Podcast
Questions and Answers
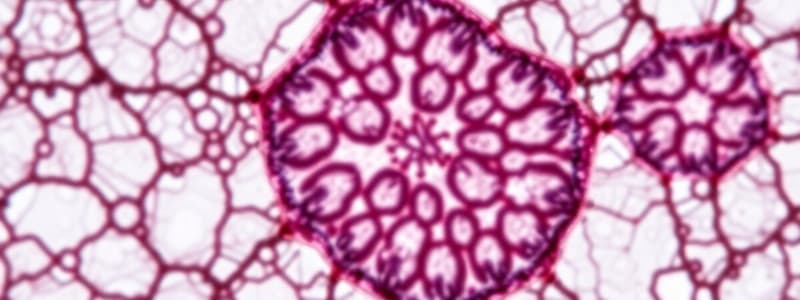
A connective tissue sample shows cells with eccentric, indented nuclei and cytoplasm filled with lysosomes. What is the primary function of these cells?
A connective tissue sample shows cells with eccentric, indented nuclei and cytoplasm filled with lysosomes. What is the primary function of these cells?
- Formation of circulating antibodies.
- Secretion of heparin and histamine.
- Synthesis of collagen fibers.
- Phagocytosis of foreign materials. (correct)
Which component of ground substance in connective tissue is responsible for attaching cells to fibers?
Which component of ground substance in connective tissue is responsible for attaching cells to fibers?
- Chondroitin sulfate
- Glycoprotein (correct)
- Hyaluronic acid
- Sulphated acid mucopolysaccharides
A tissue sample stained with Toluidine blue shows cells with granules that stain purple to red. Which of the following is the most likely function of these cells?
A tissue sample stained with Toluidine blue shows cells with granules that stain purple to red. Which of the following is the most likely function of these cells?
- Transporting oxygen in the blood.
- Secreting heparin and histamine. (correct)
- Phagocytosing bacteria and cellular debris.
- Producing collagen and elastic fibers.
Which of the following is an example of specialized connective tissue?
Which of the following is an example of specialized connective tissue?
Plasma cells are responsible for producing antibodies. Which morphological feature is associated with antibody production?
Plasma cells are responsible for producing antibodies. Which morphological feature is associated with antibody production?
Which characteristic is NOT typically associated with epithelial tissue?
Which characteristic is NOT typically associated with epithelial tissue?
The basement membrane's primary function in relation to epithelial tissue is to:
The basement membrane's primary function in relation to epithelial tissue is to:
In which of the following locations would you most likely find simple squamous epithelium?
In which of the following locations would you most likely find simple squamous epithelium?
Where is simple cuboidal epithelium typically located?
Where is simple cuboidal epithelium typically located?
The primary function of simple columnar epithelium, found in the lining of the intestines, is:
The primary function of simple columnar epithelium, found in the lining of the intestines, is:
What is a key characteristic of pseudostratified columnar epithelium that distinguishes it from other types?
What is a key characteristic of pseudostratified columnar epithelium that distinguishes it from other types?
Stratified squamous epithelium is well-suited for:
Stratified squamous epithelium is well-suited for:
The unique characteristic of transitional epithelium that makes it suitable for lining the urinary bladder is its:
The unique characteristic of transitional epithelium that makes it suitable for lining the urinary bladder is its:
Which of the following is a characteristic of the superficial cells in relaxed epithelium?
Which of the following is a characteristic of the superficial cells in relaxed epithelium?
What is the primary difference between endocrine and exocrine glands?
What is the primary difference between endocrine and exocrine glands?
Which type of exocrine gland secretion involves the loss of the apical part of the cell?
Which type of exocrine gland secretion involves the loss of the apical part of the cell?
Which of the following describes the method of secretion in merocrine glands?
Which of the following describes the method of secretion in merocrine glands?
Which of the following cell types is NOT a component of sensory epithelium?
Which of the following cell types is NOT a component of sensory epithelium?
What is the primary function of connective tissue?
What is the primary function of connective tissue?
Which property of collagen fibers allows them to be easily viewed using H&E stain?
Which property of collagen fibers allows them to be easily viewed using H&E stain?
What protein primarily composes elastic fibers?
What protein primarily composes elastic fibers?
Which staining technique is most effective for visualizing reticular fibers in connective tissue?
Which staining technique is most effective for visualizing reticular fibers in connective tissue?
What is the primary function of reticular fibers within an organ?
What is the primary function of reticular fibers within an organ?
How do fibroblasts contribute to wound repair in connective tissue?
How do fibroblasts contribute to wound repair in connective tissue?
What distinguishes plasma cells from other connective tissue cells regarding their origin?
What distinguishes plasma cells from other connective tissue cells regarding their origin?
Which of the following is a characteristic feature of plasma cells when observed under a light microscope?
Which of the following is a characteristic feature of plasma cells when observed under a light microscope?
What cellular structures are abundant within fibroblasts, reflecting their primary function?
What cellular structures are abundant within fibroblasts, reflecting their primary function?
What is the primary role of fibroblasts in connective tissue?
What is the primary role of fibroblasts in connective tissue?
Which component of the extracellular matrix is secreted by fibroblasts and provides elasticity to tissues?
Which component of the extracellular matrix is secreted by fibroblasts and provides elasticity to tissues?
Flashcards
Epithelium
Epithelium
Tissue type that covers surfaces and lines cavities; forms glands and sensory receptors.
Basement Membrane
Basement Membrane
Layer separating epithelium from underlying connective tissue, made of glycoproteins and reticular fibers.
