Podcast
Questions and Answers
In dentistry, what is the primary purpose of implants?
In dentistry, what is the primary purpose of implants?
- To provide temporary support for damaged teeth.
- To support fixed or removable prostheses by being placed in or on bone. (correct)
- To realign the jaw and correct bite issues.
- To replace missing teeth only for aesthetic reasons.
What factor significantly advanced the development of modern implantology?
What factor significantly advanced the development of modern implantology?
- The discovery of new ceramic materials.
- The introduction of immediate loading protocols.
- The understanding of how metals react to bodily fluids, bone physiology, and tissues. (correct)
- The use of patient-specific implant designs.
Who introduced the concept of 'Osseointegration' and when was it widely accepted in implantology?
Who introduced the concept of 'Osseointegration' and when was it widely accepted in implantology?
- Albrektson in the early 1970s
- Hobo in the 1960s.
- Ichida, gaining acceptance in the early 1990s.
- Branemark, with the concept gaining acceptance in the 1980s. (correct)
What term describes the integration of the implant with surrounding soft tissues, in addition to bone?
What term describes the integration of the implant with surrounding soft tissues, in addition to bone?
Which material property is most associated with successful osseointegration?
Which material property is most associated with successful osseointegration?
What is a critical consideration regarding loading implants during the healing period?
What is a critical consideration regarding loading implants during the healing period?
What does immediate loading/ immediate restoration of dental implants rely heavily on?
What does immediate loading/ immediate restoration of dental implants rely heavily on?
According to the Harvard conference in 1975, what is the maximum acceptable mobility for a successful implant?
According to the Harvard conference in 1975, what is the maximum acceptable mobility for a successful implant?
According to the 1986 Albrektson and Zarb criteria, what radiographic finding should be absent for implant success?
According to the 1986 Albrektson and Zarb criteria, what radiographic finding should be absent for implant success?
What is generally the limiting factor when considering implant placement in children and adolescents?
What is generally the limiting factor when considering implant placement in children and adolescents?
Around what age range does the pubertal growth period typically occur in males, which is a consideration for implant timing?
Around what age range does the pubertal growth period typically occur in males, which is a consideration for implant timing?
Why might earlier implant placement in adolescents lead to infraocclusion?
Why might earlier implant placement in adolescents lead to infraocclusion?
For an adolescent requiring a single tooth implant due to tooth loss, what is a critical consideration regarding the final restoration?
For an adolescent requiring a single tooth implant due to tooth loss, what is a critical consideration regarding the final restoration?
What is a primary indication for implant treatment in fully edentulous patients with severely resorbed ridges requiring enhanced retention?
What is a primary indication for implant treatment in fully edentulous patients with severely resorbed ridges requiring enhanced retention?
Which condition is considered a definitive contraindication for osseointegrated implant treatment?
Which condition is considered a definitive contraindication for osseointegrated implant treatment?
In patients who have had a high dose of radiation therapy, what radiation level makes implant placement contraindicated?
In patients who have had a high dose of radiation therapy, what radiation level makes implant placement contraindicated?
Why are radiographic examinations essential in dental implant planning?
Why are radiographic examinations essential in dental implant planning?
Which of the following is a limitation of using panoramic radiographs for implant planning?
Which of the following is a limitation of using panoramic radiographs for implant planning?
Which imaging modality is particularly useful for assessing the sagittal dimensions of the mandible and maxilla in implant planning?
Which imaging modality is particularly useful for assessing the sagittal dimensions of the mandible and maxilla in implant planning?
Why is magnetic resonance imaging not as widely used in oral implantology compared to other imaging techniques?
Why is magnetic resonance imaging not as widely used in oral implantology compared to other imaging techniques?
What advantage does cone-beam computed tomography (CBCT) offer over traditional panoramic radiographs for implant planning?
What advantage does cone-beam computed tomography (CBCT) offer over traditional panoramic radiographs for implant planning?
What is the purpose of using radiopaque markers in a template during panoramic radiography for implant planning?
What is the purpose of using radiopaque markers in a template during panoramic radiography for implant planning?
What is a significant advantage of interactive computerized tomography (EBT) in implant planning?
What is a significant advantage of interactive computerized tomography (EBT) in implant planning?
What is the primary benefit of using surgical stents created from interactive computerized tomography data?
What is the primary benefit of using surgical stents created from interactive computerized tomography data?
