Podcast
Questions and Answers
Which of the following best describes the primary characteristic of dysphagia?
Which of the following best describes the primary characteristic of dysphagia?
- Difficulty in swallowing (correct)
- Sharp pain localized in the lower abdomen
- Involuntary muscle spasms in the limbs
- Chronic inflammation of the nasal passages
A patient reports a sensation of food sticking in their throat immediately after swallowing. This symptom is most indicative of which condition?
A patient reports a sensation of food sticking in their throat immediately after swallowing. This symptom is most indicative of which condition?
- Laryngitis
- Dysphagia (correct)
- Appendicitis
- Gastritis
Which of the following conditions is most likely to present with gradual onset dysphagia, potentially spreading to regional lymph nodes?
Which of the following conditions is most likely to present with gradual onset dysphagia, potentially spreading to regional lymph nodes?
- Soft food bolus
- Oesophageal spasm
- Oesophageal tumour (correct)
- Acid reflux
A patient with a history of acid reflux presents with dysphagia. What is the most likely underlying cause of their swallowing difficulty?
A patient with a history of acid reflux presents with dysphagia. What is the most likely underlying cause of their swallowing difficulty?
Which of the following scenarios requires the most urgent intervention?
Which of the following scenarios requires the most urgent intervention?
A patient with dysphagia is diagnosed with a fibrous stricture at the upper end of the oesophagus and presents with glossitis and iron deficiency anemia. What is the most likely underlying condition?
A patient with dysphagia is diagnosed with a fibrous stricture at the upper end of the oesophagus and presents with glossitis and iron deficiency anemia. What is the most likely underlying condition?
What is the primary mechanism behind achalasia that leads to dysphagia?
What is the primary mechanism behind achalasia that leads to dysphagia?
Which of the following conditions affecting the oral and pharyngeal regions is most likely to cause dysphagia?
Which of the following conditions affecting the oral and pharyngeal regions is most likely to cause dysphagia?
A patient presents with dysphagia secondary to herniation of the mucosa through the inferior pharyngeal constrictor muscle. This condition is most likely:
A patient presents with dysphagia secondary to herniation of the mucosa through the inferior pharyngeal constrictor muscle. This condition is most likely:
Which of the following conditions is characterized by an intermittent sensation of a lump in the throat, primarily worsened when swallowing saliva?
Which of the following conditions is characterized by an intermittent sensation of a lump in the throat, primarily worsened when swallowing saliva?
Which symptom is characterized as a retrosternal burning discomfort, primarily caused by acid reflux?
Which symptom is characterized as a retrosternal burning discomfort, primarily caused by acid reflux?
Diarrhoea and which other symptom could be indicative of fat malabsorption?
Diarrhoea and which other symptom could be indicative of fat malabsorption?
In which third of the oesophagus can the muscles either be striated or non-striated?
In which third of the oesophagus can the muscles either be striated or non-striated?
Which nerve innervates both the motor and sensory functions of the oesophageal plexus?
Which nerve innervates both the motor and sensory functions of the oesophageal plexus?
What kind of epithelium are the mucosal layers of the oesophagus?
What kind of epithelium are the mucosal layers of the oesophagus?
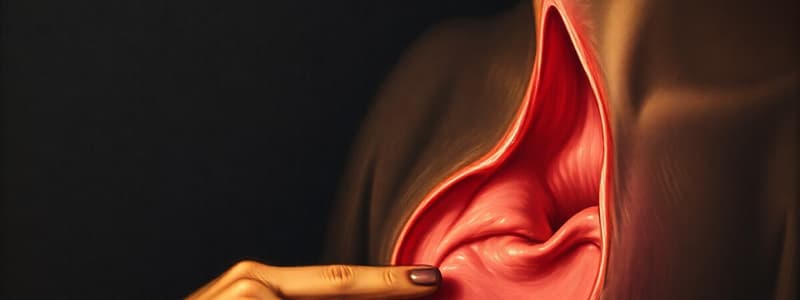
What is the primary mechanism that facilitates the movement of a food bolus through the oesophagus to the stomach?
What is the primary mechanism that facilitates the movement of a food bolus through the oesophagus to the stomach?
What best describes the pathophysiology and location of Killian's Dehiscence, often associated with pharyngeal pouch formation?
What best describes the pathophysiology and location of Killian's Dehiscence, often associated with pharyngeal pouch formation?
Which of the following best describes why Candida Oesophagitis occurs?
Which of the following best describes why Candida Oesophagitis occurs?
What is the main treatment for oesophageal spasm?
