Podcast
Questions and Answers
Which of the following is NOT a known site of occurrence for endometriosis?
Which of the following is NOT a known site of occurrence for endometriosis?
- Urinary bladder
- Lungs (correct)
- Cul-de-sac
- Ovary
Which symptom is part of the classic triad associated with endometriosis?
Which symptom is part of the classic triad associated with endometriosis?
- Dyschezia (correct)
- Increased appetite
- Menorrhagia
- Heavy menstrual bleeding
What is the most common site of endometriosis occurrence?
What is the most common site of endometriosis occurrence?
- Broad ligament
- Ovary (correct)
- Uterosacral ligaments
- Cul-de-sac
During physical examination, which finding is commonly associated with endometriosis?
During physical examination, which finding is commonly associated with endometriosis?
Which diagnostic method is considered definitive for diagnosing endometriosis?
Which diagnostic method is considered definitive for diagnosing endometriosis?
What is a characteristic finding in 'chocolate cysts' seen in endometriosis?
What is a characteristic finding in 'chocolate cysts' seen in endometriosis?
What role does Ca125 play in the context of diagnosing endometriosis?
What role does Ca125 play in the context of diagnosing endometriosis?
Which of the following statements about endometriosis staging is correct?
Which of the following statements about endometriosis staging is correct?
Which of the following is NOT considered a key consideration in the management of endometriosis?
Which of the following is NOT considered a key consideration in the management of endometriosis?
In the management of endometriosis, when should laparoscopy be strongly considered only after a trial of medical treatments?
In the management of endometriosis, when should laparoscopy be strongly considered only after a trial of medical treatments?
What is the most definitive surgical treatment for endometriosis?
What is the most definitive surgical treatment for endometriosis?
What is typically the first-line medical treatment for a patient with endometriosis?
What is typically the first-line medical treatment for a patient with endometriosis?
Which condition is commonly associated with endometriosis and defined as the presence of ectopic endometrial tissue within the myometrium?
Which condition is commonly associated with endometriosis and defined as the presence of ectopic endometrial tissue within the myometrium?
Which symptom is NOT typically associated with endometriosis?
Which symptom is NOT typically associated with endometriosis?
The risk of recurrence of endometriosis is best described as:
The risk of recurrence of endometriosis is best described as:
Which factor should NOT be considered when determining appropriate treatment for endometriosis?
Which factor should NOT be considered when determining appropriate treatment for endometriosis?
Which symptom is least likely to be associated with endometriosis, based on the classic presentation?
Which symptom is least likely to be associated with endometriosis, based on the classic presentation?
Which of the following theories best explains the pathogenesis of endometriosis?
Which of the following theories best explains the pathogenesis of endometriosis?
In what situation is a laparoscopy typically used in the diagnosis of endometriosis?
In what situation is a laparoscopy typically used in the diagnosis of endometriosis?
Which statement regarding the staging of endometriosis is accurate?
Which statement regarding the staging of endometriosis is accurate?
What characteristic feature would you expect to find in a complex adnexal mass on ultrasound consistent with endometriosis?
What characteristic feature would you expect to find in a complex adnexal mass on ultrasound consistent with endometriosis?
Which statement about the classic triad of symptoms in endometriosis is correct?
Which statement about the classic triad of symptoms in endometriosis is correct?
What is a common finding in a physical examination of a patient with endometriosis?
What is a common finding in a physical examination of a patient with endometriosis?
Which of the following is a misconception about Ca125 testing in relation to endometriosis?
Which of the following is a misconception about Ca125 testing in relation to endometriosis?
What are the key medical treatment options for managing endometriosis as a first-line approach?
What are the key medical treatment options for managing endometriosis as a first-line approach?
Which treatment option should be considered if first-line medical treatments fail after diagnosis confirmation through laparoscopy?
Which treatment option should be considered if first-line medical treatments fail after diagnosis confirmation through laparoscopy?
Which statement about the surgical management of endometriosis is true regarding fertility preservation?
Which statement about the surgical management of endometriosis is true regarding fertility preservation?
What factor can impact the risk of recurrence in patients with endometriosis?
What factor can impact the risk of recurrence in patients with endometriosis?
Which condition may present with a tender, enlarged uterus and is often confused with endometriosis?
Which condition may present with a tender, enlarged uterus and is often confused with endometriosis?
Which of the following symptoms is common among patients with endometriosis, according to its clinical findings?
Which of the following symptoms is common among patients with endometriosis, according to its clinical findings?
What is a notable consideration when evaluating the treatment for endometriosis in younger patients?
What is a notable consideration when evaluating the treatment for endometriosis in younger patients?
What is true regarding the lifestyle modifications in the management of endometriosis?
What is true regarding the lifestyle modifications in the management of endometriosis?
Flashcards are hidden until you start studying
Study Notes
Definition
- Endometriosis is a condition where endometrial tissue (typically found in the lining of the uterus) grows outside of the uterus.
- This condition is benign, meaning it is not cancerous.
