Podcast
Questions and Answers
What is a key factor that can lead to diseases related to endocrine glands?
What is a key factor that can lead to diseases related to endocrine glands?
- Excessive or insufficient hormone secretion (correct)
- Abnormalities in nerve function
- Inconsistent levels of glucose metabolism
- Deficiencies in blood vessel health
Which feature distinguishes Type 1 diabetes from Type 2 diabetes?
Which feature distinguishes Type 1 diabetes from Type 2 diabetes?
- Type 1 diabetes primarily affects older adults
- Type 1 diabetes is associated with increased weight gain
- Type 1 diabetes develops insidiously over time
- Type 1 diabetes often has an acute onset (correct)
What is the primary method for diagnosing diabetes mellitus?
What is the primary method for diagnosing diabetes mellitus?
- Evaluating liver enzymes
- Measuring blood electrolyte levels
- Assessing kidney function
- Blood glucose testing (correct)
What is the fasting plasma glucose level indicative of diabetes mellitus?
What is the fasting plasma glucose level indicative of diabetes mellitus?
What process is commonly involved in the regulation of hormone secretion?
What process is commonly involved in the regulation of hormone secretion?
Which statement best describes Type 2 diabetes?
Which statement best describes Type 2 diabetes?
What is the purpose of using grey-topped tubes in blood glucose testing?
What is the purpose of using grey-topped tubes in blood glucose testing?
When might a Glucose Tolerance Test be required?
When might a Glucose Tolerance Test be required?
What is a primary characteristic of primary endocrine diseases?
What is a primary characteristic of primary endocrine diseases?
What treatment options are available for prolactinoma?
What treatment options are available for prolactinoma?
Which of the following is a common clinical sign of hyperprolactinemia in men?
Which of the following is a common clinical sign of hyperprolactinemia in men?
How is hormone secretion regulated in the human body?
How is hormone secretion regulated in the human body?
What is a common clinical sign of hyperprolactinemia in women?
What is a common clinical sign of hyperprolactinemia in women?
What is the primary diagnostic method for insulinoma?
What is the primary diagnostic method for insulinoma?
How does primary hypothyroidism affect TSH and T4 levels?
How does primary hypothyroidism affect TSH and T4 levels?
What characterizes the cortisol secretion in relation to daily rhythms?
What characterizes the cortisol secretion in relation to daily rhythms?
Which of the following symptoms is commonly associated with hyperthyroidism?
Which of the following symptoms is commonly associated with hyperthyroidism?
What is a potential role of the hypothalamic/pituitary/adrenal axis during stress?
What is a potential role of the hypothalamic/pituitary/adrenal axis during stress?
In the context of glycated haemoglobin (HbA1c), what does it specifically indicate?
In the context of glycated haemoglobin (HbA1c), what does it specifically indicate?
What is the most common cause of spontaneous hypoglycemia related to insulin excess?
What is the most common cause of spontaneous hypoglycemia related to insulin excess?
What distinguishes primary hyperthyroidism from primary hypothyroidism?
What distinguishes primary hyperthyroidism from primary hypothyroidism?
Which statement about the components of the hypothalamic/pituitary/thyroid axis is correct?
Which statement about the components of the hypothalamic/pituitary/thyroid axis is correct?
What is the role of cortisol in metabolism?
What is the role of cortisol in metabolism?
Which electrolyte imbalance is typically associated with Addison's Disease?
Which electrolyte imbalance is typically associated with Addison's Disease?
What is the minimum increase in cortisol that indicates a normal response in the Short Synacthen Test?
What is the minimum increase in cortisol that indicates a normal response in the Short Synacthen Test?
Which of the following statements about Cushing's syndrome is NOT correct?
Which of the following statements about Cushing's syndrome is NOT correct?
In Cushing's syndrome caused by ectopic ACTH production, how does cortisol impact ACTH levels?
In Cushing's syndrome caused by ectopic ACTH production, how does cortisol impact ACTH levels?
What role does the 24-hour urine cortisol excretion test play in diagnosing Cushing's syndrome?
What role does the 24-hour urine cortisol excretion test play in diagnosing Cushing's syndrome?
