Podcast
Questions and Answers
What is the primary cause of Cushing's syndrome?
What is the primary cause of Cushing's syndrome?
- Excessive adrenaline production
- Excessive insulin production
- Excessive aldosterone production
- Excessive cortisol production (correct)
Cushing's disease is characterized by excessive production of cortisol from the adrenal glands.
Cushing's disease is characterized by excessive production of cortisol from the adrenal glands.
False (B)
Which hormone does the hypothalamus release to initiate cortisol production?
Which hormone does the hypothalamus release to initiate cortisol production?
Corticotropin-releasing hormone (CRH)
High cortisol levels can lead to __________ hypertension.
High cortisol levels can lead to __________ hypertension.
Match the following effects of high cortisol with their descriptions:
Match the following effects of high cortisol with their descriptions:
Which effect does high cortisol have on blood sugar levels?
Which effect does high cortisol have on blood sugar levels?
Cortisol contributes to increased insulin sensitivity and a lower risk of diabetes mellitus.
Cortisol contributes to increased insulin sensitivity and a lower risk of diabetes mellitus.
What are the characteristic features of fat redistribution caused by high cortisol?
What are the characteristic features of fat redistribution caused by high cortisol?
High cortisol inhibits __________ synthesis, leading to a higher risk of osteoporosis.
High cortisol inhibits __________ synthesis, leading to a higher risk of osteoporosis.
What effect does high cortisol have on the sympathetic nervous system?
What effect does high cortisol have on the sympathetic nervous system?
Which feature is NOT characteristic of Cushing's Syndrome?
Which feature is NOT characteristic of Cushing's Syndrome?
Cushing's Disease is characterized by high ACTH levels due to adrenal tumors.
Cushing's Disease is characterized by high ACTH levels due to adrenal tumors.
What test measures free cortisol levels to help diagnose Cushing's Syndrome?
What test measures free cortisol levels to help diagnose Cushing's Syndrome?
Excess cortisol can lead to increased susceptibility to __________.
Excess cortisol can lead to increased susceptibility to __________.
Match the following terms with their correct descriptions:
Match the following terms with their correct descriptions:
Which symptom is typically associated with Cushing's Syndrome?
Which symptom is typically associated with Cushing's Syndrome?
Salivary cortisol measurement is an effective alternative method to detect cortisol levels.
Salivary cortisol measurement is an effective alternative method to detect cortisol levels.
What is the primary treatment approach for pituitary tumors causing Cushing's Disease?
What is the primary treatment approach for pituitary tumors causing Cushing's Disease?
Patients with Cushing's Syndrome often experience __________ obesity.
Patients with Cushing's Syndrome often experience __________ obesity.
What effect does high cortisol levels have on GnRH production?
What effect does high cortisol levels have on GnRH production?
What is a common feature of Cushing's Syndrome?
What is a common feature of Cushing's Syndrome?
Low GnRH levels lead to increased FSH and LH levels.
Low GnRH levels lead to increased FSH and LH levels.
Which hormone is primarily responsible for stimulating the adrenal cortex to produce cortisol?
Which hormone is primarily responsible for stimulating the adrenal cortex to produce cortisol?
Name one diagnostic test used to screen for Cushing's Syndrome.
Name one diagnostic test used to screen for Cushing's Syndrome.
Cushing's disease specifically refers to the overproduction of cortisol alone.
Cushing's disease specifically refers to the overproduction of cortisol alone.
What are two common physical characteristics of fat redistribution in individuals with high cortisol levels?
What are two common physical characteristics of fat redistribution in individuals with high cortisol levels?
The appearance of __________ in the abdomen is a sign of decreased collagen strength.
The appearance of __________ in the abdomen is a sign of decreased collagen strength.
Match the following symptoms with Cushing's Syndrome:
Match the following symptoms with Cushing's Syndrome:
High levels of cortisol can lead to __________, which is often resistant to treatment.
High levels of cortisol can lead to __________, which is often resistant to treatment.
What is a significant effect of high cortisol on the immune system?
What is a significant effect of high cortisol on the immune system?
Which of the following describes a finding in patients with Cushing's Syndrome?
Which of the following describes a finding in patients with Cushing's Syndrome?
Match the following effects of high cortisol with their outcomes:
Match the following effects of high cortisol with their outcomes:
A high-dose dexamethasone test cannot help differentiate between pituitary and ectopic ACTH sources.
A high-dose dexamethasone test cannot help differentiate between pituitary and ectopic ACTH sources.
What is the primary treatment for adrenal tumors in Cushing's Syndrome?
What is the primary treatment for adrenal tumors in Cushing's Syndrome?
Cortisol production is influenced by the hypothalamus and adrenal cortex, but not the pituitary gland.
Cortisol production is influenced by the hypothalamus and adrenal cortex, but not the pituitary gland.
What metabolic effect does high cortisol have on blood sugar levels?
What metabolic effect does high cortisol have on blood sugar levels?
Elevated cortisol levels in urine may indicate __________ Syndrome or Cushing's Disease.
Elevated cortisol levels in urine may indicate __________ Syndrome or Cushing's Disease.
What complication can arise from decreased collagen in the dermis?
What complication can arise from decreased collagen in the dermis?
