Podcast
Questions and Answers
What is the effect of using metal instruments on polished titanium?
What is the effect of using metal instruments on polished titanium?
- Decreases surface roughness
- Has no effect on surface roughness
- Removes hard deposits
- Increases surface roughness (correct)
What is the purpose of selectively polishing the prosthesis and abutments?
What is the purpose of selectively polishing the prosthesis and abutments?
- To evaluate implant stability
- To remove hard deposits
- To smooth out the surface (correct)
- To increase surface roughness
What is the significance of implant mobility?
What is the significance of implant mobility?
- Is highly specific for the detection of implant failure (correct)
- Indicates implant stability
- Indicates osseointegration
- Is not a reliable measure of implant stability
What is the purpose of impact resistance and resonance frequency analysis?
What is the purpose of impact resistance and resonance frequency analysis?
What does an increase in RFA value indicate?
What does an increase in RFA value indicate?
What is the cardinal sign of implant failure?
What is the cardinal sign of implant failure?
What is the primary focus of long-term success of implants?
What is the primary focus of long-term success of implants?
What is the recommended frequency of recall maintenance visits for the first year after treatment?
What is the recommended frequency of recall maintenance visits for the first year after treatment?
What is included in the clinical examination step of implant maintenance?
What is included in the clinical examination step of implant maintenance?
What is the purpose of routine maintenance, recall evaluations, and radiographs?
What is the purpose of routine maintenance, recall evaluations, and radiographs?
What is evaluated during the dental implant examination?
What is evaluated during the dental implant examination?
What is the purpose of medical and dental history in implant maintenance?
What is the purpose of medical and dental history in implant maintenance?
What is the primary goal of peri-implant oral hygiene during the early postoperative phase of healing?
What is the primary goal of peri-implant oral hygiene during the early postoperative phase of healing?
What is the characteristic of peri-implant mucosal health?
What is the characteristic of peri-implant mucosal health?
What is the purpose of the rubber tip stimulator in peri-implant maintenance?
What is the purpose of the rubber tip stimulator in peri-implant maintenance?
What is the significance of keratinized, attached gingiva in peri-implant health?
What is the significance of keratinized, attached gingiva in peri-implant health?
What is the purpose of AIRFLOW® with PLUS powder in peri-implant maintenance?
What is the purpose of AIRFLOW® with PLUS powder in peri-implant maintenance?
What is the indication of bleeding on probing at implant sites?
What is the indication of bleeding on probing at implant sites?
What is the typical indication of a solid resonating sound from implant percussion?
What is the typical indication of a solid resonating sound from implant percussion?
What is the primary purpose of evaluating implant restorations after delivery?
What is the primary purpose of evaluating implant restorations after delivery?
Why are periapical radiographs taken during different stages of implant treatment?
Why are periapical radiographs taken during different stages of implant treatment?
What is the primary difference between peri-mucositis and peri-implantitis?
What is the primary difference between peri-mucositis and peri-implantitis?
Why are occlusal guards recommended in patients with oral parafunctions and heavy occlusal forces?
Why are occlusal guards recommended in patients with oral parafunctions and heavy occlusal forces?
What is the significance of embrasure spaces in implant restorations?
What is the significance of embrasure spaces in implant restorations?
What is the primary characteristic of peri-implantitis?
What is the primary characteristic of peri-implantitis?
What is the primary goal of peri-implant mucositis treatment?
What is the primary goal of peri-implant mucositis treatment?
What is the role of antimicrobials in peri-implant mucositis treatment?
What is the role of antimicrobials in peri-implant mucositis treatment?
What is a surgical intervention for peri-implantitis?
What is a surgical intervention for peri-implantitis?
What is the consequence of untreated peri-implantitis?
What is the consequence of untreated peri-implantitis?
What is the primary objective of treating peri-implantitis?
What is the primary objective of treating peri-implantitis?
What is the primary purpose of using non-metal ultrasonic tips and Teflon-coated curettes on titanium implants?
What is the primary purpose of using non-metal ultrasonic tips and Teflon-coated curettes on titanium implants?
