Podcast
Questions and Answers
What is the primary action of Disease Modifying Anti-Rheumatic Drugs (DMARDs) in the treatment of rheumatoid arthritis?
What is the primary action of Disease Modifying Anti-Rheumatic Drugs (DMARDs) in the treatment of rheumatoid arthritis?
- Provide immediate pain relief
- Relieve muscle spasms
- Promote bone density
- Slow joint degeneration (correct)
Which of the following is a common adverse reaction to DMARDs?
Which of the following is a common adverse reaction to DMARDs?
- Alopecia (correct)
- Constipation
- Headaches
- Increased appetite
Which adverse reaction is specifically associated with the use of Plaquenil?
Which adverse reaction is specifically associated with the use of Plaquenil?
- Visual acuity improvement
- Hearing loss
- Retinal damage (correct)
- Increased risk of infection
Methotrexate is contraindicated for which of the following patients?
Methotrexate is contraindicated for which of the following patients?
What should women taking DMARDs be cautious about?
What should women taking DMARDs be cautious about?
What is the interaction risk when combining sulfa drugs with methotrexate?
What is the interaction risk when combining sulfa drugs with methotrexate?
What is the role of Bone Resorption Inhibitors (Bisphosphonates)?
What is the role of Bone Resorption Inhibitors (Bisphosphonates)?
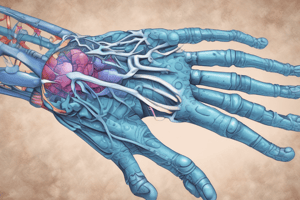
Which deformity is specifically associated with late-stage rheumatoid arthritis?
Which deformity is specifically associated with late-stage rheumatoid arthritis?
What is a contraindication for the use of bisphosphonates?
What is a contraindication for the use of bisphosphonates?
Which of the following is a common side effect associated with all uric acid inhibitors?
Which of the following is a common side effect associated with all uric acid inhibitors?
What should be monitored regularly in patients taking bisphosphonates?
What should be monitored regularly in patients taking bisphosphonates?
What interaction reduces the effectiveness of bisphosphonates?
What interaction reduces the effectiveness of bisphosphonates?
Which skeletal muscle relaxant is known to increase the risk of hepatic toxicity?
Which skeletal muscle relaxant is known to increase the risk of hepatic toxicity?
In patients taking colchicine for an acute gout attack, what is a significant adverse effect to monitor for?
In patients taking colchicine for an acute gout attack, what is a significant adverse effect to monitor for?
What is the recommended action if a rash develops in a patient taking allopurinol?
What is the recommended action if a rash develops in a patient taking allopurinol?
Which of the following should be taken with caution to avoid increasing side effects when using colchicine?
Which of the following should be taken with caution to avoid increasing side effects when using colchicine?
What is the appropriate nursing intervention following administration of a bisphosphonate?
What is the appropriate nursing intervention following administration of a bisphosphonate?
What is the maximum recommended duration for the use of skeletal muscle relaxants?
What is the maximum recommended duration for the use of skeletal muscle relaxants?
Which drug interaction increases the risk of gastrointestinal bleeding when using allopurinol?
Which drug interaction increases the risk of gastrointestinal bleeding when using allopurinol?
What is an advisable nursing intervention when administering uric acid inhibitors?
What is an advisable nursing intervention when administering uric acid inhibitors?
Which effect is associated with long-term use of skeletal muscle relaxants?
Which effect is associated with long-term use of skeletal muscle relaxants?
What is a potential adverse reaction for patients taking Diclofenac?
What is a potential adverse reaction for patients taking Diclofenac?
What is the goal of pharmacological treatment of osteoporosis?
What is the goal of pharmacological treatment of osteoporosis?
How do bone inhibitors work?
How do bone inhibitors work?
How can reflux associated with bone resorption inhibitors be minimized?
How can reflux associated with bone resorption inhibitors be minimized?
How does vitamin D enhance bone health?
How does vitamin D enhance bone health?
Which bone inhibitor is contraindicated during pregnancy?
Which bone inhibitor is contraindicated during pregnancy?
If a patient develops stomatitis related to DMARDs, what instructions should be given to the patient to minimize the effects of stomatitis?
If a patient develops stomatitis related to DMARDs, what instructions should be given to the patient to minimize the effects of stomatitis?
Why should women taking DMARDs be instructed to use an effective form of birth control?
Why should women taking DMARDs be instructed to use an effective form of birth control?
Which DMARD is also a drug used to treat various types of cancer?
Which DMARD is also a drug used to treat various types of cancer?
What nursing interventions are appropriate for a patient who has developed signs and symptoms of bone marrow depression related to DMARD therapy? (Select all that apply)
What nursing interventions are appropriate for a patient who has developed signs and symptoms of bone marrow depression related to DMARD therapy? (Select all that apply)
How is the action of DMARDs appropriate in treating patients with rheumatoid arthritis?