High cortisol induces __________, leading to muscle wasting.
High cortisol induces __________, leading to muscle wasting.
Which of the following conditions can result from prolonged exposure to high cortisol levels?
Which of the following conditions can result from prolonged exposure to high cortisol levels?
What is a primary consequence of high cortisol levels on the cardiovascular system?
What is a primary consequence of high cortisol levels on the cardiovascular system?
Elevated cortisol levels can suppress immune function and increase susceptibility to infections.
Elevated cortisol levels can suppress immune function and increase susceptibility to infections.
What hormone is released by the anterior pituitary in response to CRH?
What hormone is released by the anterior pituitary in response to CRH?
High cortisol can lead to secondary __________ that is resistant to usual treatments.
High cortisol can lead to secondary __________ that is resistant to usual treatments.
Match the effects of high cortisol with their outcomes:
Match the effects of high cortisol with their outcomes:
Which of the following is NOT a characteristic physical feature associated with Cushing's Syndrome?
Which of the following is NOT a characteristic physical feature associated with Cushing's Syndrome?
Cushing's disease refers to excessive production of cortisol from the adrenal cortex.
Cushing's disease refers to excessive production of cortisol from the adrenal cortex.
High cortisol levels can promote gluconeogenesis and lead to __________ in the blood.
High cortisol levels can promote gluconeogenesis and lead to __________ in the blood.
What body feature is often described by the term 'buffalo hump'?
What body feature is often described by the term 'buffalo hump'?
What metabolic effect does cortisol have on muscle tissue?
What metabolic effect does cortisol have on muscle tissue?
What is a classic feature associated with Cushing's Syndrome?
What is a classic feature associated with Cushing's Syndrome?
Low ACTH levels indicate a primary adrenal problem.
Low ACTH levels indicate a primary adrenal problem.
What is the effect of high cortisol levels on muscle strength?
What is the effect of high cortisol levels on muscle strength?
Cushing's disease is characterized by high levels of ________ due to a pituitary adenoma.
Cushing's disease is characterized by high levels of ________ due to a pituitary adenoma.
Match the following symptoms of Cushing's Syndrome with their descriptions:
Match the following symptoms of Cushing's Syndrome with their descriptions:
Which diagnostic test helps to evaluate urine cortisol levels over 24 hours?
Which diagnostic test helps to evaluate urine cortisol levels over 24 hours?
High doses of dexamethasone can suppress cortisol levels in cases of ectopic ACTH sources.
High doses of dexamethasone can suppress cortisol levels in cases of ectopic ACTH sources.
What are two common diagnostic markers suggesting Cushing's Syndrome?
What are two common diagnostic markers suggesting Cushing's Syndrome?
The __________ hormone from the hypothalamus stimulates ACTH production from the pituitary gland.
The __________ hormone from the hypothalamus stimulates ACTH production from the pituitary gland.
What is the primary treatment approach for adrenal tumors in Cushing's Syndrome?
What is the primary treatment approach for adrenal tumors in Cushing's Syndrome?
What effect does high cortisol have on heart rate?
What effect does high cortisol have on heart rate?
Cushing's disease results from excessive cortisol production from the adrenal glands.
Cushing's disease results from excessive cortisol production from the adrenal glands.
Name one characteristic physical feature associated with fat redistribution due to high cortisol levels.
Name one characteristic physical feature associated with fat redistribution due to high cortisol levels.
High cortisol can lead to a predisposition to __________ infections.
High cortisol can lead to a predisposition to __________ infections.
Match the following effects of high cortisol to their corresponding outcomes:
Match the following effects of high cortisol to their corresponding outcomes:
Which of the following describes a metabolic effect of cortisol?
Which of the following describes a metabolic effect of cortisol?
High cortisol levels enhance immune function and increase resistance to infections.
High cortisol levels enhance immune function and increase resistance to infections.
What is the primary source of excessive ACTH production in Cushing's disease?
What is the primary source of excessive ACTH production in Cushing's disease?
Cortisol induces __________, which leads to muscle wasting.
Cortisol induces __________, which leads to muscle wasting.
Match the complications of high cortisol with their descriptions:
Match the complications of high cortisol with their descriptions:
Which of the following symptoms is commonly associated with Cushing's Syndrome?
Which of the following symptoms is commonly associated with Cushing's Syndrome?
High cortisol levels can suppress the immune system, increasing susceptibility to infections.
High cortisol levels can suppress the immune system, increasing susceptibility to infections.
What test is commonly used to measure free cortisol levels in patients suspected of having Cushing's Syndrome?
What test is commonly used to measure free cortisol levels in patients suspected of having Cushing's Syndrome?
Decreased collagen strength in bones contributes to __________ bone structure.
Decreased collagen strength in bones contributes to __________ bone structure.
Match the clinical features with their correct descriptions:
Match the clinical features with their correct descriptions:
What effect does excessive cortisol have on GnRH production?
What effect does excessive cortisol have on GnRH production?
Women with Cushing's Syndrome may experience menstrual irregularities as a result of low GnRH levels.
Women with Cushing's Syndrome may experience menstrual irregularities as a result of low GnRH levels.
What diagnostic test can be performed to differentiate between pituitary tumors and ectopic ACTH production?
