Podcast
Questions and Answers
Which of the following complications of Crohn's disease directly impacts the digestive system?
Which of the following complications of Crohn's disease directly impacts the digestive system?
- Skin lesions
- Thromboembolism
- Strictures (correct)
- Ankylosing spondylitis
What is a potential consequence of Crohn's disease affecting the small intestine?
What is a potential consequence of Crohn's disease affecting the small intestine?
- Increased risk of kidney stones
- Decreased iron absorption (correct)
- Formation of gallstones
- Increased production of digestive enzymes
Which of these findings on a stool culture would support a diagnosis of Crohn's disease?
Which of these findings on a stool culture would support a diagnosis of Crohn's disease?
- Presence of normal bacteria
- Absence of parasites
- Presence of bacteria causing food poisoning
- Presence of blood and mucus (correct)
What imaging study can demonstrate an "apple core" appearance in the area of a stricture in a patient with Crohn's disease?
What imaging study can demonstrate an "apple core" appearance in the area of a stricture in a patient with Crohn's disease?
Which of the following is NOT a common symptom of Crohn's disease?
Which of the following is NOT a common symptom of Crohn's disease?
Which of the following blood test results would likely be elevated in a patient with Crohn's disease?
Which of the following blood test results would likely be elevated in a patient with Crohn's disease?
Which of the following complications of Crohn's disease is MOST likely to directly lead to anemia?
Which of the following complications of Crohn's disease is MOST likely to directly lead to anemia?
What is a potential consequence of Crohn's disease that could affect a patient's musculoskeletal system?
What is a potential consequence of Crohn's disease that could affect a patient's musculoskeletal system?
Which of the following clinical findings, besides symptoms like diarrhea and abdominal pain, would be MOST suggestive of Crohn's disease over other inflammatory bowel diseases?
Which of the following clinical findings, besides symptoms like diarrhea and abdominal pain, would be MOST suggestive of Crohn's disease over other inflammatory bowel diseases?
Which of the following diagnostic procedures should be avoided if bowel perforation is suspected in a patient with Crohn's disease?
Which of the following diagnostic procedures should be avoided if bowel perforation is suspected in a patient with Crohn's disease?
Which drug therapy approach involves utilizing less toxic medications initially and gradually escalating to stronger options as needed for treatment?
Which drug therapy approach involves utilizing less toxic medications initially and gradually escalating to stronger options as needed for treatment?
What is the primary mechanism of action for aminosalicylates in treating Crohn's disease?
What is the primary mechanism of action for aminosalicylates in treating Crohn's disease?
Which of these drugs is NOT categorized as an immunosuppressant used in Crohn's disease management?
Which of these drugs is NOT categorized as an immunosuppressant used in Crohn's disease management?
Which specific type of surgical intervention aims to widen narrowed areas of the bowel in Crohn's disease patients?
Which specific type of surgical intervention aims to widen narrowed areas of the bowel in Crohn's disease patients?
Which of the following is NOT a key focus of nutritional therapy in Crohn's disease management?
Which of the following is NOT a key focus of nutritional therapy in Crohn's disease management?
What dietary approach emphasizes the use of easily digestible nutrients and avoids fiber-rich foods in Crohn's disease?
What dietary approach emphasizes the use of easily digestible nutrients and avoids fiber-rich foods in Crohn's disease?
Which of the following is NOT a common nursing assessment component for Crohn's disease patients?
Which of the following is NOT a common nursing assessment component for Crohn's disease patients?
Which of these instructions is LEAST likely to be included in patient teaching for Crohn's disease management?
Which of these instructions is LEAST likely to be included in patient teaching for Crohn's disease management?
Which of the following statements is TRUE about ulcerative colitis?
Which of the following statements is TRUE about ulcerative colitis?
In the context of Crohn's disease, which of these medications is most effective in reducing inflammation?
In the context of Crohn's disease, which of these medications is most effective in reducing inflammation?
Which of the following is a defining characteristic of Crohn's disease, differentiating it from other inflammatory bowel conditions?
Which of the following is a defining characteristic of Crohn's disease, differentiating it from other inflammatory bowel conditions?
In the context of the etiology of Crohn's disease, which statement correctly identifies the known factors?
