Podcast
Questions and Answers
What role does the parasympathetic activity play in the digestive system?
What role does the parasympathetic activity play in the digestive system?
- Increases heart rate during digestion
- Enhances blood flow to the skin
- Promotes digestion (correct)
- Inhibits digestion
Which of the following hormones is NOT directly involved in regulating digestive secretions?
Which of the following hormones is NOT directly involved in regulating digestive secretions?
- CCK
- Secretin
- Gastrin
- Insulin (correct)
During which phase of swallowing does the process become involuntary?
During which phase of swallowing does the process become involuntary?
- Pre-swallowing Phase
- Oral Phase
- Esophageal Phase
- Pharyngeal Phase (correct)
What is the primary function of peristalsis in the esophagus?
What is the primary function of peristalsis in the esophagus?
Which mechanism blocks the nasal passage during swallowing?
Which mechanism blocks the nasal passage during swallowing?
The lower esophageal sphincter (LES) has the role of:
The lower esophageal sphincter (LES) has the role of:
Which cranial nerve is NOT involved in the swallowing reflex?
Which cranial nerve is NOT involved in the swallowing reflex?
Segmentation in the digestive process primarily serves to:
Segmentation in the digestive process primarily serves to:
What is the primary purpose of the gastric phase of digestion?
What is the primary purpose of the gastric phase of digestion?
Which hormones are released during the intestinal phase to regulate digestion?
Which hormones are released during the intestinal phase to regulate digestion?
What role does bicarbonate play during the intestinal phase?
What role does bicarbonate play during the intestinal phase?
Which segment of the small intestine is primarily responsible for nutrient absorption?
Which segment of the small intestine is primarily responsible for nutrient absorption?
What is the significance of villi and microvilli in the small intestine?
What is the significance of villi and microvilli in the small intestine?
How does the intestinal phase affect gastric emptying?
How does the intestinal phase affect gastric emptying?
Which segment of the small intestine connects to the cecum?
Which segment of the small intestine connects to the cecum?
What triggers the gastric phase of digestion?
What triggers the gastric phase of digestion?
What is a common cause of intestinal obstruction?
What is a common cause of intestinal obstruction?
What is the role of secretin in the small intestine?
What is the role of secretin in the small intestine?
Which enzyme is responsible for breaking down lactose?
Which enzyme is responsible for breaking down lactose?
What condition may result from mesenteric ischemia?
What condition may result from mesenteric ischemia?
How do villi and microvilli contribute to the function of the small intestine?
How do villi and microvilli contribute to the function of the small intestine?
What is the primary function of the mucus secreted in the small intestine?
What is the primary function of the mucus secreted in the small intestine?
What is the primary role of gastrin in stomach functioning?
What is the primary role of gastrin in stomach functioning?
Which hormone is released in response to acidic chyme entering the small intestine?
Which hormone is released in response to acidic chyme entering the small intestine?
Which of the following is the most common malignancy of the small intestine?
Which of the following is the most common malignancy of the small intestine?
Which hormone stimulates the release of pancreatic enzymes and bile for fat digestion?
Which hormone stimulates the release of pancreatic enzymes and bile for fat digestion?
How does cholecystokinin (CCK) affect stomach emptying?
How does cholecystokinin (CCK) affect stomach emptying?
What structure in the stomach allows it to expand as it fills with food?
What structure in the stomach allows it to expand as it fills with food?
What is the role of secretin in the digestive process?
What is the role of secretin in the digestive process?
Which nerve is responsible for increasing stomach motility and secretion?
Which nerve is responsible for increasing stomach motility and secretion?
Which of the following hormones is NOT produced by cells in the gastrointestinal tract?
Which of the following hormones is NOT produced by cells in the gastrointestinal tract?
What is the effect of sympathetic innervation on stomach activity?
What is the effect of sympathetic innervation on stomach activity?
What role does bicarbonate play in the gastrointestinal tract?
What role does bicarbonate play in the gastrointestinal tract?
Where do gastric ulcers primarily occur?
Where do gastric ulcers primarily occur?
Which of the following is NOT a component of the mucosal defense mechanisms?
Which of the following is NOT a component of the mucosal defense mechanisms?
What can excessive production of gastric acid lead to?
What can excessive production of gastric acid lead to?
Which factor can increase acid production in the stomach?
Which factor can increase acid production in the stomach?
What is the primary cause of damage in the gastric mucosa leading to ulcers?
What is the primary cause of damage in the gastric mucosa leading to ulcers?
What substance is essential for the absorption of vitamin B12?