What diagnostic test can be performed to differentiate between pituitary tumors and ectopic ACTH production?
One common appearance associated with decreased collagen levels in the skin is __________.
One common appearance associated with decreased collagen levels in the skin is __________.
Which of the following treatments may be used for adrenal tumors?
Which of the following treatments may be used for adrenal tumors?
What is the primary hormone that CRH stimulates the anterior pituitary to release?
What is the primary hormone that CRH stimulates the anterior pituitary to release?
Cushing's disease is characterized by excessive cortisol production from the adrenal glands.
Cushing's disease is characterized by excessive cortisol production from the adrenal glands.
What characteristic physical manifestations can be associated with fat redistribution in individuals experiencing high cortisol levels?
What characteristic physical manifestations can be associated with fat redistribution in individuals experiencing high cortisol levels?
High cortisol levels can lead to __________ obesity, characterized by a specific body fat distribution.
High cortisol levels can lead to __________ obesity, characterized by a specific body fat distribution.
Match the metabolic effects of high cortisol with their descriptions:
Match the metabolic effects of high cortisol with their descriptions:
Which of the following is a potential complication resulting from prolonged high cortisol levels?
Which of the following is a potential complication resulting from prolonged high cortisol levels?
Excessive cortisol has an immunosuppressive effect, increasing susceptibility to fungal infections.
Excessive cortisol has an immunosuppressive effect, increasing susceptibility to fungal infections.
Which symptom is commonly observed in individuals with Cushing's Syndrome?
Which symptom is commonly observed in individuals with Cushing's Syndrome?
What is the function of ACTH in the hormonal pathway related to cortisol production?
What is the function of ACTH in the hormonal pathway related to cortisol production?
High levels of cortisol can lead to __________, resulting in muscle atrophy, especially in proximal muscles.
High levels of cortisol can lead to __________, resulting in muscle atrophy, especially in proximal muscles.
Cushing's Syndrome can be caused by chronic steroid use.
Cushing's Syndrome can be caused by chronic steroid use.
Name one clinical feature associated with muscle weakness in Cushing's Syndrome.
Name one clinical feature associated with muscle weakness in Cushing's Syndrome.
What effect does high cortisol have on the sympathetic nervous system?
What effect does high cortisol have on the sympathetic nervous system?
Excess cortisol can lead to the condition known as __________, which is characterized by resistance to usual treatment.
Excess cortisol can lead to the condition known as __________, which is characterized by resistance to usual treatment.
Match the following types of tests with their purposes in diagnosing Cushing's Syndrome:
Match the following types of tests with their purposes in diagnosing Cushing's Syndrome:
What does a high ACTH level suggest in the context of Cushing's Disease?
What does a high ACTH level suggest in the context of Cushing's Disease?
Men with Cushing's Syndrome tend to have increased testosterone production.
Men with Cushing's Syndrome tend to have increased testosterone production.
What body part is associated with the term 'buffalo hump'?
What body part is associated with the term 'buffalo hump'?
Cushing's Disease often leads to hirsutism and __________ due to excess androgens.
Cushing's Disease often leads to hirsutism and __________ due to excess androgens.
Which of the following is a common complication resulting from decreased collagen in the skin?
Which of the following is a common complication resulting from decreased collagen in the skin?
Flashcards are hidden until you start studying
Study Notes
Cushing's Syndrome and Cushing's Disease
- Cushing's syndrome results from excessive cortisol production.
- Cushing's disease specifically refers to excessive ACTH production from the anterior pituitary gland.
- Cortisol production involves the hypothalamus, anterior pituitary, and adrenal cortex.
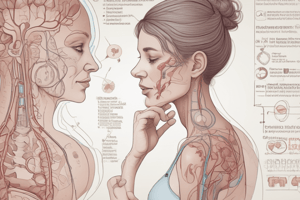
Hormonal Pathway
- Hypothalamus releases corticotropin-releasing hormone (CRH).
- CRH stimulates anterior pituitary to produce adrenocorticotropic hormone (ACTH).
- ACTH triggers adrenal cortex, specifically the zona fasciculata, to produce cortisol.
Effects of High Cortisol Levels
- High cortisol enhances the activity and sensitivity of the sympathetic nervous system.
- Increases heart rate and stroke volume via beta-1 adrenergic receptors, raising blood pressure.
- Activates alpha-1 adrenergic receptors in blood vessels, promoting vasoconstriction.
Secondary Hypertension
- High cortisol can lead to secondary hypertension that is resistant to conventional anti-hypertensive therapy.
Immune System Suppression
- High cortisol inhibits neutrophil margination, compromising infection response.
- Suppresses T-cell proliferation, reducing overall immune function.
- Results in increased susceptibility to infections, especially fungal infections.
Metabolic and Endocrine Effects
- Cortisol promotes gluconeogenesis and glycogenolysis in the liver, raising blood sugar levels (hyperglycemia).
- May lead to increased insulin resistance and risk of developing diabetes mellitus (diabetogenic effect).
Lipid and Protein Metabolism
- Cortisol induces lipolysis but redistributes fat from extremities to central body, causing obesity in the abdomen and face.
- Characteristic features include moon facies, buffalo hump, and significant abdominal obesity.
