Podcast
Questions and Answers
What is the function of the pleuroperitoneal membranes during diaphragm development?
What is the function of the pleuroperitoneal membranes during diaphragm development?
- To separate the thoracic and abdominal cavities completely
- To serve as a barrier preventing herniation of organs
- To form the central tendon of the diaphragm without fusion
- To provide a connective tissue scaffold for migrating muscle cells (correct)
What results from a failure of muscle cells to populate the pleuroperitoneal membranes?
What results from a failure of muscle cells to populate the pleuroperitoneal membranes?
- Separation of the thoracic and abdominal cavities
- Congenital diaphragmatic hernias (correct)
- Formation of the serous membranes
- Development of the pericardioperitoneal canals
Which embryonic layer is primarily responsible for forming the diaphragm?
Which embryonic layer is primarily responsible for forming the diaphragm?
- Ectoderm
- Epiblast
- Endoderm
- Mesoderm (correct)
What forms the central tendon of the diaphragm during its development?
What forms the central tendon of the diaphragm during its development?
What is the dorsal mesentery's primary function in relation to the gut tube?
What is the dorsal mesentery's primary function in relation to the gut tube?
What is the effect of the different growth rates of the dorsal and ventral borders of the stomach during development?
What is the effect of the different growth rates of the dorsal and ventral borders of the stomach during development?
During stomach rotation, which direction does the dorsal border move?
During stomach rotation, which direction does the dorsal border move?
What is the role of the ventral mesogastrium in developing the liver?
What is the role of the ventral mesogastrium in developing the liver?
Which structure connects the spleen to the posterior abdominal wall?
Which structure connects the spleen to the posterior abdominal wall?
As the stomach rotates, what happens to the omental bursa?
As the stomach rotates, what happens to the omental bursa?
Which characteristic is true for water-soluble vitamins compared to lipid-soluble vitamins?
Which characteristic is true for water-soluble vitamins compared to lipid-soluble vitamins?
What is one of the specific reactions catalyzed by the coenzymes of Vitamin B2?
What is one of the specific reactions catalyzed by the coenzymes of Vitamin B2?
Which of the following statements about Vitamin B3 coenzymes is correct?
Which of the following statements about Vitamin B3 coenzymes is correct?
What is a notable effect of the high toxicity potential of lipid-soluble vitamins?
What is a notable effect of the high toxicity potential of lipid-soluble vitamins?
Which of the following vitamins is directly involved in the electron transport chain (ETC) through its coenzyme?
Which of the following vitamins is directly involved in the electron transport chain (ETC) through its coenzyme?
Why are coenzymes less likely to diffuse across cell membranes compared to vitamins?
Why are coenzymes less likely to diffuse across cell membranes compared to vitamins?
Which type of vitamins can most readily diffuse across cell membranes?
Which type of vitamins can most readily diffuse across cell membranes?
What is the primary reason a coenzyme cannot convert back into a vitamin?
What is the primary reason a coenzyme cannot convert back into a vitamin?
Which of the following statements is true regarding coenzymes?
Which of the following statements is true regarding coenzymes?
How does the size and structure of vitamins compare to coenzymes?
How does the size and structure of vitamins compare to coenzymes?
Which vitamin form acts as the coenzyme in B6-related reactions?
Which vitamin form acts as the coenzyme in B6-related reactions?
Which process is B6 involved in to help convert an amino acid into NAD+?
Which process is B6 involved in to help convert an amino acid into NAD+?
Which of the following B6-assisted reactions is crucial for neurotransmitter synthesis?
Which of the following B6-assisted reactions is crucial for neurotransmitter synthesis?
What is the major role of vitamin B6 in the glycogenolysis process?
What is the major role of vitamin B6 in the glycogenolysis process?
Which addition helps form the phosphorylated form of B6 necessary for absorption?
Which addition helps form the phosphorylated form of B6 necessary for absorption?
What is the primary role of B6 in the glucose-alanine cycle?
What is the primary role of B6 in the glucose-alanine cycle?
Which amino acid is synthesized from homocysteine and serine?
Which amino acid is synthesized from homocysteine and serine?
What is a key function of the glucose-alanine cycle in muscle metabolism?
What is a key function of the glucose-alanine cycle in muscle metabolism?
Which statement about the desaturation of fatty acids in relation to B6 is correct?
Which statement about the desaturation of fatty acids in relation to B6 is correct?
How might increased levels of homocysteine affect cardiovascular health?
How might increased levels of homocysteine affect cardiovascular health?
Flashcards are hidden until you start studying
Study Notes
Mesenteries and Septum Transversum
- The visceral and parietal layers connect as the dorsal mesentery, running from the posterior body wall to the gut tube.
- The ventral mesentery spans from the anterior body wall to the gut tube, existing from the caudal foregut to the upper duodenum.
