Podcast
Questions and Answers
What mechanism is primarily responsible for the activation of nociceptors during pulpal inflammation?
What mechanism is primarily responsible for the activation of nociceptors during pulpal inflammation?
- Direct innervation by mechanosensitive neurons
- Peripheral sensitization and plasma extravasation (correct)
- Hydrodynamic theory due to fluid movement
- Interaction of odontoblasts with dentinal tubules
Which of the following statements about odontoblasts is true?
Which of the following statements about odontoblasts is true?
- Odontoblasts can act as mechanoreceptors and release ATP. (correct)
- Odontoblasts do not express TRP channels.
- Odontoblasts are not involved in the sensory response.
- Odontoblasts are solely responsible for dentin production.
Which inflammatory mediator is notably increased during pulpal inflammation?
Which inflammatory mediator is notably increased during pulpal inflammation?
- Prostaglandin E2 (PGE2) (correct)
- Interleukin-1 (IL-1)
- Bradykinin
- Tumor necrosis factor-alpha (TNF-α)
What is a limitation of hydrodynamic theory in explaining odontogenic pain?
What is a limitation of hydrodynamic theory in explaining odontogenic pain?
What role do mechanosensitive neurons play in the context of hydrodynamic theory?
What role do mechanosensitive neurons play in the context of hydrodynamic theory?
What type of nerve fibers are primarily responsible for dentinal hypersensitivity?
What type of nerve fibers are primarily responsible for dentinal hypersensitivity?
Which symptom is primarily associated with increased inflammation of the pulp?
Which symptom is primarily associated with increased inflammation of the pulp?
What mechanism leads to sensitization in cases of pulpitis?
What mechanism leads to sensitization in cases of pulpitis?
What characterizes the pain experienced due to exposed dentinal tubules?
What characterizes the pain experienced due to exposed dentinal tubules?
Which of the following increases in response to inflammation of the pulp?
Which of the following increases in response to inflammation of the pulp?
What role do unmyelinated afferents play in tooth pain?
What role do unmyelinated afferents play in tooth pain?
What is NOT a proposed mechanism of dentinal hypersensitivity?
What is NOT a proposed mechanism of dentinal hypersensitivity?
During pulpitis, which response is characterized by the phenomenon of central sensitization?
During pulpitis, which response is characterized by the phenomenon of central sensitization?
Which class of drugs primarily targets cell wall synthesis?
Which class of drugs primarily targets cell wall synthesis?
What is the primary mechanism through which prokaryotic ribosomes are disrupted by certain antibiotics?
What is the primary mechanism through which prokaryotic ribosomes are disrupted by certain antibiotics?
Which antibiotic is known to be effective only against gram-positive bacteria?
Which antibiotic is known to be effective only against gram-positive bacteria?
What contributes to the increase in antibiotic resistance according to the content?
What contributes to the increase in antibiotic resistance according to the content?
What is a characteristic of innate resistance in bacteria?
What is a characteristic of innate resistance in bacteria?
What type of drugs primarily affects nucleic acid synthesis?
What type of drugs primarily affects nucleic acid synthesis?
How do gram-negative bacteria resist beta-lactam antibiotics?
How do gram-negative bacteria resist beta-lactam antibiotics?
What is the estimated annual death toll attributed to antibiotic resistance according to the information provided?
What is the estimated annual death toll attributed to antibiotic resistance according to the information provided?
What is the recommended prophylactic dose of amoxicillin before a dental procedure?
What is the recommended prophylactic dose of amoxicillin before a dental procedure?
Which of the following is NOT a common risk factor for opportunistic infections?
Which of the following is NOT a common risk factor for opportunistic infections?
Which type of antibiotic is considered bactericidal?
Which type of antibiotic is considered bactericidal?
What procedure is NOT typically associated with a high incidence of bacteraemia?
What procedure is NOT typically associated with a high incidence of bacteraemia?
Which antibiotic is typically prescribed for patients with immediate hypersensitivity to penicillin?
Which antibiotic is typically prescribed for patients with immediate hypersensitivity to penicillin?
What type of reaction requires sensitization and is a common concern with antibiotic use?
What type of reaction requires sensitization and is a common concern with antibiotic use?
Which condition is associated with rheumatic heart disease?
Which condition is associated with rheumatic heart disease?
Which antibiotic has a broad spectrum of activity and is commonly used in dental prescriptions?
Which antibiotic has a broad spectrum of activity and is commonly used in dental prescriptions?
What is a potential side effect of antibiotic use?
What is a potential side effect of antibiotic use?
Which of the following groups is most likely to need prophylactic antibiotic therapy before dental procedures?
Which of the following groups is most likely to need prophylactic antibiotic therapy before dental procedures?
What is a common factor contributing to periodontal infections?
What is a common factor contributing to periodontal infections?