Muscle and Bone Effects
- High cortisol leads to muscle wasting (atrophy), particularly affecting proximal muscles.
- Inhibits collagen synthesis, resulting in osteopenia and increasing the risk of osteoporosis and fractures.
- The reduction in collagen strength in bones contributes to fragile bone structure.
Clinical Implications
- Classic features of Cushing's Syndrome:
- Hypertension refractory to treatment.
- Increased risk for infections.
- Hyperglycemia and potential diabetes.
- Distinctive body fat distribution changes (moon facies, buffalo hump).
- Muscle weakness and susceptibility to fractures.### Cushing Syndrome and Its Effects
- Atrophy and muscle weakness primarily affect the proximal muscles.
- Collagen in the dermis is crucial for skin integrity and tensile strength; decreased collagen leads to thin skin.
- Thinning skin increases the risk of:
- Striae: Commonly seen in the abdomen.
- Ecchymosis: Bruising appearance on skin due to fragility.
- Slow wound healing: Impaired by reduced collagen and immune response.
- Symptoms of Cushing syndrome include:
- Abdominal obesity
- Thin skin with visible striae or bruising
- Potential for muscle myopathy and increased fracture risk.
Endocrine and Reproductive Effects
- Excess cortisol inhibits the production of GnRH from the hypothalamus.
- Low GnRH leads to decreased FSH and LH levels, resulting in:
- Men in reproductive health: Reduced libido and testosterone production.
- Women in reproductive health: Menstrual irregularities or amenorrhea.
Key Clinical Signs of Cushing Syndrome
- Fat Redistribution Features:
- Moon facies: Rounding of facial features.
- Buffalo hump: Fat accumulation at the nape of the neck.
- Changes in collagen lead to thin skin, striae, ecchymosis, and wound healing complications.
- High cortisol levels can cause secondary hypertension and increased susceptibility to infections.
Cushing's Disease vs. Cushing's Syndrome
- Cushing's Disease: High ACTH levels, usually from a pituitary adenoma, may lead to excess androgens (causing hirsutism and acne) and hyperpigmentation.
- Cushing's Syndrome: High cortisol levels due to adrenal tumors (adenoma or carcinoma) or iatrogenic causes (chronic steroid use).
Causes of Cushing's Disease
- Pituitary tumors producing excessive ACTH.
- Ectopic ACTH production, primarily from small cell lung cancers, pancreatic islet cell tumors, or renal cell carcinomas.
Diagnostic Workup for Cushing's
- Essential tests to screen for Cushing's include:
- Low-dose dexamethasone suppression test: Normal response suppresses ACTH and cortisol levels; those with Cushing's do not exhibit this response.
- 24-hour urinary cortisol test: Measures free cortisol levels, serving as another diagnostic marker.
Therapeutic Management Considerations
- Chronic steroid use may initially suppress ACTH production leading to adrenal atrophy and subsequent cortisol deficiency if steroids are abruptly discontinued.
- Understanding pathophysiology aids in identifying whether the issue stems from adrenal, pituitary, or ectopic sources of ACTH and cortisol production.
- Clinical management varies based on whether the cause is primary hypercortisolism (adrenal) or secondary (pituitary/ectopic).### Understanding Cushing's Syndrome and Cushing's Disease
- Collecting urine over 24 hours to measure cortisol levels in patients helps determine potential hypercortisolism
- Normal patients exhibit low cortisol levels in urine; high levels indicate possible Cushing's Syndrome or Cushing's Disease
- Elevated cortisol levels in urine may signal underlying adrenal cortex issues or pituitary tumors (Cushing's Disease)
Diagnostic Tests
- Salivary cortisol measurement at 11 PM can be an alternative to urine tests for cortisol levels
- High cortisol in saliva can indicate Cushing's Syndrome, indicating increased ACTH from either the pituitary gland or ectopic sites
- At least two positive tests (24-hour urine cortisol, elevated salivary cortisol, or lack of suppression with dexamethasone) suggest a diagnosis of Cushing's
Differentiating Causes of Cushing's
- Determine if hypercortisolism is caused by adrenal issues or pituitary tumors through ACTH level analysis
- Low ACTH indicates primary adrenal problem; high ACTH suggests secondary issues (pituitary or ectopic source)
Dexamethasone Suppression Test
- High-dose dexamethasone (8 mg) can help differentiate between pituitary tumors and ectopic ACTH sources
- In cases of pituitary tumors, high doses can suppress ACTH and cortisol, while ectopic sources remain unaffected
- ACTH suppression indicates a pituitary source; persistence of high levels points to ectopic tumors, typically small cell lung carcinoma
Corticotropin-Releasing Hormone (CRH) Test
- Administering CRH can help identify the source of ACTH production: pituitary tumors show a significant increase in ACTH, while ectopic sources show minimal response
- Post-CRH administration, a massive increase in cortisol correlates with a pituitary tumor diagnosis
Imaging and Further Evaluation
- If adrenal tumors (adenomas or carcinomas) are suspected, use CT or MRI for visual confirmation
- In cases of secondary hypercortisolism, if ACTH levels are high, perform further tests to indicate if it is due to a pituitary adenoma or ectopic production
- Screening should include scans of the chest, abdomen, and pelvis to identify common ectopic sources like small cell lung cancer
Treatment Approaches
- Pituitary tumors: surgical resection is the primary treatment
- Adrenal tumors: options include adrenalectomy or medications like Ketoconazole to suppress cortisol production
- Ectopic ACTH production: treatment may involve surgical resection, chemotherapy, or radiation therapy, with current cortisol suppression using Ketoconazole
- Chronic steroid use requires gradual tapering of steroid dosage
Conclusion
- The diagnostic approach for determining Cushing's Syndrome vs. Cushing's Disease revolves around a series of tests assessing cortisol and ACTH levels, followed by imaging as necessary for definitive diagnosis and treatment planning.