Which of the following techniques is originally designed to evaluate tooth mobility quantitatively?
Which of the following techniques is originally designed to evaluate tooth mobility quantitatively?
What is the significance of detecting implant mobility?
What is the significance of detecting implant mobility?
What is the primary advantage of using a rubber cup and non-abrasive polishing paste for polishing the prosthesis and abutments?
What is the primary advantage of using a rubber cup and non-abrasive polishing paste for polishing the prosthesis and abutments?
What is the primary difference between impact resistance and resonance frequency analysis?
What is the primary difference between impact resistance and resonance frequency analysis?
What is the primary factor that determines the frequency of recall maintenance visits after the first year of treatment?
What is the primary factor that determines the frequency of recall maintenance visits after the first year of treatment?
What is the purpose of evaluating the occlusal relationships during the implant examination?
What is the purpose of evaluating the occlusal relationships during the implant examination?
What is the primary focus of the dental team's administration of professional prophylaxis procedures?
What is the primary focus of the dental team's administration of professional prophylaxis procedures?
What is the significance of evaluating the presence of plaque and calculus during the dental implant examination?
What is the significance of evaluating the presence of plaque and calculus during the dental implant examination?
What is the primary goal of the medical and dental history evaluation during implant maintenance?
What is the primary goal of the medical and dental history evaluation during implant maintenance?
What is the primary characteristic of peri-implantitis?
What is the primary characteristic of peri-implantitis?
What is the most critical factor in preventing peri-implant disease?
What is the most critical factor in preventing peri-implant disease?
What is the goal of treatment for peri-implant mucositis?
What is the goal of treatment for peri-implant mucositis?
What is the primary benefit of using AIRFLOW with PLUS powder in peri-implant maintenance?
What is the primary benefit of using AIRFLOW with PLUS powder in peri-implant maintenance?
What is the role of antimicrobials in peri-implant mucositis treatment?
What is the role of antimicrobials in peri-implant mucositis treatment?
What is the characteristic of peri-implant mucosal health?
What is the characteristic of peri-implant mucosal health?
What is a surgical intervention for peri-implantitis?
What is a surgical intervention for peri-implantitis?
When should biofilm control begin for implants?
When should biofilm control begin for implants?
What is the consequence of untreated peri-implantitis?
What is the consequence of untreated peri-implantitis?
What is the indication of bleeding on probing at implant sites?
What is the indication of bleeding on probing at implant sites?
What is the purpose of evaluating implant restorations after delivery?
What is the purpose of evaluating implant restorations after delivery?
What is the significance of a dull sound during implant percussion?
What is the significance of a dull sound during implant percussion?
What is the primary tool for detection of failed or failing implants in routine clinical evaluations?
What is the primary tool for detection of failed or failing implants in routine clinical evaluations?
Why are occlusal guards recommended in patients with oral parafunctions and heavy occlusal forces?
Why are occlusal guards recommended in patients with oral parafunctions and heavy occlusal forces?
What is the primary difference between peri-mucositis and peri-implantitis?
What is the primary difference between peri-mucositis and peri-implantitis?
Flashcards are hidden until you start studying
Study Notes
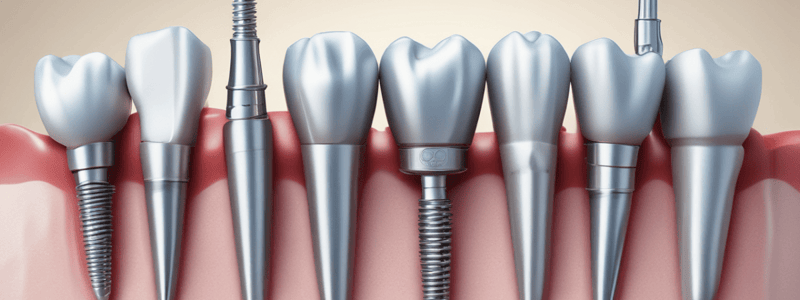
Instrument Selection for Titanium Implants
- Metal instruments, including metal curettes and scalers, and ultrasonic scalers increase the surface roughness of polished titanium.