- The septum transversum is a thick mesodermal tissue located between the thoracic cavity and yolk sac, derived from visceral (splanchnic) mesoderm.
- This septum doesn't separate the thoracic and abdominal cavities, leaving pericardioperitoneal canals.
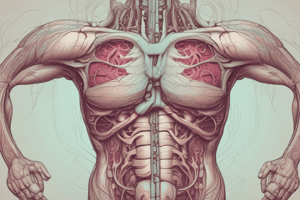
Diaphragm Development
- The diaphragm closes the opening between the future pleural and peritoneal cavities via pleuroperitoneal folds, which later fuse with mesentery to form crura of the diaphragm.
- It develops from:
- Two pleuroperitoneal membranes.
- Muscular components from somites at C3-C5.
- The mesentery of the esophagus.
- Congenital diaphragmatic hernias occur in 1 in 2,000 births due to muscle cell deficiencies preventing myoblast migration.
Stomach Development
- The stomach emerges as a fusiform enlargement of the caudal foregut, with differential growth creating greater (dorsal) and lesser (ventral) curvatures.
- It rotates 90° clockwise around its long axis, positioning the anterior border to the right and the posterior border to the left.
- The left vagus nerve innervates the anterior wall, while the right vagus nerve innervates the posterior wall.
Mesenteries and Organs
- The dorsal mesogastrium connects the stomach to the dorsal body wall, and the ventral mesogastrium connects it to the ventral body wall.
- Components derived from the ventral mesogastrium include the peritoneum around the liver, lesser omentum, and falciform ligament.
- The spleen begins forming from the dorsal mesogastrium in the 5th week and attaches to the posterior body wall via the lienorenal ligament and to the stomach by the gastrolienal ligament.
Pancreas Development
- The pancreas develops from pancreatic buds arising from the caudal foregut; the ventral bud fuses with the dorsal bud during the duodenum's rotation.
- An annular pancreas occurs when the ventral bud forms a ring around the duodenum, potentially causing obstruction.
Midgut Development
- The midgut is suspended by an elongated mesentery, supplied by the Superior Mesenteric Artery (SMA).
- It forms a U-shaped loop, expanding into the umbilical cord due to limited abdominal space.
- Key structures include small intestine sections, cecum, appendix, ascending colon, and the upper two-thirds of the transverse colon.
Intestinal Rotation and Fixation
- The midgut loop experiences two counterclockwise rotations, totaling 270°, returning to the abdomen around the 10th week.
- Various intestines and structures become retroperitoneal due to pressure against the posterior abdominal wall, while some retain their mesentery.
Hindgut Development
- The hindgut includes the left third of the transverse colon, descending colon, sigmoid colon, rectum, and parts of the urinary system, all supplied by the Inferior Mesenteric Artery.
- The cloaca, the endpoint of the hindgut, is segmented into a urogenital sinus and a rectum by the urorectal septum.
Congenital Conditions
- Congenital omphalocele involves persistent herniation of intestinal loops into an umbilical cord.
- Gastroschisis results from the anterior abdominal wall's incomplete closure, causing visceral protrusion into the amniotic cavity.
- Meckel's diverticulum arises from the yolk stalk, potentially inflamed and mimicking appendicitis.
Additional Conditions
- Umbilical fistula forms when the vitelline duct remains patent, permitting communication between umbilicus and intestine.
- Vitelline cyst occurs from the transformation of the vitelline duct's ends into fibrous cords while the middle part develops into a cyst.
Overall Outcomes
- Understand vitamin absorption, conversion, and usage for optimal health.
- Apply biochemical mechanisms of vitamins to treatment of specific conditions.
Intro Objectives
- Classify vitamins into water-soluble and lipid-soluble categories.
- Contrast absorption, transport, storage, excretion, toxicity, and dosing between the two types.
- Discuss mechanisms leading to vitamin deficiencies.
B-Vitamin Coenzymes
- B-vitamins converted to coenzymes that catalyze specific biochemical reactions.
- Vitamin B2 (Riboflavin) forms FAD and FMN; key in various metabolic pathways.
Reactions for B2 and B3 Coenzymes
- B2 (Riboflavin):
- FAD reduces during:
- Citric acid cycle (succinate to fumarate)
- Fatty acid oxidation
- Electron transport chain (ETC) contributing to ATP production.
- FAD reduces during:
- B3 (Niacin):
- NAD+ reduces during:
- Glycolysis and citric acid cycle
- Lipid and amino acid metabolism.
- ETC generating ATP from NADH.
- NAD+ reduces during:
Vitamin vs. Coenzyme
- Vitamins are smaller, simpler molecules that can sometimes diffuse across membranes, especially if lipid-soluble.