How is the action of DMARDs appropriate in treating patients with rheumatoid arthritis?
What is defined as pancytopenia?
What is defined as pancytopenia?
What is the definition of alopecia?
What is the definition of alopecia?
Which of the following best defines exfoliative dermatitis?
Which of the following best defines exfoliative dermatitis?
What is the drug of choice for maintenance of gouty arthritis?
What is the drug of choice for maintenance of gouty arthritis?
What should be included in a teaching plan for a patient with gout?
What should be included in a teaching plan for a patient with gout?
What is the most common adverse effect of muscle relaxants?
What is the most common adverse effect of muscle relaxants?
Before giving a PRN muscle relaxant, what must the nurse first assess?
Before giving a PRN muscle relaxant, what must the nurse first assess?
Why are muscle relaxants useful in treating the pain associated with acute muscle injuries?
Why are muscle relaxants useful in treating the pain associated with acute muscle injuries?
How would the nurse evaluate the effectiveness of DMARDs and muscle relaxants?
How would the nurse evaluate the effectiveness of DMARDs and muscle relaxants?
Flashcards
What are Disease Modifying Anti-Rheumatic Drugs (DMARDs)?
What are Disease Modifying Anti-Rheumatic Drugs (DMARDs)?
Drugs that work by suppressing the immune system, often used to treat rheumatoid arthritis, fibromyalgia, and inflammatory bowel diseases.
What is Stomatitis?
What is Stomatitis?
A common adverse reaction of DMARDs, characterized by inflammation and sores in the mouth.
What is Retinal Damage?
What is Retinal Damage?
A side effect of DMARDs that can cause vision problems, particularly affecting the retina.
What is Methotrexate?
What is Methotrexate?
Signup and view all the flashcards
What is Heart Failure (HF)?
What is Heart Failure (HF)?
Signup and view all the flashcards
What is Boutonierre Deformity?
What is Boutonierre Deformity?
Signup and view all the flashcards
What is Ulnar Deviation?
What is Ulnar Deviation?
Signup and view all the flashcards
What are Bone Resorption Inhibitors?
What are Bone Resorption Inhibitors?
Signup and view all the flashcards
Bisphosphonates
Bisphosphonates
Signup and view all the flashcards
Increased or Recurrent Bone Pain
Increased or Recurrent Bone Pain
Signup and view all the flashcards
Esophagitis
Esophagitis
Signup and view all the flashcards
Bisphosphonates in Pregnancy
Bisphosphonates in Pregnancy
Signup and view all the flashcards
Uric Acid Inhibitors
Uric Acid Inhibitors
Signup and view all the flashcards
Nausea, Vomiting, Diarrhea (N/V/D)
Nausea, Vomiting, Diarrhea (N/V/D)
Signup and view all the flashcards
Skin Rash, Hepatitis, Kidney Damage (Allopurinol)
Skin Rash, Hepatitis, Kidney Damage (Allopurinol)
Signup and view all the flashcards
Uric Acid Inhibitors in Pregnancy
Uric Acid Inhibitors in Pregnancy
Signup and view all the flashcards
Skeletal Muscle Relaxants
Skeletal Muscle Relaxants
Signup and view all the flashcards
Drowsiness, Dizziness
Drowsiness, Dizziness
Signup and view all the flashcards
Physical Dependence
Physical Dependence
Signup and view all the flashcards
Skeletal Muscle Relaxants in Pregnancy
Skeletal Muscle Relaxants in Pregnancy
Signup and view all the flashcards
Short-Term Use of Skeletal Muscle Relaxants
Short-Term Use of Skeletal Muscle Relaxants
Signup and view all the flashcards
Skeletal Muscle Relaxants and Alcohol
Skeletal Muscle Relaxants and Alcohol
Signup and view all the flashcards
Study Notes
Disease-Modifying Anti-Rheumatic Drugs (DMARDs)
- Slow joint degeneration and progression of rheumatoid arthritis (RA).
- Used when pain relief and anti-inflammatory drugs are ineffective.
- Act by producing immunosuppression; also treat fibromyalgia and inflammatory bowel diseases (Crohn's disease).
- Common adverse reactions: Nausea, stomatitis, alopecia.
- Other potential adverse reactions: Skin rash, fever, easy bruising, visual changes, tinnitus, hearing loss.
- Sulfasalazine-containing DMARDs: Ocular changes, gastrointestinal upset, mild pancytopenia.
- Plaquenil: Can cause retinal damage.
- Contraindications (Methotrexate): Renal insufficiency, liver disease, alcohol abuse, folate deficiency, pancytopenia.
- Contraindications (Enbrel, Humira, Remicade): Heart failure (HF) or neurological demyelinating diseases.
- Late-stage RA deformities: Boutonniere deformity of the thumb, ulnar deviation of metacarpophalangeal joints, swan-neck deformity of fingers.