What is a common outcome seen in Cushing's syndrome caused by a pituitary adenoma after administering the Prolonged Dexamethasone Suppression Test?
What is a common outcome seen in Cushing's syndrome caused by a pituitary adenoma after administering the Prolonged Dexamethasone Suppression Test?
What condition can result from excess growth hormone (GH) in adults?
What condition can result from excess growth hormone (GH) in adults?
How does the presence of adrenal tumors affect ACTH levels in Cushing's syndrome?
How does the presence of adrenal tumors affect ACTH levels in Cushing's syndrome?
What could indicate a likely diagnosis of Cushing's syndrome based on a random cortisol test?
What could indicate a likely diagnosis of Cushing's syndrome based on a random cortisol test?
What does increased growth hormone (GH) stimulate in the liver?
What does increased growth hormone (GH) stimulate in the liver?
What is the primary reason why random levels of growth hormone (GH) are not helpful in diagnosing acromegaly?
What is the primary reason why random levels of growth hormone (GH) are not helpful in diagnosing acromegaly?
What hormone from the hypothalamus is responsible for stimulating growth hormone release?
What hormone from the hypothalamus is responsible for stimulating growth hormone release?
What is the expected response to the oral glucose suppression test in normal individuals?
What is the expected response to the oral glucose suppression test in normal individuals?
What is the main cause of high serum prolactin levels?
What is the main cause of high serum prolactin levels?
What physiological role does prolactin play during pregnancy?
What physiological role does prolactin play during pregnancy?
What is the first-line diagnostic test for evaluating growth hormone deficiency?
What is the first-line diagnostic test for evaluating growth hormone deficiency?
Which medical condition commonly leads to elevated prolactin levels?
Which medical condition commonly leads to elevated prolactin levels?
What would be suggested if other causes of hyperprolactinemia are ruled out?
What would be suggested if other causes of hyperprolactinemia are ruled out?
What test utilizes glucagon to evaluate growth hormone deficiency?
What test utilizes glucagon to evaluate growth hormone deficiency?
What are common clinical signs of hyperprolactinemia in women?
What are common clinical signs of hyperprolactinemia in women?
What is a primary characteristic of secondary endocrine diseases?
What is a primary characteristic of secondary endocrine diseases?
What is the main treatment strategy for a prolactinoma?
What is the main treatment strategy for a prolactinoma?
How do endocrine diseases typically arise?
How do endocrine diseases typically arise?
What determines the necessity for dynamic function tests in diagnosing endocrine disorders?
What determines the necessity for dynamic function tests in diagnosing endocrine disorders?
What typically occurs in terms of sodium and potassium levels in Addison's disease?
What typically occurs in terms of sodium and potassium levels in Addison's disease?
What does a very high ACTH level indicate in the context of Cushing's syndrome?
What does a very high ACTH level indicate in the context of Cushing's syndrome?
What outcome is expected from the Prolonged Dexamethasone Suppression Test in patients with Cushing's syndrome caused by a pituitary source?
What outcome is expected from the Prolonged Dexamethasone Suppression Test in patients with Cushing's syndrome caused by a pituitary source?
Why is measuring random cortisol levels generally ineffective in diagnosing Cushing's syndrome?
Why is measuring random cortisol levels generally ineffective in diagnosing Cushing's syndrome?
What does a low cortisol level before the Short Synacthen Test typically indicate?
What does a low cortisol level before the Short Synacthen Test typically indicate?
What is one of the clinical features associated with Cushing's syndrome?
What is one of the clinical features associated with Cushing's syndrome?
Which statement is true regarding cortisol suppression in ectopic ACTH syndrome?
Which statement is true regarding cortisol suppression in ectopic ACTH syndrome?
What is a common cause of Cushing's syndrome originating from the adrenal glands?
What is a common cause of Cushing's syndrome originating from the adrenal glands?
What may the combination of low sodium and high potassium levels indicate in a patient's clinical presentation?
What may the combination of low sodium and high potassium levels indicate in a patient's clinical presentation?
In the case of adrenal tumors in Cushing's syndrome, how does ACTH typically present?
