmetrical pelvis movement
Asymmetrical pelvis movement
Signup and view all the flashcards
Referred Lameness
Referred Lameness
Signup and view all the flashcards
Lameness Assessment on Hard Ground
Lameness Assessment on Hard Ground
Signup and view all the flashcards
European Lameness Grading Scale
European Lameness Grading Scale
Signup and view all the flashcards
AAEP Lameness Grading Scale
AAEP Lameness Grading Scale
Signup and view all the flashcards
Ridden Assessment
Ridden Assessment
Signup and view all the flashcards
Bilateral Lameness
Bilateral Lameness
Signup and view all the flashcards
Recommended Re-examination Time
Recommended Re-examination Time
Signup and view all the flashcards
Pain After Nerve Block
Pain After Nerve Block
Signup and view all the flashcards
Tarsometatarsal (TMT) Joint Block
Tarsometatarsal (TMT) Joint Block
Signup and view all the flashcards
Digital Flexor Tendon Sheath Block
Digital Flexor Tendon Sheath Block
Signup and view all the flashcards
Deep Branch of the Lateral Plantar Nerve Block
Deep Branch of the Lateral Plantar Nerve Block
Signup and view all the flashcards
Stifle Joint Block
Stifle Joint Block
Signup and view all the flashcards
Suspected fracture
Suspected fracture
Signup and view all the flashcards
Skin infection/dermatitis of injection site
Skin infection/dermatitis of injection site
Signup and view all the flashcards
Moderate – severe soft tissue injury
Moderate – severe soft tissue injury
Signup and view all the flashcards
Intra-synovial diagnostic analgesia
Intra-synovial diagnostic analgesia
Signup and view all the flashcards
Palmar/Plantar digital nerve block
Palmar/Plantar digital nerve block
Signup and view all the flashcards
Abaxial sesamoid nerve block
Abaxial sesamoid nerve block
Signup and view all the flashcards
Low 4-point nerve block
Low 4-point nerve block
Signup and view all the flashcards
Distal interphalangeal (coffin) joint block
Distal interphalangeal (coffin) joint block
Signup and view all the flashcards
Navicular bursa block
Navicular bursa block
Signup and view all the flashcards
MCP/MTP (fetlock) joint block
MCP/MTP (fetlock) joint block
Signup and view all the flashcards
Fetlock joint block: Collateral sesamoidean ligament approach
Fetlock joint block: Collateral sesamoidean ligament approach
Signup and view all the flashcards
Low 4-point nerve block
Low 4-point nerve block
Signup and view all the flashcards
Abaxial sesamoid nerve block
Abaxial sesamoid nerve block
Signup and view all the flashcards
Palmar digital nerve block
Palmar digital nerve block
Signup and view all the flashcards
Study Notes
Approach to Equine Lameness Investigation
- The presentation covers a comprehensive approach to investigating lameness in horses.
- Key learning objectives include understanding how to approach a lame horse, describing lameness evaluation, and identifying the use and description of nerve and joint blocks.
History
- Signalment (breed, age, sex) is crucial.
- The horse's use and competition level provide context.
- The perceived problem is vital, as is the onset, duration, and progression of the lameness.
- Previous history, trauma, and medication use are relevant factors.
- Changes in management and farriery practices are also important details.
- The effects of exercise or surface type should be considered.
Clinical Examination
- Observation of obvious clinical signs, posture, conformation, and symmetry is important.
- Faulty conformation is a warning sign, not an unsoundness.
- Palpation, assessing for heat, pain, swelling, effusion, and range of motion, is essential.
- A hoof tester examination is a useful diagnostic tool.
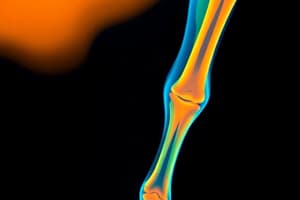
Gait Evaluation
- Gait evaluation involves observing the horse's walk (straight line), trot (straight line), and lunge (in a circle on both soft and hard surfaces).
- Assessing lameness on inside/outside of circle during lunge is important.
- Evaluating lameness through flexion tests and a ridden assessment further helps clarify the diagnosis.
Identifying Lameness
- Lameness is assessed at the walk and trot, looking for distinguishing signs.
- Forelimb lameness might manifest as a head nod or the horse putting less weight on the affected limb.
- Hindlimb lameness can sometimes be identified by an asymmetrical movement of the pelvis ('hip hike' or 'hip drop').
- Gait evaluation during lunging on both soft and hard surfaces is crucial for a thorough diagnosis.
- Flexion tests and a ridden assessment provide more detailed insights into the nature of the lameness.
Identifying Lameness Continued
- Assessing lameness during lunging can provide a better understanding of the specific movement causing the issue.
- Determining if the lameness is worse on hard or soft surfaces helps differentiate between bone and soft tissue issues.
- Flexion tests, identifying pain on specific limb movements, are critical diagnostic procedures.
- The ridden assessment is a final diagnostic input.
Referred Lameness
- Severe hindlimb lameness can sometimes be mistakenly diagnosed as forelimb lameness.