Cushing's Syndrome and Disease Overview
- Cushing's syndrome is characterized by excessive cortisol production, while Cushing's disease specifically involves elevated ACTH from the anterior pituitary gland.
- The hormonal pathway includes the hypothalamus releasing CRH, stimulating the anterior pituitary to produce ACTH, leading to cortisol production in the adrenal cortex.
Physiological Effects of High Cortisol
- High cortisol levels enhance sympathetic nervous system activity, increasing heart rate and stroke volume, contributing to elevated blood pressure.
- Activates alpha-1 adrenergic receptors, causing vasoconstriction and potentially leading to secondary hypertension resistant to standard treatments.
Immune System Impact
- Elevated cortisol suppresses neutrophil activity and T-cell proliferation, leading to increased risk of infections, particularly fungal infections.
Metabolic and Endocrine Consequences
- Cortisol promotes gluconeogenesis and glycogenolysis, resulting in hyperglycemia and potentially increased insulin resistance, heightening the risk of diabetes.
Lipid and Protein Metabolism Changes
- Induces lipolysis with fat redistribution from extremities to central body, causing features like moon facies, buffalo hump, and abdominal obesity.
- Muscle wasting (atrophy) predominantly affects proximal muscles and inhibits collagen synthesis, contributing to osteopenia and fracture risks.
Clinical Manifestations of Cushing's Syndrome
- Classic hallmark signs include:
- Refractory hypertension
- Increased susceptibility to infections
- Hyperglycemia and potential for diabetes
- Distinctive alterations in body fat distribution
- Muscle weakness and fragility leading to fractures.
Dermatological Effects
- Decreased collagen in the dermis results in thin skin, striae, ecchymosis, and impaired wound healing, increasing vulnerability to skin injuries.
- Symptoms include abdominal obesity, thin skin with striae or bruising, and potential muscle myopathy.
Endocrine and Reproductive Effects
- Elevated cortisol inhibits GnRH production, resulting in decreased FSH and LH levels which can affect reproductive health, leading to reduced libido in men and menstrual irregularities in women.
Differentiating Cushing's Disease from Syndrome
- Cushing's disease involves high ACTH levels generally caused by pituitary adenomas, potentially leading to excess androgens and hyperpigmentation.
- Cushing's syndrome manifests from high cortisol levels due to adrenal tumors or chronic steroid use.
Causes and Diagnostic Workup
- Causes of Cushing's disease include pituitary tumors and ectopic ACTH production primarily from certain cancers.
- Diagnostic tests encompass low-dose dexamethasone suppression tests and 24-hour urinary cortisol tests to assess cortisol levels.
Identifying Hypercortisolism Sources
- Salivary cortisol measurements can supplement urine tests; high levels indicate possible Cushing's syndrome.
- Differentiation of hypercortisolism source is achieved through ACTH level analysis — low indicating adrenal issues, high suggesting secondary causes.
Dexamethasone Suppression and CRH Tests
- High-dose dexamethasone can differentiate between pituitary tumors (suppressing ACTH) and ectopic sources (no suppression).
- CRH administration helps identify ACTH source; pituitary tumors show significant ACTH spikes compared to ectopic sources.
Imaging and Evaluation
- CT or MRI is essential for visual confirmation of suspected adrenal tumors, while further testing for high ACTH determines sources of secondary hypercortisolism.
- Screening scans should include chest, abdomen, and pelvis to identify ectopic ACTH-producing sites.
Treatment Strategies
- Surgical resection is the primary approach for pituitary tumors; adrenal tumors may require adrenalectomy or cortisol suppression medications like Ketoconazole.
- Ectopic ACTH production treatment could involve surgery, chemotherapy, or radiation therapy, with cortisol suppression also managed pharmacologically.
- Gradual tapering is essential for chronic steroid users to avoid adrenal insufficiency.
Summary
- Diagnosing Cushing's syndrome versus Cushing's disease involves a comprehensive series of tests for cortisol and ACTH levels, followed by imaging to confirm diagnosis and guide treatment planning.
Cushing's Syndrome and Disease Overview
- Cushing's syndrome is characterized by excessive cortisol production, while Cushing's disease specifically involves elevated ACTH from the anterior pituitary gland.
- The hormonal pathway includes the hypothalamus releasing CRH, stimulating the anterior pituitary to produce ACTH, leading to cortisol production in the adrenal cortex.
Physiological Effects of High Cortisol
- High cortisol levels enhance sympathetic nervous system activity, increasing heart rate and stroke volume, contributing to elevated blood pressure.