What substance is essential for the absorption of vitamin B12?
Which layer of the gastrointestinal tract provides structural support?
Which layer of the gastrointestinal tract provides structural support?
Flashcards are hidden until you start studying
Study Notes
Gastric Phase
- Gastric phase is triggered when food enters the stomach, stretching the stomach wall and stimulating the presence of proteins. This leads to the release of gastrin, which boosts the production of hydrochloric acid (HCl) and pepsinogen.
- Pepsinogen, when activated by HCl, becomes pepsin, a crucial enzyme for protein digestion.
- The stomach's motility increases, mixing food with gastric juices to form chyme, a semi-liquid mixture ready for further digestion in the small intestine.
- This phase is considered the main digestive phase, as gastric secretions and muscle contractions work together to liquefy food.
Intestinal Phase
- The intestinal phase begins when chyme enters the duodenum, the first part of the small intestine.
- This triggers the release of secretin and cholecystokinin (CCK) from the small intestine.
- Secretin and CCK play a vital role in regulating the flow of chyme into the duodenum, preventing it from being overloaded.
- Secretin also stimulates the pancreas to release bicarbonate which neutralizes stomach acid, and CCK stimulates the gallbladder to release bile for fat digestion.
- The intestinal phase ultimately ensures proper digestion and absorption of nutrients in the small intestine, while preventing excessive acidity.
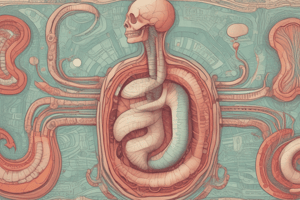
Small Intestine Anatomy
- The small intestine consists of three segments:
- Duodenum: The shortest segment, it receives chyme from the stomach, bile from the liver and gallbladder, and pancreatic juices.
- Jejunum: The middle section, responsible for the majority of nutrient absorption.
- Ileum: The longest section, absorbs vitamin B12 and bile salts, connecting to the large intestine.
- The small intestine mucosa features villi and microvilli, finger-like projections that greatly increase surface area for nutrient absorption.
Essential Physiology
- The autonomic nervous system governs digestive functions. Parasympathetic activity promotes digestion, while sympathetic activity inhibits it, particularly during stressful situations.
- Gastrin, CCK, and secretin are essential hormones that carefully regulate digestive secretions and motility.
- Peristalsis is responsible for moving food along the digestive tract, while segmentation mixes food to ensure better digestion.
- The combined action of digestive enzymes and bile is crucial for breaking down nutrients into absorbable forms.
Physiology of Swallowing
- Swallowing involves the transportation of food or liquid from the mouth to the stomach. This complex process involves voluntary and involuntary phases.
- Oral Phase (Voluntary): We consciously initiate swallowing by chewing food (mastication), mixing it with saliva to form a bolus. The tongue then pushes the bolus towards the back of the mouth (oropharynx), triggering the next phase.
- Pharyngeal Phase (Involuntary): The process now becomes involuntary as the bolus reaches the pharynx. The rising soft palate closes the nasal passage, preventing food from entering the nasal cavity. The epiglottis covers the trachea to prevent food from entering the airways. Pharyngeal muscles contract, propelling the bolus into the esophagus. This phase is regulated by the swallowing reflex.
- Esophageal Phase (Involuntary): The bolus travels down the esophagus through peristalsis, rhythmic contractions of smooth muscle. The lower esophageal sphincter (LES) relaxes, allowing the bolus to enter the stomach, and immediately closes to prevent reflux.
- Swallowing Reflex: Coordinated by the swallowing center in the medulla oblongata and pons. This reflex involves sensory and motor nerves, primarily cranial nerves V, VII, IX, X, and XII.
Stomach: Innervation and Mucosal Structure
- Innervation:
- Parasympathetic: Via the vagus nerve, stimulates stomach motility and secretion.
- Sympathetic: Via the celiac plexus, inhibits stomach activity during stress or danger (fight-or-flight response).
- Mucosal Structure:
- Rugae: Folds in the stomach lining that allow it to expand as it fills with food.
- Gastric Pits: Microscopic indentations in the mucosa leading to gastric glands, which secrete digestive substances (HCl, pepsinogen, mucus).
Hormones Affecting Stomach Emptying
- Gastrin: Produced by G cells in the stomach and duodenum:
- Stimulates gastric motility, increasing stomach muscle contractions and promoting faster emptying.
- Enhances HCl secretion, contributing to food breakdown for emptying into the small intestine.
