Podcast
Questions and Answers
What is the term for the contractions that start when the bolus reaches the upper part of the esophagus?
What is the term for the contractions that start when the bolus reaches the upper part of the esophagus?
- Lower esophageal sphincter contractions
- Primary peristaltic contractions (correct)
- Secondary peristaltic contractions
- Deglutition reflex contractions
What is the primary function of the first stage of deglutition?
What is the primary function of the first stage of deglutition?
- Passage of food material from the pharynx into the oesophagus
- Passage of material through the oral cavity into the pharynx (correct)
- Contraction of the superior pharyngeal constrictor
- Mastication and respiration
What happens to the pressure in the upper part of the esophagus initially when a bolus enters?
What happens to the pressure in the upper part of the esophagus initially when a bolus enters?
- The pressure remains constant
- The pressure becomes positive
- The pressure becomes negative (correct)
- The pressure increases suddenly
Which muscles are involved in the upward and backward movements of the tongue during the first stage of deglutition?
Which muscles are involved in the upward and backward movements of the tongue during the first stage of deglutition?
What is the role of the lower esophageal sphincter?
What is the role of the lower esophageal sphincter?
What occurs during the second stage of deglutition?
What occurs during the second stage of deglutition?
What induces secondary peristaltic contractions?
What induces secondary peristaltic contractions?
What is the maximum pressure developed during primary peristaltic contractions?
What is the maximum pressure developed during primary peristaltic contractions?
Which nerves carry parasympathetic action potentials to the stomach?
Which nerves carry parasympathetic action potentials to the stomach?
What is the effect of cocainisation on the swallowing reflex?
What is the effect of cocainisation on the swallowing reflex?
What is the primary function of postganglionic neurons in the stomach?
What is the primary function of postganglionic neurons in the stomach?
What is the stimulus for the deglutition reflex?
What is the stimulus for the deglutition reflex?
What occurs during the elevation of the soft palate during the second stage of deglutition?
What occurs during the elevation of the soft palate during the second stage of deglutition?
What is the primary function of the primary peristaltic wave during the second stage of deglutition?
What is the primary function of the primary peristaltic wave during the second stage of deglutition?
What is the role of gastrin in the stomach?
What is the role of gastrin in the stomach?
What is the sequence of events in the lower esophageal sphincter during swallowing?
What is the sequence of events in the lower esophageal sphincter during swallowing?
What type of act is the beginning of swallowing?
What type of act is the beginning of swallowing?
What is the role of the cricopharyngeus muscle during the second stage of deglutition?
What is the role of the cricopharyngeus muscle during the second stage of deglutition?
What is the primary mechanism by which chyme in the duodenum with a pH less than 2 inhibits gastric secretions?
What is the primary mechanism by which chyme in the duodenum with a pH less than 2 inhibits gastric secretions?
What is the primary function of the peristaltic wave in the stomach?
What is the primary function of the peristaltic wave in the stomach?
What happens to the pharynx after the bolus enters the oesophagus?
What happens to the pharynx after the bolus enters the oesophagus?
What is the role of pacemaker cells in the stomach?
What is the role of pacemaker cells in the stomach?
What is the final phase of the peristaltic contraction of the antrum?
What is the final phase of the peristaltic contraction of the antrum?
What happens when the peristaltic wave moves over the proximal antrum?
What happens when the peristaltic wave moves over the proximal antrum?
What happens to the pylorus when the peristaltic wave moves over the middle of the antrum?
What happens to the pylorus when the peristaltic wave moves over the middle of the antrum?
How does the gastric chyme get swept into the duodenum during the emptying phase?
How does the gastric chyme get swept into the duodenum during the emptying phase?
What happens to the viscous and solid mass of the chyme during the emptying phase?
What happens to the viscous and solid mass of the chyme during the emptying phase?
What happens to the parts of the chyme that flow across the central opening of the peristaltic wave?
What happens to the parts of the chyme that flow across the central opening of the peristaltic wave?
What happens during the contraction of the terminal antrum?
What happens during the contraction of the terminal antrum?
What is the result of the jet-like retropulsion during the contraction of the terminal antrum?
What is the result of the jet-like retropulsion during the contraction of the terminal antrum?
What is the primary function of the peristaltic wave in the antrum?
What is the primary function of the peristaltic wave in the antrum?
What happens to the chyme in the proximal antrum during the phase of emptying and mixing?
What happens to the chyme in the proximal antrum during the phase of emptying and mixing?
Which type of muscle forms the External Sphincter around the anal canal?
Which type of muscle forms the External Sphincter around the anal canal?
What is the primary function of the rectum during defecation?
What is the primary function of the rectum during defecation?
What is the typical intrarectal pressure that triggers the desire for defecation?
What is the typical intrarectal pressure that triggers the desire for defecation?