In the case of adrenal tumors in Cushing's syndrome, how does ACTH typically present?
What type of feedback mechanism is primarily involved in regulating hormone secretion?
What type of feedback mechanism is primarily involved in regulating hormone secretion?
Which of the following is a distinguishing factor of Type 2 diabetes compared to Type 1 diabetes?
Which of the following is a distinguishing factor of Type 2 diabetes compared to Type 1 diabetes?
Which blood glucose testing tool is used specifically to prevent glucose metabolism by blood cells?
Which blood glucose testing tool is used specifically to prevent glucose metabolism by blood cells?
What is the plasma glucose level indicative of diabetes when fasting plasma glucose is measured?
What is the plasma glucose level indicative of diabetes when fasting plasma glucose is measured?
Which of the following symptoms is commonly associated with Type 1 diabetes?
Which of the following symptoms is commonly associated with Type 1 diabetes?
What is an important consideration when diagnosing diabetes using random plasma glucose levels?
What is an important consideration when diagnosing diabetes using random plasma glucose levels?
What characterizes the onset of Type 2 diabetes?
What characterizes the onset of Type 2 diabetes?
In a Glucose Tolerance Test, how is plasma glucose evaluated after glucose administration?
In a Glucose Tolerance Test, how is plasma glucose evaluated after glucose administration?
What is a common soft tissue manifestation that indicates acromegaly?
What is a common soft tissue manifestation that indicates acromegaly?
What is the expected GH response during the oral glucose suppression test in a person with acromegaly?
What is the expected GH response during the oral glucose suppression test in a person with acromegaly?
What condition is commonly associated with elevated levels of IGF-1?
What condition is commonly associated with elevated levels of IGF-1?
How does GHRH levels change in individuals suffering from acromegaly?
How does GHRH levels change in individuals suffering from acromegaly?
What is generally the initial step in managing hyperprolactinemia?
What is generally the initial step in managing hyperprolactinemia?
What physiological role does prolactin play during pregnancy?
What physiological role does prolactin play during pregnancy?
Which factor can cause an increase in prolactin levels aside from physiological conditions?
Which factor can cause an increase in prolactin levels aside from physiological conditions?
What test involves glucagon to diagnose growth hormone deficiency?
What test involves glucagon to diagnose growth hormone deficiency?
Why is the random level of GH considered ineffective for diagnosing acromegaly?
Why is the random level of GH considered ineffective for diagnosing acromegaly?
What is a rare cause of short stature that is specifically linked to growth hormone issues?
What is a rare cause of short stature that is specifically linked to growth hormone issues?
What mechanism leads to the symptoms of primary hypothyroidism?
What mechanism leads to the symptoms of primary hypothyroidism?
Which hormone is primarily responsible for stimulating the synthesis of cortisol in response to stress?
Which hormone is primarily responsible for stimulating the synthesis of cortisol in response to stress?
What is a common biological effect of cortisol on metabolism?
What is a common biological effect of cortisol on metabolism?
What distinguishes primary hyperthyroidism from primary hypothyroidism regarding negative feedback?
What distinguishes primary hyperthyroidism from primary hypothyroidism regarding negative feedback?
What is the role of proinsulin measurement in diagnosing insulinoma?
What is the role of proinsulin measurement in diagnosing insulinoma?
How does an increase in cortisol influence blood volume and pressure?
How does an increase in cortisol influence blood volume and pressure?
Which hormone's levels decrease as a direct consequence of primary hyperthyroidism?
Which hormone's levels decrease as a direct consequence of primary hyperthyroidism?
What happens to the levels of T4 and T3 in primary hypothyroidism?
What happens to the levels of T4 and T3 in primary hypothyroidism?
What laboratory investigations are most effective for diagnosing thyroid disease?
What laboratory investigations are most effective for diagnosing thyroid disease?
What physiological state is induced by spontaneous hypoglycemia associated with insulin excess?
What physiological state is induced by spontaneous hypoglycemia associated with insulin excess?