In the context of the etiology of Crohn's disease, which statement correctly identifies the known factors?
Which pathological feature is commonly observed in Crohn's disease that contributes to its complex presentation?
Which pathological feature is commonly observed in Crohn's disease that contributes to its complex presentation?
What is the most frequent location in the gastrointestinal tract where Crohn's disease manifests?
What is the most frequent location in the gastrointestinal tract where Crohn's disease manifests?
The 'cobblestone appearance' often found in Crohn's disease refers to which specific pathological change?
The 'cobblestone appearance' often found in Crohn's disease refers to which specific pathological change?
Besides the gastrointestinal tract, which complications of Crohn's disease can extend to other areas of the body?
Besides the gastrointestinal tract, which complications of Crohn's disease can extend to other areas of the body?
What best describes the clinical course of Crohn's disease?
What best describes the clinical course of Crohn's disease?
Which of the following best describes the impact of Crohn's disease on the bowel wall?
Which of the following best describes the impact of Crohn's disease on the bowel wall?
What is the expected output of an ileostomy patient in a 24-hour period?
What is the expected output of an ileostomy patient in a 24-hour period?
Which statement regarding self-care instructions for a patient with a new stoma indicates a misconception?
Which statement regarding self-care instructions for a patient with a new stoma indicates a misconception?
For patients recovering from inflammatory bowel disease, which menu choice reflects appropriate dietary modifications?
For patients recovering from inflammatory bowel disease, which menu choice reflects appropriate dietary modifications?
What potential complication should be monitored in a patient with a new colostomy?
What potential complication should be monitored in a patient with a new colostomy?
Which exercise is most beneficial for a patient to strengthen the pelvic floor muscles after ostomy surgery?
Which exercise is most beneficial for a patient to strengthen the pelvic floor muscles after ostomy surgery?
What is the primary symptom associated with ulcerative colitis?
What is the primary symptom associated with ulcerative colitis?
Which complication is associated with severe cases of ulcerative colitis?
Which complication is associated with severe cases of ulcerative colitis?
What surgery involves a total colectomy with rectal mucosal stripping and ileoanal reservoir?
What surgery involves a total colectomy with rectal mucosal stripping and ileoanal reservoir?
Which of the following describes the characteristics of moderate diarrhea in ulcerative colitis?
Which of the following describes the characteristics of moderate diarrhea in ulcerative colitis?
Which systemic symptom is a recognized consequence of ulcerative colitis?
Which systemic symptom is a recognized consequence of ulcerative colitis?
What is a potential complication of the total protocolectomy with continent ileostomy?
What is a potential complication of the total protocolectomy with continent ileostomy?
What is the maximum number of stools that can be experienced in severe ulcerative colitis?
What is the maximum number of stools that can be experienced in severe ulcerative colitis?
Which of the following is NOT a recognized extra-intestinal complication of ulcerative colitis?
Which of the following is NOT a recognized extra-intestinal complication of ulcerative colitis?
When does adaptation occur post-surgery in total colectomy with rectal mucosal stripping and ileoanal reservoir?
When does adaptation occur post-surgery in total colectomy with rectal mucosal stripping and ileoanal reservoir?
What is the main type of stool drainage following ileostomy?
What is the main type of stool drainage following ileostomy?
Flashcards
Crohn's Disease
Crohn's Disease
A chronic inflammatory bowel disease affecting any part of the GI tract with skip lesions.
Skip Lesions
Skip Lesions
Discontinuous areas of inflammation in Crohn's disease.
Peak Age of Onset
Peak Age of Onset
Crohn's disease typically begins in teens to mid-30s or after 60.
