Podcast
Questions and Answers
What percentage of infected individuals with Entamoeba histolytica develop symptomatic disease?
What percentage of infected individuals with Entamoeba histolytica develop symptomatic disease?
- Less than 10% (correct)
- About 50%
- About 25%
- Less than 30%
Which form of Entamoeba histolytica is primarily responsible for the transmission of amebiasis?
Which form of Entamoeba histolytica is primarily responsible for the transmission of amebiasis?
- Cyst (correct)
- Vegetative form
- Trophozoite
- Pseudopod
In which part of the gastrointestinal tract do trophozoites primarily multiply and encyst?
In which part of the gastrointestinal tract do trophozoites primarily multiply and encyst?
- Duodenum
- Large intestine (correct)
- Rectum
- Small intestine
What is the likely consequence of the non-invasive form of Entamoeba histolytica infection?
What is the likely consequence of the non-invasive form of Entamoeba histolytica infection?
Which control measure is effective against Entamoeba histolytica cysts in contaminated water?
Which control measure is effective against Entamoeba histolytica cysts in contaminated water?
What is the primary mode of transmission for the infection caused by E.histolytica?
What is the primary mode of transmission for the infection caused by E.histolytica?
Which factor most directly contributes to the spread of amoebiasis in developing countries?
Which factor most directly contributes to the spread of amoebiasis in developing countries?
During what time frame is the period of communicability for E.histolytica potentially extended?
During what time frame is the period of communicability for E.histolytica potentially extended?
What is indicated as a significant host factor influencing the recurrence of invasive amoebiasis?
What is indicated as a significant host factor influencing the recurrence of invasive amoebiasis?
What environmental condition is most favorable for the survival of cysts of E.histolytica?
What environmental condition is most favorable for the survival of cysts of E.histolytica?
Which population is at an increased risk for sexual transmission of amoebiasis?
Which population is at an increased risk for sexual transmission of amoebiasis?
In which geographical regions is amoebiasis considered a significant health problem?
In which geographical regions is amoebiasis considered a significant health problem?
What is the incubation period for amoebiasis reported to be?
What is the incubation period for amoebiasis reported to be?
Which of the following is true about individuals infected with E.histolytica?
Which of the following is true about individuals infected with E.histolytica?
Which pest is noted for its role in the transmission of amoebiasis?
Which pest is noted for its role in the transmission of amoebiasis?
Flashcards
What is amoebiasis?
What is amoebiasis?
The parasitic infection caused by Entamoeba histolytica, a protozoan that can cause symptoms ranging from mild discomfort to severe dysentery and even liver abscesses.
What is the main mode of transmission of amoebiasis?
What is the main mode of transmission of amoebiasis?
Amoebiasis is mainly transmitted through the fecal-oral route. This occurs when contaminated water, food, or surfaces are ingested, leading to the ingestion of E. histolytica cysts.
What is the invasive stage of Entamoeba histolytica?
What is the invasive stage of Entamoeba histolytica?
The invasive stage of E. histolytica is called the trophozoite. It invades the intestines and can cause ulcers, leading to bloody diarrhea.
What are amoebic cysts?
What are amoebic cysts?
Signup and view all the flashcards
What are some preventive measures for amoebiasis?
What are some preventive measures for amoebiasis?
Signup and view all the flashcards
Reservoir of Entamoeba histolytica
Reservoir of Entamoeba histolytica
Signup and view all the flashcards
How is Entamoeba histolytica transmitted?
How is Entamoeba histolytica transmitted?
Signup and view all the flashcards
What is the infectious stage of Entamoeba histolytica?
What is the infectious stage of Entamoeba histolytica?
Signup and view all the flashcards
How long does it take for Entamoeba histolytica symptoms to show?
How long does it take for Entamoeba histolytica symptoms to show?
Signup and view all the flashcards
What diseases does Entamoeba histolytica cause?
What diseases does Entamoeba histolytica cause?
Signup and view all the flashcards
What are the symptoms of amoebiasis?
What are the symptoms of amoebiasis?
Signup and view all the flashcards
Who is most at risk of Entamoeba histolytica infection?
Who is most at risk of Entamoeba histolytica infection?
Signup and view all the flashcards
Where is Entamoeba histolytica infection most common?
Where is Entamoeba histolytica infection most common?
Signup and view all the flashcards
How is Entamoeba histolytica infection treated and prevented?
How is Entamoeba histolytica infection treated and prevented?
Signup and view all the flashcards
How significant is Entamoeba histolytica infection on a global scale?
How significant is Entamoeba histolytica infection on a global scale?
Signup and view all the flashcards
Study Notes
Amebiasis Overview
- Amebiasis is defined by the WHO as harboring the Entamoeba histolytica protozoan parasite, with or without clinical symptoms.
- The symptomatic disease affects less than 10% of infected individuals, categorized as either intestinal or extraintestinal.
- A small percentage of those with intestinal infections develop invasive amebiasis.
- Intestinal amebiasis ranges from mild abdominal discomfort and diarrhea to severe dysentery.
- Extraintestinal amebiasis involves organs like the liver (abscess), lungs, brain, spleen, and skin
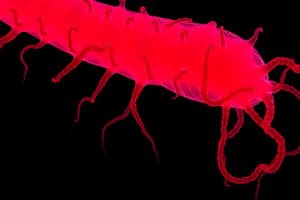
Infectious Agent
- Amebiasis is caused by potentially pathogenic strains of Entamoeba histolytica.