Flashcards are hidden until you start studying
Study Notes
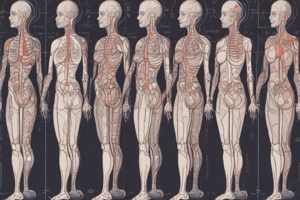
Endocrine Glands and Hormones
- Endocrine glands secrete hormones into the bloodstream, regulating physiological processes in other organs.
- Diseases arise from excessive or insufficient hormone levels.
- Hormone secretion is mainly regulated by negative feedback mechanisms.
Diabetes Mellitus
- Most common endocrine disease in the UK, affecting about 7% of the population.
- Type 1 diabetes symptoms include weight loss, tiredness, polyuria, polydipsia, and typically has an acute onset.
- Type 2 diabetes shares symptoms with Type 1 but is often linked to increased weight and has a slower onset.
- Diagnosis involves blood glucose testing using grey-topped tubes with fluoride and EDTA.
Blood Glucose Testing
- Fasting plasma glucose of 7.0 mmol/L or more indicates diabetes mellitus.
- Random plasma glucose exceeding 11.1 mmol/L can also indicate diabetes.
- Glucose Tolerance Test involves measuring plasma glucose after taking 75 g of glucose and is used when needed.
Glycated Haemoglobin (HbA1c)
- HbA1c indicates average glucose levels over the previous 2-3 months, useful for diagnosis and monitoring control.
Insulinoma
- Insulinoma is a benign tumor causing spontaneous hypoglycemia.
- Diagnosis involves prolonged fasting and measuring proinsulin, insulin, and C-peptide levels during hypoglycemia.
- Treatment options include surgery or oral diazoxide.
Hypothalamic/Pituitary Axis
- Endocrine regulation involves the hypothalamic/pituitary/end-organ axis with hormones like TSH, LH, and FSH.
- The hypothalamus releases TRH, stimulating the pituitary to release TSH which promotes thyroid hormone production.
Thyroid Disorders
- Primary hypothyroidism leads to low T4 and T3 levels despite elevated TSH due to inadequate feedback.
- Symptoms of hypothyroidism: weight gain, dry skin, fatigue, constipation, and slowed cognitive function.
- Primary hyperthyroidism results in high T4 and T3 levels and low TSH, with symptoms including weight loss, fast heart rate, and increased nervous activity.
Investigations for Endocrine Disorders
- Hormone measurement is key for thyroid, pituitary, and gonadal disorders, but less reliable for adrenal disorders.
- Dynamic Function Tests assess axes function.
Adrenal Gland Functions
- Adrenal cortex produces essential hormones such as cortisol, which regulates blood volume, pressure, and metabolic processes.
- Primary adrenal insufficiency (Addison's Disease) can arise from auto-immunities or infections like TB, leading to low cortisol levels.
Addison's Disease
- Symptoms include lethargy, skin pigmentation changes, abdominal pain, dehydration, and low blood sodium.
- Diagnosis involves cortisol and electrolyte measurements and the Short Synacthen Test.
Cushing's Syndrome
- Characterized by excessive cortisol production; causes can be at the hypothalamus (high CRH), pituitary (high ACTH), or adrenal (tumors).
- Diagnosis includes ACTH levels to pinpoint etiologies and 24-hour urine cortisol tests to check cortisol production.
- Treatment depends on identifying the underlying cause.
Growth Hormone Disorders
- Excessive growth hormone (GH) in children causes gigantism; in adults, it leads to acromegaly.
- Acromegaly symptoms: coarse facial features, increased shoe/ring size, along with soft tissue thickening.
- Diagnosing GH disorders involves measuring levels of IGF-1 and conducting oral glucose suppression tests.
Prolactin and Hyperprolactinemia
- Prolactin is produced in the anterior pituitary, vital for breast development and milk production.
- Increased prolactin levels can result from stress, medications, or primary hypothyroidism.
- Hyperprolactinemia symptoms vary between men and women, characterized by galactorrhea and menstrual issues in women and impotence in men.
Endocrine Disease Overview
- Endocrine disorders are primarily caused by variations in hormone secretion.
- Primary endocrine diseases stem from direct target organ dysfunction, while secondary are due to pituitary dysfunction.