What is the main treatment for oesophageal spasm?
Which factor is crucial to address in the treatment and management of oesophageal webs due to them being premalignant?
Which factor is crucial to address in the treatment and management of oesophageal webs due to them being premalignant?
Flashcards
Dysphagia
Dysphagia
Difficulty in swallowing.
Oesophageal Dysphagia Reasons
Oesophageal Dysphagia Reasons
Tumors, inflammation, strictures, trauma; webs, spasms, achalasia.
Oesophageal Tumors (Dysphagia)
Oesophageal Tumors (Dysphagia)
SCC or adenocarcinoma causing gradual dysphagia; may spread to lymph nodes or lumen.
Inflammation Causing Dysphagia
Inflammation Causing Dysphagia
Signup and view all the flashcards
Stricture Induced-Dysphagia
Stricture Induced-Dysphagia
Signup and view all the flashcards
Foreign Body Dysphagia
Foreign Body Dysphagia
Signup and view all the flashcards
Oesophageal Web
Oesophageal Web
Signup and view all the flashcards
Oesophageal Web Components
Oesophageal Web Components
Signup and view all the flashcards
Oesophageal Spasms Causes
Oesophageal Spasms Causes
Signup and view all the flashcards
Achalasia
Achalasia
Signup and view all the flashcards
Complications of Achalasia
Complications of Achalasia
Signup and view all the flashcards
Oral/Pharyngeal Dysphagia Reasons
Oral/Pharyngeal Dysphagia Reasons
Signup and view all the flashcards
Inflammation Causing Oral Dysphagia
Inflammation Causing Oral Dysphagia
Signup and view all the flashcards
Fibrosis Causing Oral Dysphagia
Fibrosis Causing Oral Dysphagia
Signup and view all the flashcards
Pharyngeal Pouch
Pharyngeal Pouch
Signup and view all the flashcards
Pharyngeal Pouch Complications
Pharyngeal Pouch Complications
Signup and view all the flashcards
Xerostomia Causes
Xerostomia Causes
Signup and view all the flashcards
Globus Hystericus
Globus Hystericus
Signup and view all the flashcards
Heartburn
Heartburn
Signup and view all the flashcards
Achalasia Treatments
Achalasia Treatments
Signup and view all the flashcards
Study Notes
- Dysphagia: Difficulty in swallowing.
Symptoms of Dysphagia
- Sensation of something sticking in the throat or chest during or immediately after swallowing.
Oesophageal Reasons for Dysphagia
- Tumours
- SCC (majority) or adenocarcinoma (lower 1/3rd).
- Gradual onset.
- Can spread to lymph nodes or fungate into the lumen.
- Local spread effects: tracheo-oesophageal fistulation, recurrent laryngeal nerve palsy.
- Inflammation: Caused by acid reflux, drugs, or chemical burns.
- Stricture: Caused by radiation or acid reflux, leading to narrowing of the oesophagus.
- Foreign body
- Soft food bolus: Can be treated with muscle relaxants.
- Impacted coins (smooth): Requires prompt removal.
- Bones (sharp): Requires emergency removal to prevent perforation.
- Trauma: Due to bones or surgery.
- Web
- Atrophic mucosa leads to a fibrous stricture at the upper oesophagus.
- Appears as a web on barium swallow.
- Premalignant.
- Made up of glossitis, iron deficiency, anaemia, dysphagia, koilonychias.
- Seen in middle-aged women.
- Atrophic mucosa leads to a fibrous stricture at the upper oesophagus.
- External Compression from: Goitre, enlarged left atrium, mediastinal glands.
- Oesophageal Spasms: Due to atypical achalasia, acid reflux, neuromuscular disorders, or cardia obstruction.
- Achalasia
- Loss of ganglia leads to failure of cardiac sphincter relaxation.
- Obstructs oesophageal emptying with dysphagia for solids and liquids.
- Failure of peristalsis causes further dilation.
- Retained contents may regurgitate, causing respiratory issues.
- Loss of ganglia leads to failure of cardiac sphincter relaxation.
Oral and Pharyngeal Reasons for Dysphagia
- Tumours: SCC.
- Inflammation
- Severe candidiasis.
- Herpes.
- Tonsillitis, glossitis.
- Fibrosis: Scleroderma (increased collagen, decreased elastin, microstomia, and fibrosis).
- Trauma: Due to bones or surgery.
- Pouch
- Herniation of mucosa through the inferior pharyngeal constrictor muscle (cricopharyngeus).
- Pulsion diverticulum forms and collects food.