- E. histolytica exists in two forms: vegetative (trophozoite) and cystic.
- Trophozoites multiply and encyst in the colon.
- Cysts are excreted in stool and when ingested, release trophozoites that colonize the large intestine.
- Some trophozoites invade the bowel, causing ulceration, primarily in the cecum, ascending colon, rectum, and sigmoid. Some may enter veins and reach the liver and other organs.
- Trophozoites have a short lifespan outside the human body and aren't crucial for transmission.
- Cysts are infective to humans and remain viable in feces, water, sewage, and soil for several days, especially if moisture and temperature are low.
- Cysts are resistant to chlorine in typical water purification amounts but can be killed by drying, heating to 55°C, or freezing.
Reservoir and Communicability
- Humans are the only reservoir for amebiasis infection.
- Feces containing cysts are the source of infection.
- Most infected individuals are asymptomatic carriers.
- Carriers who handle food present a higher risk.
- Communicability can last several years if infections remain unrecognized and untreated.
Incubation Period
- The incubation period varies from a few days to several months or years.
- An average incubation period is usually 2 to 4 weeks or longer.
Modes of Transmission
- Water contaminated with sewage can cause epidemics, fecal-oral being the dominant transmission mode. Food handlers can play a significant role if they're convalescent or healthy carriers.
- Flies and cockroaches harbor cysts, potentially contaminating food.
- Farm vegetables contaminated by sewage can also transmit the parasite.
- Sexual transmission (oral-anal contact, especially among men who have sex with men) is increasingly reported.
- Poverty, ignorance, and poor sanitation favor the spread in developing countries.
- Hot, dry climates aren't conducive for cyst survival.
Host Factors
- Amebiasis can affect individuals of all ages and sexes equally.
- Amebiasis often occurs as a household infection, with subsequent family members becoming infected.
- Anti-amoebic antibodies are produced during tissue invasion.
- Cell-mediated immunity controls invasive amebiasis recurrence.
Environmental Factors
- Amebiasis is closely tied to poor sanitation and socio-economic status rather than climate.
- In regions with distinct wet-dry seasons, infection rates are higher during rainy seasons, likely because cysts survive longer.
- Epidemic outbreaks often associate with sewage contaminating water supplies.
Epidemiology
-
Amebiasis is a common gastrointestinal infection with worldwide distribution.
-
It's a significant health problem in many regions, including China, Southeast & West Asia, Latin America, and Mexico.
-
Globally, about 500 million people carry E. histolytica in their intestines and approximately one-tenth develop invasive amebiasis.
-
Invasive amebiasis is estimated to cause 40,000 to 100,000 deaths annually.
-
Prevalence rates can be as low as 2% or up to 60% or more in unsanitary areas.
-
High prevalence areas typically see endemic amebiasis, resulting from high transmission and constant reinfection.
-
In developing countries, high incidence correlates with contaminated water sources used for human consumption and in growing/preparing food.
-
Worldwide, approximately 50 million cases of invasive E. histolytica disease occur annually, leading to nearly 100,000 deaths.
-
Infected individuals often remain asymptomatic, highlighting the magnitude of potential cases relative to those presenting with symptoms.
-
Specific risk factors, such as long-term travel, HIV infection, pregnancy, and corticosteroid use, have been linked to heightened amebiasis severity in some populations.
-
Different age groups and sexes are affected differently regarding specific conditions like amebic colitis, with adults more prone to liver abscesses and younger individuals to fulminant colitis.
Clinical Features
- The clinical response to E. histolytica infection can vary.
- Invasive amebiasis leads to dysentery, liver abscess, and pleuropulmonary involvement.
- Involvement of other organs is less common.
- The majority of instances involve non-dysenteric intestinal amebiasis, exhibiting mild symptoms or being asymptomatic.
- Amebic dysentery or acute amebic colitis typically has an 8-10-day incubation period, with sudden onset.
- Symptoms encompass severe abdominal cramps, chills, fever, nausea, headache, and tenesmus.
- Stools are often liquid, contain bloody mucus, and may show leukocytosis.
- Severe cases can be life-threatening.
Diagnosis
- Diagnosis involves microscopic identification of trophozoites or cysts in fresh stool samples, or tissue aspirates.
- Demonstration of red blood cell-containing trophozoites within stool or tissue samples confirms amebiasis.
- Serological tests may not be useful for intestinal amebiasis but can indicate extraintestinal infection.
- Indirect hemagglutination assays are a common diagnostic test.
- Newer techniques such as counterimmunoelectrophoresis and ELISA are also utilized.
Treatment
- Symptomatic intestinal and extraintestinal amebiasis is treated with metronidazole or tinidazole.
- Following initial treatment with metronidazole or tinidazole, individuals are often treated with iodoquinol or paromomycin.
- Asymptomatic E. histolytica carriers are routinely treated with iodoquinol or paromomycin.
- Extensive amebic liver abscesses (>5 cm diameter) are often surgically drained to alleviate pain.
Prevention
- Primary prevention strategies emphasize sanitation practice.
- Safe disposal and proper hygiene are vital.
- Clean water sources and proper food preparation are important.
- Health education regarding risk, mode of transmission, and preventative actions in affected communities is critical.
Case Scenario
- A 24-year-old male patient experiencing frequent bloody stools and pus in stool for three days, increased defecation frequency, abdominal pain, and vomiting, was diagnosed with amebic dysentery.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.