- Diagnosis may require various tests, including single blood tests or more complex dynamic function assessments.
Endocrine Glands and Hormones
- Endocrine glands secrete hormones into the bloodstream, regulating physiological processes in other organs.
- Diseases arise from excessive or insufficient hormone levels.
- Hormone secretion is mainly regulated by negative feedback mechanisms.
Diabetes Mellitus
- Most common endocrine disease in the UK, affecting about 7% of the population.
- Type 1 diabetes symptoms include weight loss, tiredness, polyuria, polydipsia, and typically has an acute onset.
- Type 2 diabetes shares symptoms with Type 1 but is often linked to increased weight and has a slower onset.
- Diagnosis involves blood glucose testing using grey-topped tubes with fluoride and EDTA.
Blood Glucose Testing
- Fasting plasma glucose of 7.0 mmol/L or more indicates diabetes mellitus.
- Random plasma glucose exceeding 11.1 mmol/L can also indicate diabetes.
- Glucose Tolerance Test involves measuring plasma glucose after taking 75 g of glucose and is used when needed.
Glycated Haemoglobin (HbA1c)
- HbA1c indicates average glucose levels over the previous 2-3 months, useful for diagnosis and monitoring control.
Insulinoma
- Insulinoma is a benign tumor causing spontaneous hypoglycemia.
- Diagnosis involves prolonged fasting and measuring proinsulin, insulin, and C-peptide levels during hypoglycemia.
- Treatment options include surgery or oral diazoxide.
Hypothalamic/Pituitary Axis
- Endocrine regulation involves the hypothalamic/pituitary/end-organ axis with hormones like TSH, LH, and FSH.
- The hypothalamus releases TRH, stimulating the pituitary to release TSH which promotes thyroid hormone production.
Thyroid Disorders
- Primary hypothyroidism leads to low T4 and T3 levels despite elevated TSH due to inadequate feedback.
- Symptoms of hypothyroidism: weight gain, dry skin, fatigue, constipation, and slowed cognitive function.
- Primary hyperthyroidism results in high T4 and T3 levels and low TSH, with symptoms including weight loss, fast heart rate, and increased nervous activity.
Investigations for Endocrine Disorders
- Hormone measurement is key for thyroid, pituitary, and gonadal disorders, but less reliable for adrenal disorders.
- Dynamic Function Tests assess axes function.
Adrenal Gland Functions
- Adrenal cortex produces essential hormones such as cortisol, which regulates blood volume, pressure, and metabolic processes.
- Primary adrenal insufficiency (Addison's Disease) can arise from auto-immunities or infections like TB, leading to low cortisol levels.
Addison's Disease
- Symptoms include lethargy, skin pigmentation changes, abdominal pain, dehydration, and low blood sodium.
- Diagnosis involves cortisol and electrolyte measurements and the Short Synacthen Test.
Cushing's Syndrome
- Characterized by excessive cortisol production; causes can be at the hypothalamus (high CRH), pituitary (high ACTH), or adrenal (tumors).
- Diagnosis includes ACTH levels to pinpoint etiologies and 24-hour urine cortisol tests to check cortisol production.
- Treatment depends on identifying the underlying cause.
Growth Hormone Disorders
- Excessive growth hormone (GH) in children causes gigantism; in adults, it leads to acromegaly.
- Acromegaly symptoms: coarse facial features, increased shoe/ring size, along with soft tissue thickening.
- Diagnosing GH disorders involves measuring levels of IGF-1 and conducting oral glucose suppression tests.
Prolactin and Hyperprolactinemia
- Prolactin is produced in the anterior pituitary, vital for breast development and milk production.
- Increased prolactin levels can result from stress, medications, or primary hypothyroidism.
- Hyperprolactinemia symptoms vary between men and women, characterized by galactorrhea and menstrual issues in women and impotence in men.
Endocrine Disease Overview
- Endocrine disorders are primarily caused by variations in hormone secretion.
- Primary endocrine diseases stem from direct target organ dysfunction, while secondary are due to pituitary dysfunction.
- Diagnosis may require various tests, including single blood tests or more complex dynamic function assessments.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.