In taking a patient's medical history prior to implant placement, which condition is most critical to assess regarding potential complications?
In taking a patient's medical history prior to implant placement, which condition is most critical to assess regarding potential complications?
What aspect of a patient's dental history is important when considering implant placement?
What aspect of a patient's dental history is important when considering implant placement?
Why is assessing the amount of bone resorption important during the clinical examination?
Why is assessing the amount of bone resorption important during the clinical examination?
What is the purpose of evaluating the soft tissues, oral hygiene, periodontal health, and condition of the teeth and edentulous spaces during a clinical examination for implant placement?
What is the purpose of evaluating the soft tissues, oral hygiene, periodontal health, and condition of the teeth and edentulous spaces during a clinical examination for implant placement?
According to Lekholm and Zarb's classification, what does 'Group A' signify regarding bone quantity?
According to Lekholm and Zarb's classification, what does 'Group A' signify regarding bone quantity?
What is a characteristic of bone quality 'Class 1' according to Lekholm and Zarb's classification?
What is a characteristic of bone quality 'Class 1' according to Lekholm and Zarb's classification?
In cases classified as 'Group D' according to Lekholm and Zarb, what is a key surgical consideration?
In cases classified as 'Group D' according to Lekholm and Zarb, what is a key surgical consideration?
What does the term 'delayed implant placement' refer to?
What does the term 'delayed implant placement' refer to?
Esthetic outcomes in implant restorations are significantly influenced by:
Esthetic outcomes in implant restorations are significantly influenced by:
What can result from vertical bone resorption when placing implants?
What can result from vertical bone resorption when placing implants?
What situation necessitates an immediate implant procedure?
What situation necessitates an immediate implant procedure?
What is the biggest drawback of immediate implant restoration?
What is the biggest drawback of immediate implant restoration?
Which of the following statements is true regarding cantilever extensions in implant-supported prostheses?
Which of the following statements is true regarding cantilever extensions in implant-supported prostheses?
A patient requires restoration of the posterior mandible. If the opposing arch lacks second and third molars, what occlusal scheme is appropriate?
A patient requires restoration of the posterior mandible. If the opposing arch lacks second and third molars, what occlusal scheme is appropriate?
How should lateral stresses be adressed when creating implant-supported prosthetics?
How should lateral stresses be adressed when creating implant-supported prosthetics?
What is the primary goal of immediate temporization (provisionals ) ?
What is the primary goal of immediate temporization (provisionals ) ?
After 3 months if gum line has gone, what may be done to repair ?
After 3 months if gum line has gone, what may be done to repair ?
Which of the following is an advantage of using a screw-retained implant restoration?
Which of the following is an advantage of using a screw-retained implant restoration?
Regarding anterior placement of the implants which factor will need to be addressed first if having any concern?
Regarding anterior placement of the implants which factor will need to be addressed first if having any concern?
Flashcards
Dental Implants
Dental Implants
Structures replacing missing organs or tissues; in dentistry, supporting fixed or removable prostheses.
Osseointegration
Osseointegration
Titanium's ability to directly bond with bone at a chemical level.
Material Quality in Implants
Material Quality in Implants
Material purity impacts chemical bond with bone, using pure titanium to directly connect with bone
No Load Immediate (loading)
No Load Immediate (loading)
Signup and view all the flashcards
Patient Evaluation
Patient Evaluation
Signup and view all the flashcards
Implant Benefits
Implant Benefits
Signup and view all the flashcards
Success Criteria
Success Criteria
Signup and view all the flashcards
Growth restriction
Growth restriction
Signup and view all the flashcards
Bone Maturity
Bone Maturity
Signup and view all the flashcards
When to use Implants
When to use Implants
Signup and view all the flashcards
Reasons to Use Implants
Reasons to Use Implants
Signup and view all the flashcards
Contraindications
Contraindications
Signup and view all the flashcards
Planning
Planning
Signup and view all the flashcards
Radiographic Analysis with
Radiographic Analysis with
Signup and view all the flashcards
Surgical Stents
Surgical Stents
Signup and view all the flashcards
Medical History
Medical History
Signup and view all the flashcards
Oral evaluation
Oral evaluation
Signup and view all the flashcards
Lekholm and Zarb's assessments
Lekholm and Zarb's assessments
Signup and view all the flashcards
Anatomical structures
Anatomical structures
Signup and view all the flashcards
Type of Bone
Type of Bone
Signup and view all the flashcards
Split finger techniqu
Split finger techniqu
Signup and view all the flashcards
Positioning angled
Positioning angled
Signup and view all the flashcards
Better choice with internal
Better choice with internal
Signup and view all the flashcards
Non rigid
Non rigid
Signup and view all the flashcards
How abutments chosen
How abutments chosen
Signup and view all the flashcards
Use with abut materials
Use with abut materials
Signup and view all the flashcards
Simante vs cemented
Simante vs cemented
Signup and view all the flashcards
Restorations and Stress of Forces
Restorations and Stress of Forces
Signup and view all the flashcards
Support of cases.