Occurrence
- Endometriosis affects approximately one-third or more women experiencing chronic pelvic pain.
- Most commonly diagnosed in women in their 30s, who have not given birth, and are infertile.
- However, it can affect women throughout their reproductive years.
Theories of Pathogenesis
- Retrograde menstruation is a leading theory for endometriosis.
- During menstruation, endometrial fragments are transported through the fallopian tubes and implant at various locations within the abdomen.
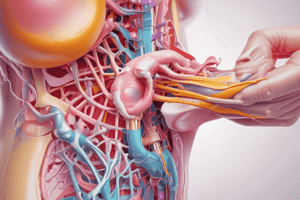
Sites of Occurrence
- Ovaries
- Cul-de-sac
- Uterosacral ligaments
- Broad ligament
- Fallopian tubes
- Round ligaments
- Vagina
- Rectosigmoid and bowel, appendix
- Urinary bladder and ureters
Symptoms
- Dysmenorrhea (painful menstruation)
- Dyspareunia (painful intercourse)
- Dyschezia (pain with bowel movements)
- Cyclic and non-cyclic pelvic pain
- Infertility
- Secondary dysmenorrhea
- Premenstrual and postmenstrual spotting (approximately 20% of cases)
Physical Exam
- No specific sign can definitively confirm endometriosis.
- Common findings include:
- Recto-vaginal exam findings
- Cul-de-sac nodularity and tenderness
- Uterosacral nodularity
- Tender, fixed adnexal mass
- Uterus fixed and retroverted
Diagnosis
- Ruling out other causes is crucial.
- Ultrasound: An adnexal mass with complex echogenicity and internal echoes consistent with blood can be observed.
- Definitive Diagnosis: Visual examination with laparotomy or laparoscopy, and histological confirmation of endometrial tissue.
- Other tests, including Ca125, are not reliable indicators of endometriosis.
Pathology
- "Chocolate cysts" in the ovaries are a common characteristic of endometriosis.
- These cysts are filled with old endometrial shedding and blood, giving them a thick, tarry consistency.
- Ruptured cysts can cause chemical peritonitis.
- Adhesions are a common consequence of endometriosis.
Staging
- A staging system exists for endometriosis, but there is no clear correlation between the stage and the severity or frequency of pain symptoms.
Management Considerations
- Severity of Symptoms
- Extent of the disease
- Desire for future fertility
- Age of the patient
- Threat to the Gastrointestinal or Urinary tract
Treatment Options
- Excision or ablation surgery
- Pelvic physical therapy
- Medications for pain, birth control, and GnRH agonists
- Treatments for co-occurring conditions
- Self-care
Medical Management
- First-line treatment (minimum of three to six months):
- Oral contraceptive pills (OCP’s), cyclic or continuous
- Progestins
- Aromatase inhibitors
- Referral for laparoscopy for diagnosis and treatment if these fail.
- Second-line medical treatments (usually after laparoscopy):
- Mirena IUD (levonorgestrel)
- GnRH agonists (Lupron)
- GnRH agonists should not be administered without prior diagnostic laparoscopy.
- Pain relief alone does not confirm an endometriosis diagnosis.
Surgical Management
- Fertility-preserving:
- Laparoscopy (or rarely, laparotomy) with ablation or excision of endometrial implants and adhesions.
- Endometriomas larger than 3 centimeters in diameter should be surgically removed.
- Most definitive:
- Hysterectomy (often laparoscopic) with ablation or excision of all endometrial implants and adhesions.
- Removal of ovaries was previously a traditional option, but recent studies suggest that preserving ovaries is reasonable in many cases.
- Recurrence is always a risk.
Related Disorder: Adenomyosis
- Ectopic endometrial tissue within the myometrium.
- Typically affects parous women between 35 and 50 years old.
- Symptoms:
- Often asymptomatic
- Secondary dysmenorrhea, abdominal pressure, bloating
- Menorrhagia
- Dyspareunia, sometimes chronic pelvic pain
- Examination findings:
- Diffusely enlarged, globular, tender uterus
- Diagnosis:
- Strong clinical suspicion based on history findings and exam findings
- Characteristic findings on ultrasound and MRI
- Definitive diagnosis confirmed through pathology report.
Bottom Line Concepts
- Endometriosis is most prevalent among women in their reproductive years who are subfertile.
- The exact cause of endometriosis remains uncertain and is likely attributed to a combination of factors.
- Dysmenorrhea, dyspareunia, and dyschezia are the classic symptoms associated with endometriosis.
- The stage of endometriosis does not reliably correlate with the frequency or severity of pain.
- Treatment approaches vary and should consider the severity of symptoms, disease extent, future fertility aspirations, and patient age.
- Endometriosis can reoccur throughout a woman's life.
- Minimizing menstrual flow and suppressing ovarian cycling can reduce the risk and symptoms of endometriosis.
Endometriosis Definition
- Endometrial glands and stroma are found outside the uterine cavity and walls.
- This condition is benign.