Genetic Predisposition
Genetic Predisposition
Signup and view all the flashcards
Chronic Disorder
Chronic Disorder
Signup and view all the flashcards
Cobblestone Appearance
Cobblestone Appearance
Signup and view all the flashcards
Ulcerations
Ulcerations
Signup and view all the flashcards
Fistulous Tracts
Fistulous Tracts
Signup and view all the flashcards
Symptoms of Crohn's Disease
Symptoms of Crohn's Disease
Signup and view all the flashcards
Complications of Crohn's Disease
Complications of Crohn's Disease
Signup and view all the flashcards
Nutritional problems in Crohn's
Nutritional problems in Crohn's
Signup and view all the flashcards
Diagnosis of Crohn's Disease
Diagnosis of Crohn's Disease
Signup and view all the flashcards
CBC in Crohn's Diagnosis
CBC in Crohn's Diagnosis
Signup and view all the flashcards
Stool cultures in Crohn's
Stool cultures in Crohn's
Signup and view all the flashcards
CT with contrast for Crohn's
CT with contrast for Crohn's
Signup and view all the flashcards
Barium Studies in Crohn's
Barium Studies in Crohn's
Signup and view all the flashcards
Extra-intestinal complications
Extra-intestinal complications
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Symptoms of Ulcerative Colitis
Symptoms of Ulcerative Colitis
Signup and view all the flashcards
Types of Diarrhea in UC
Types of Diarrhea in UC
Signup and view all the flashcards
Severe UC Symptoms
Severe UC Symptoms
Signup and view all the flashcards
Complications of UC
Complications of UC
Signup and view all the flashcards
Surgical Treatment - Total Colectomy
Surgical Treatment - Total Colectomy
Signup and view all the flashcards
Total Protocolectomy
Total Protocolectomy
Signup and view all the flashcards
Continent Ileostomy (Kock pouch)
Continent Ileostomy (Kock pouch)
Signup and view all the flashcards
Postoperative Care for Ileostomy
Postoperative Care for Ileostomy
Signup and view all the flashcards
Extra-intestinal Manifestations of UC
Extra-intestinal Manifestations of UC
Signup and view all the flashcards
Crohn’s Disease
Crohn’s Disease
Signup and view all the flashcards
Step-Up Approach
Step-Up Approach
Signup and view all the flashcards
Aminosalicylates
Aminosalicylates
Signup and view all the flashcards
Corticosteroids
Corticosteroids
Signup and view all the flashcards
Biologic Therapies
Biologic Therapies
Signup and view all the flashcards
Nutritional Therapy for Crohn's
Nutritional Therapy for Crohn's
Signup and view all the flashcards
Strictureplasty
Strictureplasty
Signup and view all the flashcards
Capsule Endoscopy
Capsule Endoscopy
Signup and view all the flashcards
Sulfasalazine
Sulfasalazine
Signup and view all the flashcards
Transient incontinence
Transient incontinence
Signup and view all the flashcards
Peristomal skin integrity
Peristomal skin integrity
Signup and view all the flashcards
Enterostomal therapy nurse
Enterostomal therapy nurse
Signup and view all the flashcards
Kegel exercises
Kegel exercises
Signup and view all the flashcards
Dietary modifications for colostomy
Dietary modifications for colostomy
Signup and view all the flashcards
Study Notes
Crohn's Disease/Ulcerative Colitis
- Inflammatory bowel diseases (IBDs) affecting the gastrointestinal tract
- Peak age of onset between teens and mid-30s, and a second peak around age 60
- Equally affects both sexes
- More common in individuals of Jewish and Middle European descent
- Chronic disorder with periods of exacerbations (attacks) and remissions (periods of reduced symptoms)
Crohn's Disease: Pathologic Characteristics
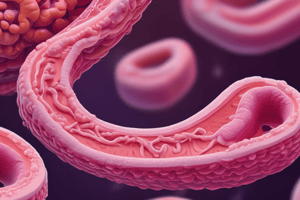
- A non-continuous inflammatory disease
- Can affect any point from the mouth to the anus
- Characterized by "skip lesions" (inflammation occurring in sections of the GI Tract but not uniformly)
- Affects the entire thickness of the bowel wall
- Cobblestone appearance of the colonic mucosa
- Granulomas and small bowel involvement are common features
Crohn's Disease: Etiology and Pathophysiology
- Ulcerations are deep and longitudinal (along the length of the bowel)
- Ulcers penetrate between islands of inflamed edematous mucosa
- This creates a classic cobblestone appearance
- Narrowing of the lumen with stricture development can occur
- Bowel obstruction is possible
Crohn's Disease: Etiology and Pathophysiology
- Microscopic leaks can allow bowel contents to spill into the peritoneal cavity, potentially leading to peritonitis
- Abscesses or fistulas (abnormal passages) that connect with other loops of bowel, skin, bladder, rectum, or vagina can form
Crohn's Disease: Clinical Manifestations
- A chronic disorder with mild to severe exacerbations occurring unpredictably over years
- Diarrhea and cramp-like abdominal pain are common complaints
- Other symptoms can include bloody stool, fever, fatigue, weight loss and rectal bleeding
Crohn's Disease: Complications
- Intestinal: Fistulas, strictures, anal abscesses, perforation, recurrence after surgery, common at anastomoses (connection points in the GI Tract)
- Extra-intestinal: Thromboembolism, arthritis, ankylosing spondylitis, eye inflammation, kidney stones, gallstones, and skin lesions
Crohn's Disease: Complications
- Nutritional problems are common due to small intestine involvement.