- The horse adapts its weight distribution, mimicking forelimb lameness in its gait.
- Differential diagnostics, including diagnostic analgesia, are necessary to correctly determine the source of the lameness.
Grading Lameness
- The European Lameness Grading Scale (0-10) provides a standardized method to quantify lameness severity observed during a trot.
- Gradations from sound (0) to severe (7-10) based on consistent observation of subtle or marked head/pelvic asymmetry, gait characteristics, and response to specific movements.
- An additional alternative Grading Scale (0-5) defines lameness by factors such as difficulty observing lameness during a walk/trot, gait abnormalities, consistency, and marked movements.
Inertial Measurement Units
- Inertial Measurement Units (IMUs) are increasingly used in equine lameness assessment, objectively measuring head and pelvic movements to quantify the extent of lameness.
- Although helpful, IMUs are not a replacement for a skilled equine practitioner.
Principles of a Lameness Investigation
- The investigation process, including consistent lameness assessment, diagnostic analgesia, diagnosis, and treatment are interwoven.
- Performing these combined factors is crucial for an effective and thorough equine lameness assessment.
Diagnostic Analgesia
- Local anesthetics, including lidocaine, mepivacaine, and bupivacaine, are used to desensitize nerves and block pain signals to pinpoint the painful area.
- The process begins distally and moves proximally through affected areas to accurately identify the source of the pain and aid in imaging directions by the examiner.
Interpreting Diagnostic Analgesia
- Determining if the block worked. Assessing skin sensation, and observing the horse's gait for signs of lameness relief are essential. Assessing any degree of lameness reduction following the block, from 50% to over 75%, is crucial.
- Specific time duration for re-evaluation after a lameness block is important.
- The re-evaluation criteria assist in a more accurate diagnosis.
Preparation for Diagnostic Analgesia
- Thorough preparation is necessary. Adequate restraint, operator safety measures (equipment, like hard hats and sedation tools, short-acting sedation), and clean technique are essential.
Complications and Contraindications
- Potential complications include soft tissue swelling, hematomas, and infections that could be caused by the procedure itself.
- The presence of skin infections, suspected fractures, and moderate-severe tissue injuries are contraindications to diagnostic analgesia.
Perineural Analgesia
- Several specific nerve blocks, including palmar digital, pastern ring, abaxial sesamoid, and low 4-point, are used in the forelimb and hindlimb.
Intra-Synovial Diagnostic Analgesia
- Distal limb, involving joints like the distal interphalangeal, navicular bursa, and metacarpophalangeal, are treated with this technique.
- Upper forelimb and hindlimb areas are similar targets.
Palmar/Plantar Digital Nerve Block
- The site of this block is just proximal to the collateral cartilage, abaxially to the tendon.
- The palpation and injection technique include detailed steps and precautions.
Abaxial Sesamoid Nerve Block
- The site of this block is immediately palmar to the neurovascular bundle at the proximal sesamoid bones.
- Specific techniques for vein artery nerve identification and injection volume are outlined.
Low 4-Point Nerve Block
- The site is distal to the splint bone between the suspensory ligament and the deep digital flexor tendon.
- The procedure, detailed technique, and care for placement near the deep digital flexor tendon sheath are discussed.
Distal Limb Perineural Analgesia Summary
- Overview of the three procedures: Abaxial sesamoid nerve block, low 4-point nerve block, and palmar digital nerve block.
Distal Interphalangeal (Coffin) Joint Block
- Procedure involves injection of local anesthetic targeting the collateral ligaments of the DIP (distal interphalangeal) joint.
- It emphasizes the appropriate placement of the needle.
Navicular Bursa Block
- Correct radiographic alignment of the needle is crucial for effective treatment of navicular spurs.
- Specific steps and considerations during this procedure are emphasized.
MCP/MTP (Fetlock) Joint Block
- Three described approaches are available for the fetlock joint block.
- Specific steps and considerations are emphasized.
Fetlock Joint Block: Collateral Sesamoidean Ligament Approach
- Detailed descriptions of anatomical boundaries, targeting the proximal palmar process of P1, are given.
- Specific directions for inserting the needle along the dorsal aspect and parallel to the ground are outlined.
Tarsometatarsal (TMT) Joint Block
- Considerations for diagnosing Osteoarthritis (OA) of the tarsal joints are discussed.
- Potential communication with the distal intertarsal joint is a factor in some cases.
Digital Flexor Tendon Sheath Block
- Different approaches are described, including approaches targeting the proximal and distal sections of the tendon sheath, and variations in placement.
Deep Branch of the Lateral Plantar Nerve Block
- The lateral approach technique, needle insertion technique, and appropriate volume of local anesthetic are detailed.
Stifle
- The diffusion of local anesthetic between the three joint compartments is emphasized.
- The necessity of specific blocking the three joint compartments is highlighted because diffusion is variable.
- The method of blocking the three compartments is also noted.
Useful Resources and Further Reading
- A list of relevant, credible resources in the field is presented (books, websites).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.