Which organism is classified as an opportunistic pathogen related to dental infections?
Which organism is classified as an opportunistic pathogen related to dental infections?
What type of antibiotic is typically bacteriostatic?
What type of antibiotic is typically bacteriostatic?
Which group of drugs represented the majority of dental prescriptions in 2022?
Which group of drugs represented the majority of dental prescriptions in 2022?
What is the primary reason for water flossers being recommended?
What is the primary reason for water flossers being recommended?
Which of the following practices can treat sensitive teeth?
Which of the following practices can treat sensitive teeth?
What should be done with overhangs on restorations?
What should be done with overhangs on restorations?
Which statement is accurate regarding periodontitis progression?
Which statement is accurate regarding periodontitis progression?
What is a significant environmental risk factor for periodontal disease?
What is a significant environmental risk factor for periodontal disease?
How should the tongue be cleaned to avoid a gag reflex?
How should the tongue be cleaned to avoid a gag reflex?
What characteristic of dental pulp indicates it is a richly vascularized organ?
What characteristic of dental pulp indicates it is a richly vascularized organ?
Which factor can contribute to difficulties in maintaining oral hygiene?
Which factor can contribute to difficulties in maintaining oral hygiene?
What is the main purpose of dental fluoride treatment?
What is the main purpose of dental fluoride treatment?
What type of nerve fibers are most sensitive to pain in the dental pulp?
What type of nerve fibers are most sensitive to pain in the dental pulp?
What action is recommended if a patient shows signs of gingival bleeding during toothbrushing?
What action is recommended if a patient shows signs of gingival bleeding during toothbrushing?
Why is cleaning of removable partial dentures important?
Why is cleaning of removable partial dentures important?
What should be avoided to ensure effective wedging in dental restorations?
What should be avoided to ensure effective wedging in dental restorations?
Which of the following is a benefit of tongue cleaning?
Which of the following is a benefit of tongue cleaning?
Flashcards are hidden until you start studying
Study Notes
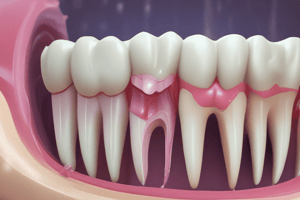
Endodontics
- Dental pulp is a soft connective tissue composed of cells (odontoblasts, fibroblasts, and others), vessels, and nerves
- Pulp innervation is provided by three types of trigeminal sensory nerve fibers: A-beta, A-delta, and C fibers
- A-beta (5%) and A-delta (15%) are myelinated with fast conduction speeds and low excitability thresholds
- C fibers (80%) are unmyelinated with slow conduction speeds and high excitability thresholds
- Pulp is richly vascularized - blood flow and plasma extravasation increase in inflamed pulp, leading to local delivery of protein-bound drugs like NSAIDs
- Central sensitization can occur alongside peripheral sensitization in response to pulpitis
Odontogenic Pain
- Myelinated afferents innervate dentinal tubules, causing sharp, bright, and stabbing pain in dentinal hypersensitivity
- Unmyelinated afferents terminate in the perivascular regions of the pulp, leading to dull aching and throbbing pain in pulpitis
- Pulpitis is primarily a localized infection by microorganisms, which can indirectly activate nociceptors through inflammatory mediators
- Increased levels of prostaglandin E2 (PGE2) are associated with pain
Mechanisms of Tooth Pain
- Hydrodynamic theory - relies on the proximity of mechanosensitive neurons to fluid movement within dentinal tubules
- Direct innervation - hydrodynamic theory doesn't account for the full range of activation seen in odontogenic pain
- Neuroplasticity - involves peripheral sensitization and plasma extravasation
- Odontoblasts as mechanoreceptors - odontoblasts express TRP channels and release signals like ATP
- Brush the outer tooth surface, then the inner tooth surface, then the chewing surface - disadvantage of non-alcohol versions is that they don't work as well
Dental Prescriptions
- In 2022, there were approximately 1.17 million dental prescriptions
- Top 15 prescribed drugs included 7 antibiotics and 1 antifungal
Infective Endocarditis
- Risk factors for infective endocarditis include repeated Group A Strep infections, Strep throat, impetigo, scabies, acute rheumatic fever, and bacteremia following dental procedures
- Acute rheumatic fever can cause an autoimmune response damaging heart valves, leading to rheumatic heart disease
- Prophylactic therapy is recommended for patients with high risk of adverse outcomes from infective endocarditis:
- Artificial heart valves
- History of infective endocarditis
- Congenital heart conditions
- Transplant with valve problems