- Activates alpha-1 adrenergic receptors, causing vasoconstriction and potentially leading to secondary hypertension resistant to standard treatments.
Immune System Impact
- Elevated cortisol suppresses neutrophil activity and T-cell proliferation, leading to increased risk of infections, particularly fungal infections.
Metabolic and Endocrine Consequences
- Cortisol promotes gluconeogenesis and glycogenolysis, resulting in hyperglycemia and potentially increased insulin resistance, heightening the risk of diabetes.
Lipid and Protein Metabolism Changes
- Induces lipolysis with fat redistribution from extremities to central body, causing features like moon facies, buffalo hump, and abdominal obesity.
- Muscle wasting (atrophy) predominantly affects proximal muscles and inhibits collagen synthesis, contributing to osteopenia and fracture risks.
Clinical Manifestations of Cushing's Syndrome
- Classic hallmark signs include:
- Refractory hypertension
- Increased susceptibility to infections
- Hyperglycemia and potential for diabetes
- Distinctive alterations in body fat distribution
- Muscle weakness and fragility leading to fractures.
Dermatological Effects
- Decreased collagen in the dermis results in thin skin, striae, ecchymosis, and impaired wound healing, increasing vulnerability to skin injuries.
- Symptoms include abdominal obesity, thin skin with striae or bruising, and potential muscle myopathy.
Endocrine and Reproductive Effects
- Elevated cortisol inhibits GnRH production, resulting in decreased FSH and LH levels which can affect reproductive health, leading to reduced libido in men and menstrual irregularities in women.
Differentiating Cushing's Disease from Syndrome
- Cushing's disease involves high ACTH levels generally caused by pituitary adenomas, potentially leading to excess androgens and hyperpigmentation.
- Cushing's syndrome manifests from high cortisol levels due to adrenal tumors or chronic steroid use.
Causes and Diagnostic Workup
- Causes of Cushing's disease include pituitary tumors and ectopic ACTH production primarily from certain cancers.
- Diagnostic tests encompass low-dose dexamethasone suppression tests and 24-hour urinary cortisol tests to assess cortisol levels.
Identifying Hypercortisolism Sources
- Salivary cortisol measurements can supplement urine tests; high levels indicate possible Cushing's syndrome.
- Differentiation of hypercortisolism source is achieved through ACTH level analysis — low indicating adrenal issues, high suggesting secondary causes.
Dexamethasone Suppression and CRH Tests
- High-dose dexamethasone can differentiate between pituitary tumors (suppressing ACTH) and ectopic sources (no suppression).
- CRH administration helps identify ACTH source; pituitary tumors show significant ACTH spikes compared to ectopic sources.
Imaging and Evaluation
- CT or MRI is essential for visual confirmation of suspected adrenal tumors, while further testing for high ACTH determines sources of secondary hypercortisolism.
- Screening scans should include chest, abdomen, and pelvis to identify ectopic ACTH-producing sites.
Treatment Strategies
- Surgical resection is the primary approach for pituitary tumors; adrenal tumors may require adrenalectomy or cortisol suppression medications like Ketoconazole.
- Ectopic ACTH production treatment could involve surgery, chemotherapy, or radiation therapy, with cortisol suppression also managed pharmacologically.
- Gradual tapering is essential for chronic steroid users to avoid adrenal insufficiency.
Summary
- Diagnosing Cushing's syndrome versus Cushing's disease involves a comprehensive series of tests for cortisol and ACTH levels, followed by imaging to confirm diagnosis and guide treatment planning.
Cushing's Syndrome and Disease Overview
- Cushing's syndrome is characterized by excessive cortisol production, while Cushing's disease specifically involves elevated ACTH from the anterior pituitary gland.
- The hormonal pathway includes the hypothalamus releasing CRH, stimulating the anterior pituitary to produce ACTH, leading to cortisol production in the adrenal cortex.
Physiological Effects of High Cortisol
- High cortisol levels enhance sympathetic nervous system activity, increasing heart rate and stroke volume, contributing to elevated blood pressure.
- Activates alpha-1 adrenergic receptors, causing vasoconstriction and potentially leading to secondary hypertension resistant to standard treatments.
Immune System Impact
- Elevated cortisol suppresses neutrophil activity and T-cell proliferation, leading to increased risk of infections, particularly fungal infections.
Metabolic and Endocrine Consequences
- Cortisol promotes gluconeogenesis and glycogenolysis, resulting in hyperglycemia and potentially increased insulin resistance, heightening the risk of diabetes.
Lipid and Protein Metabolism Changes
- Induces lipolysis with fat redistribution from extremities to central body, causing features like moon facies, buffalo hump, and abdominal obesity.
- Muscle wasting (atrophy) predominantly affects proximal muscles and inhibits collagen synthesis, contributing to osteopenia and fracture risks.
Clinical Manifestations of Cushing's Syndrome
- Classic hallmark signs include:
- Refractory hypertension
- Increased susceptibility to infections
- Hyperglycemia and potential for diabetes
- Distinctive alterations in body fat distribution
- Muscle weakness and fragility leading to fractures.