What is the role of the stretch receptors in the rectal wall during defecation?
What is the role of the stretch receptors in the rectal wall during defecation?
Which nerve branch innervates the External Sphincter?
Which nerve branch innervates the External Sphincter?
What is the result of increasing intra-abdominal pressure during defecation?
What is the result of increasing intra-abdominal pressure during defecation?
What is the role of the myenteric plexus in defecation?
What is the role of the myenteric plexus in defecation?
What is the effect of prolonged distension of the rectum on the internal anal sphincter?
What is the effect of prolonged distension of the rectum on the internal anal sphincter?
Flashcards are hidden until you start studying
Study Notes
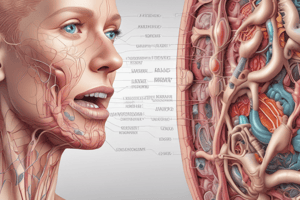
First Stage or Oral Stage
- The first stage of deglutition involves the passage of material through the oral cavity into the pharynx, which is under voluntary control.
- The contraction of the mylohyoid, styloglossus, and hypoglossus muscles causes upward and backward movements of the tongue, throwing the bolus of food back through the pillars of the fauces into the pharynx.
- During this phase, mastication ceases, and respiration is inhibited reflexly.
Second Stage or Pharyngeal Stage
- The second stage involves the passage of the bolus from the pharynx into the esophagus, which is a reflex process known as the swallowing reflex.
- Key events in this stage include:
- The contact of food material with pharyngeal and peripharyngeal structures initiates and completes the second and third stages of deglutition.
- The soft palate is elevated, and the nasopharynx is closed off from the rest of the pharynx.
- The larynx and hyoid bone are elevated, and the vocal cords are adducted, causing a momentary stoppage of respiration and speech.
- The contraction of the superior pharyngeal constrictor induces a rapid pharyngeal peristaltic wave, which propels the bolus into the esophagus.
Peristalsis and Swallowing
- Primary peristaltic contractions occur when the bolus reaches the upper part of the esophagus, propelling the bolus towards the stomach.
- Pressure developed during primary peristaltic contractions is important for propelling the bolus.
- Initially, the pressure becomes negative in the upper part of the esophagus due to the stretching of the closed esophagus by the elevation of the larynx.
- Secondary peristaltic contractions occur if the primary peristaltic contractions are unable to propel the bolus into the stomach, pushing the bolus into the stomach.
Role of Lower Esophageal Sphincter
- The distal 2-5 cm of the esophagus acts as a sphincter, known as the lower esophageal sphincter, which is constricted always.
- When the bolus enters this part of the esophagus, the sphincter relaxes, allowing the contents to enter the stomach.
- After the entry of the bolus into the stomach, the sphincter constricts, closing the lower end of the esophagus.
Deglutition Reflex
- Though the beginning of swallowing is a voluntary act, it becomes involuntary and is carried out by a reflex action called the deglutition reflex.
- The deglutition reflex occurs during the pharyngeal and esophageal stages.
- Stimulus: When the bolus enters the oropharyngeal region, the receptors present in this region are stimulated, carrying parasympathetic action potentials to the stomach.
Gastric Phase
- The gastric pump is characterized by peristaltic waves, which are induced by pacemaker cells in the stomach body.
- The peristaltic waves are propagated from the body to the antrum, eventually closing the pyloric sphincter.
- The peristaltic contraction of the antrum can be divided into three phases: propulsion, emptying and mixing, and retropulsion and grinding.
- The antral pump is associated with a sieving effect, where liquids with small suspended particles are swept across the pylorus into the duodenum, while viscous and solid materials are retained in the stomach.
Intestinal Phase
- Chyme in the duodenum with a pH less than 2 or containing lipids inhibits gastric secretions by three mechanisms:
- Sensory input to the medulla from the duodenum inhibits the motor input from the medulla to the stomach.
- Local reflexes inhibit gastric secretion - enterogastric reflex, secretin, and cholecystokinin produced by the duodenum decrease gastric secretions in the stomach.
Defecation
- Voiding of feces is known as defecation, which involves a series of coordinated motor activities.
- The rectum has two primary functions: (1) to serve as a storage site for feces and (2) to expel feces during defecation.
- When the rectal capacity is exceeded, intramural stretch receptors are activated, making the individual aware of the urgency of the forthcoming event and relaxing the internal anal sphincter.
- The individual can inhibit defecation by voluntarily increasing the tone of the external anal sphincter, which transiently increases internal sphincter tone.
Defecation Reflexes
- Defecation reflexes are classified into two types: intrinsic and extrinsic.
- Intrinsic defecation reflex is mediated through the myenteric plexus, where the distention of the rectal wall by the arriving feces initiates peristaltic waves that spread through a local circuit in the descending and sigmoid colon and the rectum.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.