- Can regurgitate into mouth or lungs at night, causing secondary pneumonia.
- Swelling in the lower neck, usually on the left.
- Deformity of cervical spine.
- Xerostomia: Sjogren's or drugs (e.g., TCAs).
- Stroke.
- Neurological Conditions: Parkinson’s, MS, MG, Bulbar Palsy (motorneurone disease).
- Globus Hystericus
- Not true dysphagia; intermittent sensation of a lump in the throat.
- Perceived to be in the midline at the level of the cricoid cartilage.
- Worse when swallowing saliva, less obvious with food or liquids.
- Not true dysphagia; intermittent sensation of a lump in the throat.
Symptoms of GI Disease
- Abdominal pain.
- Dysphagia: Difficulty in swallowing.
- Heartburn: Retrosternal burning discomfort due to acid reflux.
- Dyspepsia: Range of upper GI symptoms (nausea, heartburn, acidity, pain); general term is ‘indigestion.’
- Flatulence: Excessive wind.
- Vomiting: Stimulation of the vomiting centres in the medulla.
- Constipation.
- Diarrhoea.
- Steatorrhoea: Pale, bulky, fatty stools.
Oesophagus Overview
- Musclotendinous tube connecting the pharynx to the stomach.
- Symptoms: Dysphagia, pain (from acid reflux), cough or vomiting (reflux), bleeding (haematemesis).
- Diseases: Pharyngeal pouch, achalasia, oesophageal spasm, oesophageal web, peptic ulcer disease/reflux, carcinoma.
Oesophagus Muscles and Structure
- Muscles
- Superior, Middle, Inferior constrictor muscles.
- Weak Point: Meeting point of thyropharyngeus and cricopharyngeus.
- Also known as: Killian’s dehiscence.
- Can become: Zenker’s Diverticulum.
- Layers: Inner circular, outer longitudinal.
- Composition: Upper 2/3 striated, lower 2/3 non-striated, middle 1/3 mixed.
- Innervation: Vagus nerve (X) for motor and sensory nerves in the oesophageal plexus.
- Lining: Stratified squamous non-keratinising epithelium.
- Swallowing: Peristaltic wave triggered, food bolus pushed to the stomach via depolarisation and action potential.
- Cardiac Sphincter: Gastro-oesophageal junction described as weak.
- Also known as: Killian’s dehiscence.
Specific Oesophageal Conditions
- Pharyngeal Pouch
- Herniation of mucosa through a weakness in the pharyngeal constrictor muscles.
- The pouch hangs down due to gravity.
- Symptoms: Dysphagia, vomiting, respiratory symptoms.
- The pouch hangs down due to gravity.
- Also known as: Zeneker’s Diverticulum forms, as it passes through Killian’s Dehiscence.
- Herniation of mucosa through a weakness in the pharyngeal constrictor muscles.
- Oesophagitis
- Inflammation due to acidic reflux from the stomach.
- Candida Oesophagitis: Occurs in immunocompromised individuals (transplant, chemo, HIV infection).
- Achalasia of the Cardia
- Loss of ganglia leads to the relaxation of the gastro-oesophageal sphincter.
- Neuromuscular dysfunction where the cardiac sphincter fails to relax during swallowing.
- Results in Functional obstruction of oesophageal emptying with dysphagia for solids and liquids.
- Failure of peristalsis can lead to progressive dilatation.
- Treatments: Drugs (nifedipine), balloon dilatation, cardiomyotomy.
- Oesophageal Spasm
- Attack of dysphagia and pain due to various causes.
- Causes: Atypical achalasia, gastro-oesophageal reflux, motor disorders, symptomatic peristalsis, obstruction at the cardia, neuromuscular disorders.
- May result in "corkscrew oesophagus," causing pain from reflux and heartburn.
- Treated with Muscle relaxants.
- Causes: Atypical achalasia, gastro-oesophageal reflux, motor disorders, symptomatic peristalsis, obstruction at the cardia, neuromuscular disorders.
- Attack of dysphagia and pain due to various causes.
- Oesophageal Web
- Consists of glossitis, iron deficiency anaemia, dysphagia, koilonychia.
- Most common in middle-aged women.
- Important to identify due to premalignant potential.
- With a barium swallow: Atrophic mucosa, fibrous structure forms at upper end, the stricture forms creating a web.
- Treatment
- Dilatation of the stricture .
- Correction of the iron deficiency.
- Occasionally webs excised.
- Consists of glossitis, iron deficiency anaemia, dysphagia, koilonychia.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.