Dermatological Effects
- Decreased collagen in the dermis results in thin skin, striae, ecchymosis, and impaired wound healing, increasing vulnerability to skin injuries.
- Symptoms include abdominal obesity, thin skin with striae or bruising, and potential muscle myopathy.
Endocrine and Reproductive Effects
- Elevated cortisol inhibits GnRH production, resulting in decreased FSH and LH levels which can affect reproductive health, leading to reduced libido in men and menstrual irregularities in women.
Differentiating Cushing's Disease from Syndrome
- Cushing's disease involves high ACTH levels generally caused by pituitary adenomas, potentially leading to excess androgens and hyperpigmentation.
- Cushing's syndrome manifests from high cortisol levels due to adrenal tumors or chronic steroid use.
Causes and Diagnostic Workup
- Causes of Cushing's disease include pituitary tumors and ectopic ACTH production primarily from certain cancers.
- Diagnostic tests encompass low-dose dexamethasone suppression tests and 24-hour urinary cortisol tests to assess cortisol levels.
Identifying Hypercortisolism Sources
- Salivary cortisol measurements can supplement urine tests; high levels indicate possible Cushing's syndrome.
- Differentiation of hypercortisolism source is achieved through ACTH level analysis — low indicating adrenal issues, high suggesting secondary causes.
Dexamethasone Suppression and CRH Tests
- High-dose dexamethasone can differentiate between pituitary tumors (suppressing ACTH) and ectopic sources (no suppression).
- CRH administration helps identify ACTH source; pituitary tumors show significant ACTH spikes compared to ectopic sources.
Imaging and Evaluation
- CT or MRI is essential for visual confirmation of suspected adrenal tumors, while further testing for high ACTH determines sources of secondary hypercortisolism.
- Screening scans should include chest, abdomen, and pelvis to identify ectopic ACTH-producing sites.
Treatment Strategies
- Surgical resection is the primary approach for pituitary tumors; adrenal tumors may require adrenalectomy or cortisol suppression medications like Ketoconazole.
- Ectopic ACTH production treatment could involve surgery, chemotherapy, or radiation therapy, with cortisol suppression also managed pharmacologically.
- Gradual tapering is essential for chronic steroid users to avoid adrenal insufficiency.
Summary
- Diagnosing Cushing's syndrome versus Cushing's disease involves a comprehensive series of tests for cortisol and ACTH levels, followed by imaging to confirm diagnosis and guide treatment planning.
Cushing's Syndrome and Disease Overview
- Cushing's syndrome is characterized by excessive cortisol production, while Cushing's disease specifically involves elevated ACTH from the anterior pituitary gland.
- The hormonal pathway includes the hypothalamus releasing CRH, stimulating the anterior pituitary to produce ACTH, leading to cortisol production in the adrenal cortex.
Physiological Effects of High Cortisol
- High cortisol levels enhance sympathetic nervous system activity, increasing heart rate and stroke volume, contributing to elevated blood pressure.
- Activates alpha-1 adrenergic receptors, causing vasoconstriction and potentially leading to secondary hypertension resistant to standard treatments.
Immune System Impact
- Elevated cortisol suppresses neutrophil activity and T-cell proliferation, leading to increased risk of infections, particularly fungal infections.
Metabolic and Endocrine Consequences
- Cortisol promotes gluconeogenesis and glycogenolysis, resulting in hyperglycemia and potentially increased insulin resistance, heightening the risk of diabetes.
Lipid and Protein Metabolism Changes
- Induces lipolysis with fat redistribution from extremities to central body, causing features like moon facies, buffalo hump, and abdominal obesity.
- Muscle wasting (atrophy) predominantly affects proximal muscles and inhibits collagen synthesis, contributing to osteopenia and fracture risks.
Clinical Manifestations of Cushing's Syndrome
- Classic hallmark signs include:
- Refractory hypertension
- Increased susceptibility to infections
- Hyperglycemia and potential for diabetes
- Distinctive alterations in body fat distribution
- Muscle weakness and fragility leading to fractures.
Dermatological Effects
- Decreased collagen in the dermis results in thin skin, striae, ecchymosis, and impaired wound healing, increasing vulnerability to skin injuries.
- Symptoms include abdominal obesity, thin skin with striae or bruising, and potential muscle myopathy.
Endocrine and Reproductive Effects
- Elevated cortisol inhibits GnRH production, resulting in decreased FSH and LH levels which can affect reproductive health, leading to reduced libido in men and menstrual irregularities in women.
Differentiating Cushing's Disease from Syndrome
- Cushing's disease involves high ACTH levels generally caused by pituitary adenomas, potentially leading to excess androgens and hyperpigmentation.
- Cushing's syndrome manifests from high cortisol levels due to adrenal tumors or chronic steroid use.
Causes and Diagnostic Workup
- Causes of Cushing's disease include pituitary tumors and ectopic ACTH production primarily from certain cancers.
- Diagnostic tests encompass low-dose dexamethasone suppression tests and 24-hour urinary cortisol tests to assess cortisol levels.
Identifying Hypercortisolism Sources
- Salivary cortisol measurements can supplement urine tests; high levels indicate possible Cushing's syndrome.
- Differentiation of hypercortisolism source is achieved through ACTH level analysis — low indicating adrenal issues, high suggesting secondary causes.