Endometriosis Occurrence
- Affects more than one third of women with chronic pelvic pain.
- Most common in women in their 30s.
- Often presents in nulliparous women (women who have never given birth).
- Commonly associated with infertility.
- Can present throughout the reproductive years.
Pathogenesis of Endometriosis
- Endometrial fragments transported through fallopian tubes at time of menstruation and implant at intraabdominal sites.
Endometriosis Sites of Occurrence
- Ovary (most common)
- Cul-de-sac
- Uterosacral ligaments
- Broad ligament
- Fallopian tubes
- Round ligaments
- Vagina
- Rectosigmoid and bowel, appendix
- Urinary bladder and ureters
Endometriosis Symptoms
- Classic Triad: dysmenorrhea (painful menstruation), dyspareunia (painful intercourse), and dyschezia (painful defecation).
- Pain (cyclic and non-cyclic).
- Infertility.
- Secondary dysmenorrhea.
- Premenstrual and postmenstrual spotting.
Physical Exam
- No pathognomonic finding (no “telltale sign”).
- Potential findings:
- Recto-vaginal exam findings.
- Cul-de-sac nodularity and tenderness.
- Uterosacral nodularity.
- Tender, fixed adnexal mass.
- Uterus fixed and retroverted.
Diagnosis
- Rule out other causes.
- Ultrasound – adnexal mass of complex echogenicity, internal echoes consistent with blood.
- Definitive diagnosis:
- Direct visualization (via laparotomy or laparoscopy).
- Histologic and gross findings consistent with endometrial tissue.
- Other tests.
- Ca125 - not specific nor sensitive; not a reliable indicator of endometriosis.
Pathology of Endometriosis
- “Chocolate cysts” of the Ovary:
- Endometrial cysts filled with old endometrial sheddings and blood.
- Typically very tarry and sticky.
- Can cause chemical peritonitis if ruptured .
- These cysts are characteristic of endometriosis.
- Adhesions.
Staging
- A system of staging exists so that caregivers can communicate with each other re: locations of disease.
- There is no clear relationship between stage and frequency and severity of pain symptoms.
Management
- Key considerations:
- Severity of the symptoms.
- Extent of the disease.
- Desire for future fertility.
- Age of the patient.
- Threat to GI or urinary tract.
Endometriosis Treatment Options
- Excision or ablation surgery.
- Pelvic physical therapy.
- Medication for pain, birth control and GnRH agonists.
- Treatments for co-occurring conditions.
- Self-care.
Medical Management
- 1st line treatment (adequate trial of 3-6 months).
- OCP’s , cyclic or continuous.
- Progestins (i.e.MPA or DMPA).
- Aromatase Inhibitors.
- If these are failing, strongly consider laparoscopy to both diagnose and treat the disease.
- 2nd line medical treatments (usually tried after diagnosis confirmed by laparoscopy).
- Mirena IUD (levonorgestrel).
- GnRH agonists (Lupron).
- Should not be done without laparoscopy first.
- Relief of pain does not make the diagnosis of endometriosis.
- GnRH Agonists.
- Monthly or q3 months x 6 months; no more than 2 courses unless patient is on add back therapy.
Surgical Management
- Fertility preserving:
- Laparoscopy (or rarely, laparotomy) with ablation or excision of endometrial implants and adhesions.
- Endometriomas >3 cm in diameter should be removed surgically.
- Most definitive:
- Hysterectomy (most often laparoscopic) with ablation or excision of all endometrial implants and adhesions.
- Removal of ovaries has been traditional, but newer studies suggest retention of ovaries is reasonable in many cases.
- Risk of recurrence:
- Always a risk of recurrence!
Adenomyosis
- This is a related disorder characterized by the presence of ectopic endometrial tissue within the myometrium.
- Who gets this?
- Usually parous women (women who have given birth).
- Predominantly between the ages of 35-50 years old.
- Symptoms:
- Often asymptomatic.
- Secondary dysmenorrhea.
- Abdominal pressure.
- Bloating.
- Menorrhagia.
- Dysparenuia, sometimes chronic pelvic pain.
- Signs on examination:
- Diffusely enlarged, globular, tender uterus.
- Diagnosis:
- High index of suspicion based on clinical history and exam findings.
- Characteristic findings on ultrasound and MRI.
- Definitive dx = Pathology report.
Bottom Line Concepts
- The typical patient with endometriosis is in her reproductive years and sub-fertile.
- Pathogenesis of endometriosis is not completely understood and is probably a combination of factors.
- The characteristic triad of symptoms associated with endometriosis is dysmenorrhea, dyspareunia, and dyschezia.
- Stage of endometriosis is not clearly associated with the frequency and severity of pain symptoms.
- Appropriate treatment varies widely and should take into consideration severity of symptoms, extent of disease, and desire for future fertility.
- There is a risk of recurrence of endometriosis throughout a woman’s life.
- Minimizing menstrual flow and suppressing ovarian cycling can reduce the risk for/symptoms of endometriosis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.