- Common problems include fat malabsorption, anemia, electrolyte disturbances, and dehydration
Crohn's Disease: Diagnostic Studies
- History, physical examination, and blood tests (CBC, serum electrolyte levels, serum protein levels)
- Stool cultures, stool tests, colonoscopy, flexible sigmoidoscopy, upper endoscopy, capsule endoscopy
- CT scans and barium studies to visualize inflammation, abscess, strictures, and fistula formation
Crohn's Disease: Collaborative Care - Drug Therapy
- Step-up approach using less-toxic medications initially (aminosalicylates)
- Step-down approach incorporating biologic (immunologic) and targeted therapies
- Corticosteroids, immunosuppressants (azathioprine, 6-MP, MTX), and 5-aminosalicylates/sulfasalazine (e.g., azulfidine)
- Antimicrobials are also used (e.g., metronidazole, ciprofloxacin)
- Methylprednisone and budesonide (Entocort) are also commonly used
Crohn's Disease: Collaborative Care - Immunosuppressants and Biologics
- Immunosuppressants (with regular CBC monitoring) including methotrexate, and sometimes anti-TNF agents
- Regular follow up needed for CBC monitoring in immunosuppressed patients.
Crohn's Disease: Collaborative Care - Surgical Interventions
- Strictureplasty procedures are used to widen areas of narrowed bowel
- Complete bowel resection is required in severe cases
- Other surgeries include procedures to correct complications (fistulas, abscesses, perforations) and anastomoses
Crohn's Disease: Collaborative Care - Nutritional Therapy
- Dietary consultation plays a key role in correcting and preventing malnutrition
- Replacing fluid and electrolytes, preventing weight loss, and correcting high-calorie, high-protein diets are important
- Avoiding low-residue foods is essential for many patients
Crohn's Disease: Nursing Management
- Assessing pain, autoimmune disorders, infection, fluid/electrolyte balance and presence of blood in diarrhea
- Examining weight loss, anxiety, depression, use of prescribed medications, family history, and coping strategies
- Teaching the patient about rest, diet, and perianal care, recognizing symptoms of recurrence, and knowing when to seek medical care
Ulcerative Colitis: Clinical Manifestations
- A chronic inflammatory disease of the large intestine
- Typically involves the rectum and colon, with inflammation spreading into adjacent tissue
- Ulcerations, fistulas, and abscess formation can occur
- Bloody diarrhea with mucous is the primary symptom, frequently associated with abdominal pain, fatigue, and weight loss.
Ulcerative Colitis: Complications
- Intestinal: Strictures, perforations, hemorrhage, toxic megacolon, carcinoma, and Clostridium difficile infection
- Extra-intestinal: Thromboembolism, arthritis, ankylosing spondylitis, eye inflammation, kidney stones, gallstones, skin lesions
Ulcerative Colitis: Collaborative Care - Surgical Interventions
- Total colectomy with rectal mucosal stripping and ileoanal reservoir or pouch are procedures for treatment of ulcerative colitis
- Other procedures might include total protocolectomy with a continent ileostomy
Ulcerative Colitis and Crohn Disease - Nutritional Therapy and Discharge Instructions
- Provide information to patients about dietary modifications to reduce symptoms
- Instructions on stoma care, including changing appliances, monitoring skin, and cleaning techniques.
Student Response Questions
- Includes diet recommendations after colostomy surgery: fruits, vegetables, whole-grain breads, and poached eggs with rice.
- Also includes assessment of patient knowledge regarding disease recurrence.
- Also includes assessment of patient knowledge regarding stoma care.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.