- Plastic, Teflon-coated, and carbon and gold-coated curettes and non-metal ultrasonic tips are recommended for titanium implant scalers.
Polishing
- The prosthesis and abutments may be selectively polished with a rubber cup and non-abrasive polishing paste such as aluminum oxide, tin oxide, acidulated phosphate sodium fluoride (APF)-free prophy paste, and low-abrasive dentifrice after hard deposits have been removed.
Stability Measures
- The assessment of implant stability or mobility is an important measure for determining whether osseointegration is being maintained.
- Mobility is highly specific for the detection of implant failure or lack of osseointegration.
- Two non-invasive techniques for evaluating implant stability are impact resistance (e.g., Periotest) and resonance frequency analysis (RFA).
- Periotest is a non-invasive electronic device that provides an objective measurement of the reaction of the periodontium to a defined impact load applied to the tooth crown.
- Resonance frequency analysis uses a transducer attached to the implant or abutment to measure the response to a steady-state signal.
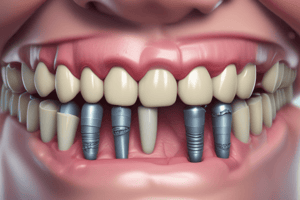
Implant Maintenance
- Periodic evaluation of implants, surrounding tissue, and oral hygiene is vital to the long-term success of the dental implant.
- Recall maintenance visits should be scheduled at 3-month intervals for the first year after treatment, and then adjusted to suit the patient's needs.
Examination of Implant
- Patient history: look for changes in systemic risk factors (e.g., diabetes, smoking, medications).
- Clinical examination: extraoral and intraoral examination, oral soft tissue evaluation, tooth mobility, fremitus, occlusion, and caries restorative factors.
- Investigation and X-ray: radiographic examination to assess peri-implant crestal bone level.
Step-by-Step Implant Examination
- Presence of plaque and calculus
- Probing depths
- Bleeding on probing
- Implant stability
- Occlusal evaluation
- Other signs and symptoms of disease
Evaluation of Biofilm Control
- Poor biofilm control is associated with peri-implant disease.
- Visualization of plaque and calculus is essential for effective biofilm control.
- Methods for patient oral hygiene:
- Cotton tip, cotton gauze, or soft toothbrush to gently remove biofilm from healing abutments or provisional restorations.
- Avoid using powered toothbrushes before implant osseointegration.
- The rubber tip stimulator can be used to stimulate blood flow.
- AIRFLOW with PLUS powder is minimally invasive and does not scratch implant surfaces, abutments, or prosthesis.
Evaluation of Peri-Implant Health and Disease
- Peri-implant mucosal health is characterized by pink, firm, and well-adapted gingival tissue.
- Peri-implant disease is associated with clinical erythema, edema, and loss of tissue tightness around the implant.
- Peri-implant probing: bleeding on probing at implant sites can indicate inflammation.
Scaling and Implant Percussion
- Removal of dental biofilm and calculus from implant components exposed to the oral environment.
- Tapping an implant's healing abutment or restoration with an instrument produces a sound that can help determine its osseointegration.
Evaluation of Implant Restorations
- Implant superstructures and restorations should be fabricated to accommodate and facilitate oral hygiene.
- After delivery, cement-retained implant restorations should be thoroughly evaluated for residual excess cement, which must be removed.
- During follow-up visits, implant restorations should be carefully examined for heavy contacts, fractures, loose screws, and occlusion should be adjusted accordingly to prevent implant overload and fractures.
Radiographic Examination
- Intraoral periapical radiographs should be taken at implant placement, abutment connection, and final restoration.
- Radiographic examination remains one of the primary tools for detection of failed or failing implants in routine clinical evaluations.
Peri-Implant Mucositis and Peri-Implantitis
- Peri-implant mucositis is the inflammatory reaction of the soft tissues surrounding an implant, with no signs of loss of supporting bone.
- Peri-implantitis is a destructive inflammatory process around an osseointegrated implant that leads to peri-implant pocket formation and progressive loss of supporting bone.
- Treatment of peri-implant mucositis and peri-implantitis includes nonsurgical and surgical interventions.