Support of cases.
Signup and view all the flashcards
Canti levering.
Canti levering.
Signup and view all the flashcards
Need for implant.
Need for implant.
Signup and view all the flashcards
Full mouth rehab
Full mouth rehab
Signup and view all the flashcards
Hybrids
Hybrids
Signup and view all the flashcards
Vertical stability
Vertical stability
Signup and view all the flashcards
What to do.
What to do.
Signup and view all the flashcards
What to take on first
What to take on first
Signup and view all the flashcards
Digital
Digital
Signup and view all the flashcards
Waxed
Waxed
Signup and view all the flashcards
Study Notes
General Implant Information
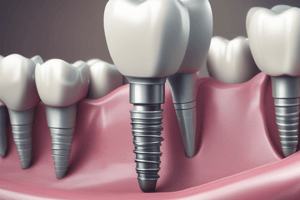
- An implant is a structure used to replace a missing organ or tissue in the general medical field.
- In dentistry, implants replace missing teeth or surrounding tissues supporting fixed or removable prostheses.
- Implants are biofunctional devices placed within or onto bone.
Implant History
- The concept of using foreign materials in the body for reconstructive and prosthetic purposes dates back a long time.
- Modern implant practices emerged after understanding the reactions of metals to body fluids, bone physiology, and tissues.
- Branemark introduced the concept of "Osseointegration" in the 1980s, based on his observations of titanium's relationship with bone in the 1960s; this concept is now widely accepted in implantology
- Osseointegration describes the direct connection between an implant and bone.
- In dentistry, the term "Tissue integration" highlights the importance of implants integrating well with surrounding tissues along with bone.
Four Key Factors for Successful Osseointegrated Implants
- Material properties: Pure titanium is preferred, forming a direct chemical bond with bone through a titanium oxide layer
- Implant shape: Branemark recommends screw-type implants for surface area and force distribution, but various shapes exist
- Surgical procedure: Requires special tools and techniques to minimize tissue damage
- Avoiding loading during healing: Implants should not be loaded to allow osseointegration, typically 3-4 months in the mandible and 4-6 months in the maxilla
Immediate Loading
- Protocols advocating immediate loading/immediate placement have emerged, suggesting that early loading can stimulate bone healing
- Primary stability and controlled force distribution are important.
Success Criteria for Implants
- Established in 1975 at the Harvard conference by Schnitman and Schulmann:
- Movement of less than 1 mm in any direction
- Bone loss not exceeding 1/3 of the implant's vertical height
- Manageable gingival inflammation without paresthesia, anesthesia, or damage to adjacent structures; no violation of anatomical structures.
- A functional service life of at least 75% within 5 years
Albrektson and Zarb's Standards (1986)
- The implant must be immobile when clinically tested
- No radiolucency should be visible on radiographs.
- Annual bone loss should not exceed 0.2 mm after the first year.
- Absence of pain, infection, neuropathies, paresthesia, or anatomical complications
Factors Ensuring Implant Success
- Proper patient assessment.
- Precision in implant placement
- Management of surrounding soft tissues
- Quality of prosthetic restoration
Advantages of Implant-Supported Prostheses
- Preserves bone.
- Maintains occlusal vertical dimension
- Provides esthetics
- Ensures proper occlusion
- Offers psychological support
- Restores proprioception
- Provides stability and retention
- Improves phonetics and muscle tone
Age Considerations for Implants
- Skeletal changes and osseointegrated implants behaving like ankylosed teeth make age a limiting factor in children and young patients.
- Controlled applications are possible with an understanding of growth and development.
Growth and Development
- Maxilla and mandible grow until puberty with the most rapid period during puberty.
- Puberty occurs around 12-14 in girls and 13-15 in boys.
- Sesamoid bone radiograph on the thumb is indicative of puberty.