- Precautions: Pregnancy and drug transmission to semen (barrier methods).
- Methotrexate precautions: Monitor thrombocytopenia, leukopenia, liver, and kidney functions every 3 months.
- Reporting issues: Report mouth sores, diarrhea, fever, sore throat, easy bruising, rash, itching, or nausea/vomiting.
- Drug interactions (DMARDs):
- Sulfa drugs increase methotrexate toxicity.
- Aspirin and NSAIDs increase methotrexate toxicity.
- Nursing Interventions: Monitor labs (thrombocytopenia, leukopenia, liver enzymes, kidney function). Monitor for drug toxicity. Teach patient compliance, birth control, reporting of infections/bleeding/allergies.
Bone Resorption Inhibitors (Bisphosphonates)
-
Inhibit bone resorption, increasing bone density and reversing osteoporosis.
-
Used for osteoporosis in postmenopausal women and in hypercalcemia of malignancy.
-
No completely safe drug: No drug is risk-free.
-
Adverse reactions:
- Increased/recurrent bone pain.
- Esophagitis, esophageal ulceration, dyspepsia, acid regurgitation, dysphagia.
- Abdominal pain, nausea, diarrhea, constipation.
- Musculoskeletal pain.
- Visual disturbances.
- Increased risk of bleeding (especially with other clotting inhibitors).
- Nephrotoxicity (IV infusions).
-
Contraindications: Pregnancy, lactation, hypocalcemia, dysphagia, esophageal stricture, serious kidney impairment. Fosamax and Actonel in patients with hypocalcemia.
-
Drug interactions:
- Antacids decrease bisphosphonate effectiveness.
- Aspirin increases risk of GI bleeds.
- Theophylline increases Theophylline toxicity.
- Caffeine, orange juice, magnesium supplements, iron, and calcium decrease alendronate absorption (wait 2 hours).
-
Nursing Interventions: Administer with 8 oz water, upright position, stay upright 30 minutes after. Take first thing in the morning on an empty stomach. Supplement calcium and vitamin D if needed. Regular bone scans (12-18 months). Monitor blood calcium. Exercise (30-40 minutes daily).
Uric Acid Inhibitors
-
Used for acute gout attacks (colchicine); preventing attacks (allopurinol, probenecid, febuxostat).
-
Adverse reactions: Nausea, vomiting, diarrhea (all drugs).
-
Allopurinol: Skin rash, hepatitis, kidney damage.
-
Colchicine: Severe nausea, vomiting, bone marrow depression, thrombocytopenia, rhabdomyolysis.
-
Probenecid: Kidney stones, kidney problems.
-
Contraindications: Pregnancy, lactation.
-
Anturane (sulfinpyrazone): Peptic ulcer disease.
-
Colchicine: Serious GI, renal, hepatic, or cardiac disorders.
-
Probenecid: Blood dyscrasias, uric acid kidney stones, children under 2 years.
-
Drug interactions:
- Grapefruit juice increases colchicine side effects.
- Ampicillin may cause rash with allopurinol.
- Theophylline increases allopurinol toxicity.
- Coumadin increases allopurinol bleeding risk.
- Penicillin increases antibiotic levels with probenecid.
- NSAIDs increase NSAID levels with probenecid.
- Barbiturates increase sedation with probenecid.
- Salicylates decrease probenecid effectiveness.
Oral anticoagulants increase bleeding risk with Anturane. Tobutamide increases hypoglycemia risk with Anturane.
- Nursing Interventions: Take with meals/plenty of water (3000 cc/day). Maintain adequate urine. Monitor stool and urine for blood. Keep colchicine on hand. Monitor uric acid levels, CBC, UA, liver, and kidney function. Stop drug and notify provider if rash develops. Avoid alcohol and high-purine foods. Regular exercise.
Skeletal Muscle Relaxants
-
Uses: For acute musculoskeletal pain.
-
Adverse Reactions (all): Drowsiness, dizziness, UTI (Zanaflex). Some drugs include hepatic toxicity; chronic use may lead to physical dependence.
-
Baclofen: Nausea, constipation, urinary retention, seizures.
-
Dantrolene: Hepatic toxicity, muscle weakness.
-
Contraindications: Pregnancy, lactation.
-
Flexeril & MAOIs: Avoid within 14 days of MAOI use.
-
Flexeril: Recent MI, cardiac conduction problems, or hyperthyroidism.
-
Diazepam: Controlled substance (IV use).
-
Drug Interactions: CNS depressants increase CNS depressant effects. Flexeril and MAOIs increase risk of seizures/fever. Norflex and Haldol increase psychosis risk. Zanaflex and antihypertensives increase hypotension risk.
-
Nursing Interventions: Take with or after meals to minimize GI problems. Short-term use only (2-3 weeks). Avoid alcohol/CNS depressants.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.