Instrument Selection for Titanium Implants
- Metal instruments, including metal curettes and scalers, and ultrasonic scalers increase the surface roughness of polished titanium.
- Plastic, Teflon-coated, and carbon and gold-coated curettes and non-metal ultrasonic tips are recommended for titanium implant scalers.
Polishing
- The prosthesis and abutments may be selectively polished with a rubber cup and non-abrasive polishing paste such as aluminum oxide, tin oxide, acidulated phosphate sodium fluoride (APF)-free prophy paste, and low-abrasive dentifrice after hard deposits have been removed.
Stability Measures
- The assessment of implant stability or mobility is an important measure for determining whether osseointegration is being maintained.
- Mobility is highly specific for the detection of implant failure or lack of osseointegration.
- Two non-invasive techniques for evaluating implant stability are impact resistance (e.g., Periotest) and resonance frequency analysis (RFA).
- Periotest is a non-invasive electronic device that provides an objective measurement of the reaction of the periodontium to a defined impact load applied to the tooth crown.
- Resonance frequency analysis uses a transducer attached to the implant or abutment to measure the response to a steady-state signal.
Implant Maintenance
- Periodic evaluation of implants, surrounding tissue, and oral hygiene is vital to the long-term success of the dental implant.
- Recall maintenance visits should be scheduled at 3-month intervals for the first year after treatment, and then adjusted to suit the patient's needs.
Examination of Implant
- Patient history: look for changes in systemic risk factors (e.g., diabetes, smoking, medications).
- Clinical examination: extraoral and intraoral examination, oral soft tissue evaluation, tooth mobility, fremitus, occlusion, and caries restorative factors.
- Investigation and X-ray: radiographic examination to assess peri-implant crestal bone level.
Step-by-Step Implant Examination
- Presence of plaque and calculus
- Probing depths
- Bleeding on probing
- Implant stability
- Occlusal evaluation
- Other signs and symptoms of disease
Evaluation of Biofilm Control
- Poor biofilm control is associated with peri-implant disease.
- Visualization of plaque and calculus is essential for effective biofilm control.
- Methods for patient oral hygiene:
- Cotton tip, cotton gauze, or soft toothbrush to gently remove biofilm from healing abutments or provisional restorations.
- Avoid using powered toothbrushes before implant osseointegration.
- The rubber tip stimulator can be used to stimulate blood flow.
- AIRFLOW with PLUS powder is minimally invasive and does not scratch implant surfaces, abutments, or prosthesis.
Evaluation of Peri-Implant Health and Disease
- Peri-implant mucosal health is characterized by pink, firm, and well-adapted gingival tissue.
- Peri-implant disease is associated with clinical erythema, edema, and loss of tissue tightness around the implant.
- Peri-implant probing: bleeding on probing at implant sites can indicate inflammation.
Scaling and Implant Percussion
- Removal of dental biofilm and calculus from implant components exposed to the oral environment.
- Tapping an implant's healing abutment or restoration with an instrument produces a sound that can help determine its osseointegration.
Evaluation of Implant Restorations
- Implant superstructures and restorations should be fabricated to accommodate and facilitate oral hygiene.
- After delivery, cement-retained implant restorations should be thoroughly evaluated for residual excess cement, which must be removed.
- During follow-up visits, implant restorations should be carefully examined for heavy contacts, fractures, loose screws, and occlusion should be adjusted accordingly to prevent implant overload and fractures.
Radiographic Examination
- Intraoral periapical radiographs should be taken at implant placement, abutment connection, and final restoration.
- Radiographic examination remains one of the primary tools for detection of failed or failing implants in routine clinical evaluations.
Peri-Implant Mucositis and Peri-Implantitis
- Peri-implant mucositis is the inflammatory reaction of the soft tissues surrounding an implant, with no signs of loss of supporting bone.
- Peri-implantitis is a destructive inflammatory process around an osseointegrated implant that leads to peri-implant pocket formation and progressive loss of supporting bone.
- Treatment of peri-implant mucositis and peri-implantitis includes nonsurgical and surgical interventions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.