- Coenzymes are larger, more complex and often charged, making diffusion across membranes less likely.
- Coenzymes cannot revert back to their vitamin forms, marking a unidirectional metabolic process.
FMN and Energy Production
- FMN acts as a prosthetic group in Complex I of the ETC.
- FMN reduces to FMNH2 during electron transfer, important for ATP synthesis.
Functions of B2 (Riboflavin)
- Participates in antioxidant regeneration, specifically glutathione.
- Aids in neurotransmitter metabolism, important for degrading neurotransmitters like dopamine and norepinephrine.
Physiological Effects of B3 (Niacin)
- Reduces fibrinogen levels, enhancing blood flow by preventing clot formation.
- Improves lipid profiles by decreasing VLDL/LDL and increasing HDL levels.
- Acts on adipose tissue to impact lipolysis and lipid metabolism, reducing LDL levels.
Pantothenic Acid (Vitamin B5)
- Key in energy production and synthesis reactions including fatty acids and cholesterol.
- Coenzyme A (CoA) is the most common form derived from B5, fundamental for several metabolic pathways.
- Plays a role in the Citric Acid Cycle (CAC), beta-oxidation of fatty acids, and production of heme for hemoglobin synthesis.
CoA Functions
- Acetyl-CoA serves as a vital substrate in energy production via the CAC.
- CoA essential for fatty acid activation during beta-oxidation.
- Succinyl-CoA and HMG-CoA derived from CoA are critical for cholesterol and ketone body synthesis.
Key Takeaways
- Knowledge of vitamin absorption and coenzyme functioning is necessary for understanding their roles in health and disease.
- B-vitamins significantly contribute to energy metabolism and antioxidant defenses, playing critical roles in physiological processes.
Vitamin B6 (Pyridoxine) Functions
- Facilitates transamination, trans- and de-sulfhydration, and decarboxylation reactions.
- Exists in six interchangeable forms known as "vitamers," differing only by their functional groups.
- Key vitamers include pyridoxal (PL), pyridoxine (PN), and pyridoxamine (PM); the coenzyme form is pyridoxal phosphate (PLP).
- Other B-vitamins assist in converting vitamers; B2 specifically converts PNP to PLP, the only active coenzyme.
Absorption and Metabolism of B6
- Phosphorylated vitamers must undergo dephosphorylation for absorption.
- Enzymes required for conversion include phosphatases for absorption and kinases to convert PL to PLP.
- B6 plays a crucial role in energy metabolism by synthesizing NAD+ from the amino acid tryptophan.
Glycogenolysis and Gluconeogenesis
- B6 aids glycogen phosphorylase to release glucose for energy during glycolysis.
- In gluconeogenesis, B6 facilitates conversions of amino acids:
- Cysteine to pyruvate.
- Aspartate to oxaloacetate.
- Alanine to pyruvate, linking to the glucose-alanine cycle.
Role in Heme Synthesis
- B6 condenses succinyl CoA with glycine, initiating heme synthesis.
Neurotransmitter Synthesis
- Involved in the creation of neurotransmitters derived from amino acids.
- Key neurotransmitters include GABA (inhibitory), seratonin, and dopamine.
B6 and Fatty Acid Metabolism
- B6 supports the synthesis of gamma-linolenic acid, a precursor to anti-inflammatory prostaglandins.
Folate (Vitamin B9) Functions
- Essential for one-carbon transfer and amino acid metabolism.
- Functions as a coenzyme after undergoing reduction to THF (tetrahydrofolate) and attachment of glutamic acid residues.
Folate Absorption and Metabolism
- Absorption requires removal of polyglutamate chains, facilitated by hydrolases in the intestinal tract.
- Folate is stored in the liver and participates in enterohepatic circulation, maintaining B-vitamin levels in the body.
Implications of Folate in Health
- Crucial for nucleotide synthesis, linked to conditions like spina bifida, anemia, and potential roles in cancer.
- Exists in a methylation cycle that is disrupted when there is insufficient B12, leading to the methyl-folate trap.
Methyl-Folate Trap
- B12 deficiency prevents regeneration of THF from methyl THF, crucial for purine and pyrimidine synthesis.
- Folate supplementation may bypass this trap temporarily, aiding in treating B12-related anemia.
Deficiencies and Symptoms
- B6 deficiency can lead to neurological (lethargy, depression) and dermatological (dermatitis, brittle nails) symptoms.
- B12 deficiency may arise from hypochlorhydria, leading to similar symptoms as B9 deficiency, including megaloblastic anemia (pernicious anemia).
Clinical Testing for Deficiencies
- Blood tests for B12, homocysteine, and methylmalonic acid are essential in diagnosing deficiencies.
- Elevated levels of methylmalonic acid indicate a B12 deficiency as it is not adequately metabolized.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.