Dexamethasone Suppression and CRH Tests
- High-dose dexamethasone can differentiate between pituitary tumors (suppressing ACTH) and ectopic sources (no suppression).
- CRH administration helps identify ACTH source; pituitary tumors show significant ACTH spikes compared to ectopic sources.
Imaging and Evaluation
- CT or MRI is essential for visual confirmation of suspected adrenal tumors, while further testing for high ACTH determines sources of secondary hypercortisolism.
- Screening scans should include chest, abdomen, and pelvis to identify ectopic ACTH-producing sites.
Treatment Strategies
- Surgical resection is the primary approach for pituitary tumors; adrenal tumors may require adrenalectomy or cortisol suppression medications like Ketoconazole.
- Ectopic ACTH production treatment could involve surgery, chemotherapy, or radiation therapy, with cortisol suppression also managed pharmacologically.
- Gradual tapering is essential for chronic steroid users to avoid adrenal insufficiency.
Summary
- Diagnosing Cushing's syndrome versus Cushing's disease involves a comprehensive series of tests for cortisol and ACTH levels, followed by imaging to confirm diagnosis and guide treatment planning.
Cushing's Syndrome and Disease Overview
- Cushing's syndrome is characterized by excessive cortisol production, while Cushing's disease specifically involves elevated ACTH from the anterior pituitary gland.
- The hormonal pathway includes the hypothalamus releasing CRH, stimulating the anterior pituitary to produce ACTH, leading to cortisol production in the adrenal cortex.
Physiological Effects of High Cortisol
- High cortisol levels enhance sympathetic nervous system activity, increasing heart rate and stroke volume, contributing to elevated blood pressure.
- Activates alpha-1 adrenergic receptors, causing vasoconstriction and potentially leading to secondary hypertension resistant to standard treatments.
Immune System Impact
- Elevated cortisol suppresses neutrophil activity and T-cell proliferation, leading to increased risk of infections, particularly fungal infections.
Metabolic and Endocrine Consequences
- Cortisol promotes gluconeogenesis and glycogenolysis, resulting in hyperglycemia and potentially increased insulin resistance, heightening the risk of diabetes.
Lipid and Protein Metabolism Changes
- Induces lipolysis with fat redistribution from extremities to central body, causing features like moon facies, buffalo hump, and abdominal obesity.
- Muscle wasting (atrophy) predominantly affects proximal muscles and inhibits collagen synthesis, contributing to osteopenia and fracture risks.
Clinical Manifestations of Cushing's Syndrome
- Classic hallmark signs include:
- Refractory hypertension
- Increased susceptibility to infections
- Hyperglycemia and potential for diabetes
- Distinctive alterations in body fat distribution
- Muscle weakness and fragility leading to fractures.
Dermatological Effects
- Decreased collagen in the dermis results in thin skin, striae, ecchymosis, and impaired wound healing, increasing vulnerability to skin injuries.
- Symptoms include abdominal obesity, thin skin with striae or bruising, and potential muscle myopathy.
Endocrine and Reproductive Effects
- Elevated cortisol inhibits GnRH production, resulting in decreased FSH and LH levels which can affect reproductive health, leading to reduced libido in men and menstrual irregularities in women.
Differentiating Cushing's Disease from Syndrome
- Cushing's disease involves high ACTH levels generally caused by pituitary adenomas, potentially leading to excess androgens and hyperpigmentation.
- Cushing's syndrome manifests from high cortisol levels due to adrenal tumors or chronic steroid use.
Causes and Diagnostic Workup
- Causes of Cushing's disease include pituitary tumors and ectopic ACTH production primarily from certain cancers.
- Diagnostic tests encompass low-dose dexamethasone suppression tests and 24-hour urinary cortisol tests to assess cortisol levels.
Identifying Hypercortisolism Sources
- Salivary cortisol measurements can supplement urine tests; high levels indicate possible Cushing's syndrome.
- Differentiation of hypercortisolism source is achieved through ACTH level analysis — low indicating adrenal issues, high suggesting secondary causes.
Dexamethasone Suppression and CRH Tests
- High-dose dexamethasone can differentiate between pituitary tumors (suppressing ACTH) and ectopic sources (no suppression).
- CRH administration helps identify ACTH source; pituitary tumors show significant ACTH spikes compared to ectopic sources.
Imaging and Evaluation
- CT or MRI is essential for visual confirmation of suspected adrenal tumors, while further testing for high ACTH determines sources of secondary hypercortisolism.
- Screening scans should include chest, abdomen, and pelvis to identify ectopic ACTH-producing sites.
Treatment Strategies
- Surgical resection is the primary approach for pituitary tumors; adrenal tumors may require adrenalectomy or cortisol suppression medications like Ketoconazole.
- Ectopic ACTH production treatment could involve surgery, chemotherapy, or radiation therapy, with cortisol suppression also managed pharmacologically.
- Gradual tapering is essential for chronic steroid users to avoid adrenal insufficiency.
Summary
- Diagnosing Cushing's syndrome versus Cushing's disease involves a comprehensive series of tests for cortisol and ACTH levels, followed by imaging to confirm diagnosis and guide treatment planning.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.