Podcast
Questions and Answers
In what ways does smoking and radiotherapy impact the success rate of dental implants?
In what ways does smoking and radiotherapy impact the success rate of dental implants?
Smoking and radiotherapy are associated with a higher risk of implant failure, with smoking increasing the risk by 35% and radiotherapy increasing the risk by 70%.
What systemic conditions may modify the treatment plan for dental implants?
What systemic conditions may modify the treatment plan for dental implants?
Systemic conditions such as uncontrolled hypertension, intake of anticoagulants, patients on bisphosphonate therapy, or patients with psychiatric conditions may modify the treatment plan for dental implants.
Is poor glycemic control an absolute contraindication for implant therapy for patients with diabetes?
Is poor glycemic control an absolute contraindication for implant therapy for patients with diabetes?
No, poor glycemic control is not an absolute contraindication for implant therapy for patients with diabetes, provided that appropriate accommodation for delays in implant integration are considered.
Why is a thorough systemic evaluation important prior to planning for dental implants?
Why is a thorough systemic evaluation important prior to planning for dental implants?
What is the increased risk of dental implant failure for smokers compared to nonsmokers?
What is the increased risk of dental implant failure for smokers compared to nonsmokers?
Why is a thorough periodontal examination crucial before implant therapy?
Why is a thorough periodontal examination crucial before implant therapy?
What is the impact of a history of periodontitis on the risk of implant failure and bone loss?
What is the impact of a history of periodontitis on the risk of implant failure and bone loss?
What significant risk factor for dental implant failure is mentioned in the text?
What significant risk factor for dental implant failure is mentioned in the text?
What are the consequences of a lack of keratinized mucosa around dental implants?
What are the consequences of a lack of keratinized mucosa around dental implants?
What bone volume is necessary for standard implants?
What bone volume is necessary for standard implants?
What specific examination should be performed for implant placement?
What specific examination should be performed for implant placement?
What factors should be considered in the esthetic analysis of an implant patient?
What factors should be considered in the esthetic analysis of an implant patient?
Why is evaluation for proximity to anatomical structures essential?
Why is evaluation for proximity to anatomical structures essential?
What adjunctive diagnostic assessments aid in diagnosis and treatment planning?
What adjunctive diagnostic assessments aid in diagnosis and treatment planning?
Flashcards are hidden until you start studying
Study Notes
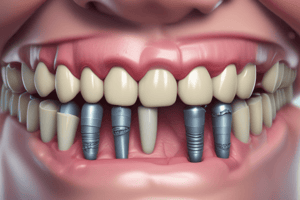
Dental Implant Site Preparation and Evaluation
- Smokers have a two times higher risk for dental implant failure than nonsmokers.
- Peri-implantitis incidence is higher in smokers compared to nonsmokers.
- Thorough periodontal examination before implant therapy is crucial for assessing disease status, oral hygiene, and mucogingival parameters.
- Patients with a history of periodontitis, aggressive form especially, are at higher risk for implant failure and bone loss.
- Poor oral hygiene is a significant risk factor for dental implant failure.
- Lack of keratinized mucosa around dental implants leads to plaque buildup, inflammation, and recession.
- For standard implants, adequate bone volume both buccopalatally/-lingually and apico-coronally is necessary.
- Site-specific examination, including evaluating bone height and width, should be performed.
- Guidelines for implant placement include minimum distances from adjacent teeth and sufficient space for restoration.
- Esthetic analysis of an implant patient should consider smile line, gingival phenotype, tooth size, space distribution, crown shape, and occlusal assessment.
- Evaluation for proximity to anatomical structures in the maxilla and mandible is essential.
- Adjunctive diagnostic assessments such as imaging, diagnostic wax-up, and clinical photographs aid in diagnosis and treatment planning.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.