- Released in response to food, especially protein-rich meals.
- Secretin: Produced by S cells in the duodenum:
- Slows down gastric emptying when acidic chyme reaches the small intestine.
- Stimulates bicarbonate secretion from the pancreas, neutralizing stomach acid in the duodenum.
- Inhibits gastric motility, preventing excessive acid from entering the small intestine at once.
- Released in response to low pH (acidity) in the duodenum.
- Cholecystokinin (CCK): Produced by I cells in the duodenum and jejunum:
- Inhibits gastric emptying, allowing time for the digestion of fats and proteins.
- Stimulates the release of bile from the gallbladder and pancreatic enzymes, crucial for fat digestion.
- Released when fatty or protein-rich chyme enters the small intestine.
- Slows down stomach emptying for efficient digestion and absorption of fats.
Small Intestine: Obstructions and Pathophysiology
- Intestinal Obstruction: Caused by factors such as adhesions, hernias, tumors, or strictures, leading to abdominal pain, distension, and vomiting.
- Mesenteric Ischemia: Reduced blood flow to the small intestine, causing tissue damage, severe abdominal pain, and potentially necrosis.
- Adenocarcinoma: The most common malignancy of the small intestine, manifesting with weight loss, obstruction, or bleeding.
Secretions of the Small Intestine
- Mucus: Secreted by goblet cells in the intestinal epithelium and Brunner's glands (duodenum):
- Protects the intestinal lining.
- Lubricates the movement of chyme.
- Assists in moving material through the intestines.
- Digestive Enzymes (Brush Border Enzymes): Located on microvilli, they complete the final digestion of carbohydrates and proteins:
- Lactase: Breaks down lactose into glucose and galactose.
- Sucrase: Breaks down sucrose into glucose and fructose.
- Maltase: Breaks down maltose into two glucose molecules.
- Peptidases: Break down peptides into amino acids.
- Hormones:
- Secretin: Stimulates bicarbonate secretion from the pancreas to neutralize gastric acid.
- Cholecystokinin (CCK): Stimulates the release of bile from the gallbladder and pancreatic enzymes, aiding in fat digestion.
- Bicarbonate: Secreted by Brunner's glands in the duodenum:
- Neutralizes stomach acid, creating a suitable environment for intestinal enzymes.
Anatomy Related to Peptic Ulcer Disease
- Location of Peptic Ulcers:
- Gastric ulcers: Occur in the stomach lining.
- Duodenal ulcers: Found in the first part of the small intestine (duodenum).
- Esophageal ulcers: Can occur in the esophagus, usually due to gastroesophageal reflux disease (GERD).
- Mucosal Layers:
- Mucosa: Innermost layer of the gastrointestinal tract, crucial for ulcer formation.
- Submucosa: Contains blood vessels and nerves, providing structural support.
- Muscularis: Composed of smooth muscle layers that facilitate peristalsis.
- Protective Factors:
- Mucus Layer: Protects epithelial cells from acidic gastric secretions.
- Bicarbonate Secretion: Neutralizes stomach acid, maintaining pH balance.
- Blood Flow: Adequate blood supply to the mucosa supports healing and protection.
Physiology of Peptic Ulcer Disease
- Gastric Secretions:
- Hydrochloric Acid (HCl): Secreted by parietal cells, essential for digestion but can damage the stomach lining if unregulated.
- Pepsinogen: Activated by HCl into pepsin, digesting proteins but also contributing to ulcer formation.
- Intrinsic Factor: Aids in vitamin B12 absorption, not directly related to ulcers.
- Mucosal Defense Mechanisms:
- Mucosal Barrier: Composed of mucus, bicarbonate, and epithelial cells that rapidly regenerate to protect against acid.
- Epithelial Renewal: Rapid turnover of epithelial cells assists in healing.
Factors Affecting Secretion and Defense
- Diet: Certain foods can increase acid production or irritate the stomach lining.
- Stress: Can elevate acid secretion and decrease mucosal blood flow.
Pathophysiology of Peptic Ulcer Disease
- Causes:
- Helicobacter pylori (H. pylori): A bacterial infection that damages the gastric mucosa, disrupting the protective barrier.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Inhibit prostaglandin production, leading to decreased mucus and bicarbonate secretion and increased acid secretion.
- Excessive Gastric Acid Production: Can result from increased secretion, stress, or other factors.
- Mechanism of Ulcer Formation: H. pylori or other factors damage the mucosa, leading to a breakdown of the protective barrier and allowing acidic gastric juice to erode the tissue, forming ulcers.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.