- Jaw growth completes around age 18 in females and 20 in males.
Implants in Younger Patients
- Implants can remain shorter (infraposition) as adjacent teeth continue to erupt.
- Crown length differences can be managed with prosthetic methods.
- In young patients, growth needs to be considered, waiting until growth stabilizes (around 20 in females and 22 in males).
- Age has no upper limit for dental implants.
Indications for Implants
- Severely resorbed ridges requiring retention
- Single or double-sided edentulous ridges, particularly in young patients.
- Long edentulous spans.
- Situations where adjacent teeth should not be prepared
- Psychological or physiological intolerance to removable prostheses.
Additional Indications
- Oral muscle incoordination
- Low tissue tolerance
- Parafunctional habits affecting prosthesis stability
- High expectations from complete dentures.
- Hyperactive gag reflex.
Contraindications
- High-dose radiation exposure (>5000 Rad)
- Psychiatric disorders (psychosis, dysmorphophobia)
- Hemolytic disorders
- Rheumatic diseases, nephritis, heart diseases, hepatic cirrhosis, allergic conditions and immune deficiency.
- Untreated local infections.
- Soft or hard tissue pathologies.
- Substance abuse
Relative Contraindications
- Low-dose radiation (<4000 Rad)
- Alveolar bone diseases, periodontal diseases, relapsing oral mucosal diseases, temporomandibular dysfunctions, insufficient bone volume and anatomical malformations
Radiographic Examination
- Aids in assessing bone quality, quantity, and relationship to anatomical structures.
- Intraoral radiographs: periapical, occlusal
- Panoramic radiographs
- Lateral cephalometric radiographs
- Magnetic resonance imaging
- Computed tomography
- Interactive computed tomography.
Intraoral Radiographs
- Aid in localized assessment but are limited by distortion
Panoramic Radiographs
- Lateral cephalometric radiographs assist in sagittal assessment concerning bone height, width, and inclination, but are not commonly indicated due to distortion
- Allow assessment of all dental arches but suffer from magnification irregularities, geometric distortion, and limited detail
CT Scans
- Essential for assessing the bone's bukko-lingual width
- Lateral cephalometric radiographs-useful for sagittal assessment of the jaws but have limitations in implant planning
Magnetic Resonance Imaging
- Limited use in implant dentistry due to artifacts from metal
Computed Tomography (CT)
- It is vital for assessing height, thickness, and density of available bone.
- Special programs like Dental CT streamline the process and axial slices to facilitate implant planning.
- Essential for planning in anatomically sensitive regions. Interactive CT software enables clinicians to review tomographic data, facilitating measurements and implant placement simulation.
- The software allows simultaneous axial sagittal plus panoramic views or can create three-dimensional models.
Surgical Stents and Guides
- Facilitate precise implant placement based on the surgical plan.
- Bone or mucosa-supported options are available
Medical History
- Important for assessing general health and identifying potential risks
- Inquiring about rheumatic conditions, heart ailments, kidney diseases, liver conditions, allergies, and medication use
Dental History
- Assessing time and cause of tooth loss is significant along with evaluation of soft tissues and presence of pathologies
- The assessment of oral hygiene is important before implant operation.
Clinical Examination
- Evaluation of oral hygiene, soft tissues, and existing dentition concerning available bone, with special tools like calibrated probes
- Evaluate the condition of remaining teeth and perform periodontal treatment, if necessary.
Lekholm plus Zarb Classification
- This classifies bone quantity into five categories (A-E) and quality into four types (1-4).
- Type A: Minimal or no bone resorption
- Type B: Moderate bone resorption
- Type C: Significant resorption leaving only basal bone.
- Type D: Severe resorption extending into basal bone, requiring bone grafting
Bone Quality
- Classifies as 1, 2, 3 and 4 by Lekholm plus Zarb
- Class 1: Mostly cortical bone
- Class 2: Thick cortical layer surrounding trabecular bone.
- Class 3: Thin cortical layer with dense trabecular bone.
- Class 4: Thin cortical layer with low-density trabecular bone.
Anatomical Considerations During Implant Placement
- Maintain a minimum of 1 mm distance between the implant apex and anatomical structures
Surgical Approaches
- Approaches depend on the time from tooth loss to implant placement: immediate, delayed, or late.
- Delayed implant placement allows for ridge resorption, potentially complicating implant placement.
- Immediate implant placement immediately after extraction can be done if the extraction site is suitable.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.