- Recommended dose is 2g amoxicillin orally 1 hour before procedure, or clindamycin for immediate hypersensitivity to penicillin
- Prophylactic therapy is not required for all procedures, only those with high incidence of bacteremia (e.g., extractions, scaling and root planing)
- Oral hygiene of patient is important, including full mouth probing for patients with periodontitis
- Not recommended for restorations, LA administration, or probing healthy teeth
Choice of Antibiotics for Infections
- Narrow spectrum: penicillin V and amoxicillin
- Broad spectrum: co-amoxyclav (Augmentin), azithromycin, metronidazole, clindamycin
- Bactericidal: metronidazole, penicillin
- Bacteriostatic: trimethaprim, sulfonamides, tetracycline, azithromycin
- Odontogenic Infections:
- Prevotella resistant to penicillin (Russia, Romania, Europe)
- Dentists are the second largest prescriber of antibiotics
- Increase in misuse and overuse of antibiotics due to:
- Antibiotics used as feed additives in agriculture
- Antibiotic-resistant genes as markers in GMO crops
- Antibiotic Resistance:
- WHO declared it one of the top 10 global public health threats
- 70% of HCAI are resistant to at least one common antibiotic
- Increase in community-acquired infection resistance
- Contributes to 700,000 deaths per year
Mechanisms of Antibiotic Resistance
- Innate Resistance:
- No mechanism to transport the drug into the cell
- Do not contain or rely on the antibiotic's target process or protein (e.g., gram- bacteria naturally resistant to beta-lactams)
- Acquired Resistance:
- Microorganisms develop genetic mutations to resist antibiotics
Mechanisms of Drug Action
- Drugs that affect cell wall synthesis - target peptidoglycan
- Beta-lactams and cephalosporins (penicillin and flucloxacillin)
- Glycopeptides (vancomycin - only effective against gram-positive bacteria)
- Drugs that affect protein synthesis - prokaryote ribosomes are different from human ribosomes, interfering with mRNA binding to ribosomes during translation
- Aminoglycosides, tetracyclines, macrolides, chloramphenicol, clindamycin
- Drugs that affect nucleic acid synthesis: structure of DNA is identical in prokaryotes and eukaryotes
- Target enzymes absent in eukaryotes
- E.g., quinolones
Adverse Reactions to Antibiotics
- Unexpected or unintended effects: headaches, vomiting, liver or kidney injury
- Dose-related effects: extension or side effects
- Allergic reactions: require sensitization (e.g. S. Pyogenes, clindamycin-resistant Group B strep)
Oral Hygiene
- Toothpaste:
- Fluoride
- Low abrasion
- Spit, don't rinse
- Can treat sensitive teeth or bleach teeth
- Alternatives: tea tree, bicarbonate, xylitol
- Tongue cleaning:
- Reduces organisms, tongue coating, and halitosis
- Water flossers:
- Alternative to flossing for those with limited dexterity or oral appliances
- Unclear effectiveness at plaque control
Factors Affecting Oral Hygiene Maintenance
- Patient factors:
- Motivation
- Manual dexterity
- Self-esteem
- Tooth anatomy:
- Crowding
- Tooth surface/position in jaw
- Proximity to frenum
- Recession
- Deep grooves
- Plaque retentive anatomy
Partial Dentures
- Thorough cleaning is necessary, especially abutment teeth and clasps
- Nighttime wear can result in gingival inflammation
Iatrogenic Dental Disease (from dental interventions)
- Open contacts
- Over or under contouring restorations
- Crowns and Bridges:
- Margins should be seamless with no gaps or overhangs to retain plaque
- Subgingival margins are harder to clean
- Restoration overhangs:
- Need to be removed or replaced
- Plaque retentive
- Avoid overhangs with effective wedging
Periodontitis Prevention
- All periodontitis is preceded by gingivitis, but not all gingivitis progresses to periodontitis
- Subgingival plaque can stimulate a destructive immune response in susceptible individuals
- Risk factors for periodontitis:
- Diabetes (type 1 and 2)
- Smoking
- Smoking cessation decreases the risk of periodontitis to levels seen in non-smokers
Early Detection of Periodontitis
- Gingival bleeding during toothbrushing
- Change in gingival color (redness) or shape (swelling)
- Persistent halitosis (bad breath) or bad taste
- Receding gums
- Tooth mobility or movement
- Bleeding gums are the earliest sign and should not be ignored
Mouthwash Treatment
- Chlorhexidine mouthwash for moderate-to-severe periodontitis:
- SRP + amoxicillin / metronidazole
- Prophylaxis:
- Used to be commonly used to reduce risk of infective endocarditis
- Side effects and risk of resistance
- Prescribe for patients with cardiac conditions with high risk of adverse outcomes
- C. Glabrata (less common):
- Opportunistic pathogen
- Risk factors:
- Very old or very young
- Poor health
- Overuse of antibiotics
- HIV infection or AIDS
- Chemotherapy or immunosuppressive drugs
- Taking steroid medication
- Diabetic with high blood sugar
- Poorly fitting dentures
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.