Simple Squamous Epithelium
Simple Squamous Epithelium
Single layer of flat cells; found lining blood vessels and body cavities.
Simple Cuboidal Epithelium
Simple Cuboidal Epithelium
Signup and view all the flashcards
Simple Columnar Epithelium
Simple Columnar Epithelium
Signup and view all the flashcards
Pseudostratified Columnar Epithelium
Pseudostratified Columnar Epithelium
Signup and view all the flashcards
Stratified Squamous Epithelium
Stratified Squamous Epithelium
Signup and view all the flashcards
Transitional Epithelium
Transitional Epithelium
Signup and view all the flashcards
Exocrine Glands
Exocrine Glands
Signup and view all the flashcards
Endocrine Glands
Endocrine Glands
Signup and view all the flashcards
Serous Glands
Serous Glands
Signup and view all the flashcards
Mucous Glands
Mucous Glands
Signup and view all the flashcards
Muco-serous Glands
Muco-serous Glands
Signup and view all the flashcards
Merocrine Glands
Merocrine Glands
Signup and view all the flashcards
Apocrine Glands
Apocrine Glands
Signup and view all the flashcards
Holocrine Glands
Holocrine Glands
Signup and view all the flashcards
Mast cell function
Mast cell function
Signup and view all the flashcards
Macrophage function:
Macrophage function:
Signup and view all the flashcards
Ground substance function
Ground substance function
Signup and view all the flashcards
Plasma cell function
Plasma cell function
Signup and view all the flashcards
Ground substance main components
Ground substance main components
Signup and view all the flashcards
Reticular Fibers
Reticular Fibers
Signup and view all the flashcards
Fixed Connective Tissue Cells
Fixed Connective Tissue Cells
Signup and view all the flashcards
Free (Wandering) Cells
Free (Wandering) Cells
Signup and view all the flashcards
Fibroblast
Fibroblast
Signup and view all the flashcards
Active Fibroblast
Active Fibroblast
Signup and view all the flashcards
Fibroblast Function
Fibroblast Function
Signup and view all the flashcards
Plasma Cell
Plasma Cell
Signup and view all the flashcards
Negative Golgi Area
Negative Golgi Area
Signup and view all the flashcards
Study Notes
Epithelial Tissue: General Characteristics
- Epithelial tissue is composed of densely packed cells with minimal intercellular substance.
- It rests on a basement membrane and the underlying connective tissue.
- Epithelium is avascular, meaning it lacks blood vessels.
- It is rich in nerve endings.
- Epithelium has a high capacity for regeneration.
- Forms sheets that cover surfaces and line all cavities in the body, known as covering and lining epithelium.
- Also forms clusters of cells that form glands. This is called glandular epithelium.
- Modified structures that act as sensory receptors are sensory epithelium.
Basement Membrane
- The basement membrane separates the epithelium from the underlying connective tissue.
- Appears as a thin layer when viewed with a light microscope (LM) and can be stained with PAS and silver.
- Under an electron microscope (EM), the basement membrane is composed of:
- A cell coat of epithelial cells.
- A basal lamina: a homogenous layer consisting of glycoproteins.
- A layer of reticular fibres.
- The function of the basement membrane includes:
- acting as a barrier against diffusion of macromolecules
- providing support for the epithelial layer.
Covering & Lining Epithelium: Simple Epithelium
- Simple squamous epithelium consists of a single layer of flat cells with flat nuclei.
- It is found lining blood vessels and body cavities.
- Simple cuboidal epithelium consists of a single layer of cubical cells with central rounded nuclei.
- It lines renal tubules and thyroid follicles.
- Simple columnar epithelium consists of one layer of tall cells with oval basal nuclei.
- It lines the stomach, intestines, and gallbladder.
- Pseudostratified columnar epithelium is composed of one layer of cells, where some cells are tall and reach the surface, while others are shorter and do not reach the surface, but all rest on the basement membrane.
- It appears falsely stratified.
- It lines the trachea as pseudostratified columnar ciliated epithelium.
Stratified Epithelium
- Stratified squamous epithelium has several layers of cells.
- Its basal cells being columnar, the following layers polyhedral, and the superficial cells flattened squamous.
- Stratified squamous epithelium has two types:
- Non-keratinized, lining the oral cavity and oesophagus.
- Keratinized, covers the skin.
- Transitional epithelium can change its form.
- It lines organs that can expand significantly, such as the urinary bladder.
- When stretched (as in a full bladder), it resembles stratified squamous non-keratinized epithelium. When relaxed (as in an empty bladder):
- The basal cells are short columnar
- Intermediate cells are polyhedral
- Superficial cells are large, rounded with convex upper surfaces and contain one or two nuclei.
Glandular Epithelium: Classification
- Ways of classifying glandular epithelium:
- Presence or absence of ducts:
- Exocrine glands: possess ducts that carry their secretion to the surface of the epithelium
- Endocrine glands: are ductless and secrete hormones directly into the blood.
- Presence or absence of ducts:
Exocrine Glands
- Further classified according to the nature of secretion into:
- Serous glands: secrete watery secretion rich in enzymes.
- Mucous glands secrete viscid mucous secretion.
- Muco-serous glands secrete both mucous and serous secretion.
- Classified by the mode of secretion:
- Merocrine glands: secrete via exocytosis, leaving the cell membrane intact and with no part of the cell being lost.
- Apocrine glands: secretion involves the loss of the apical part of the cell.
- Holocrine glands: cells accumulate secretion, then burst and are totally included in the secretion.
Sensory Epithelium (Neuro-Epithelium)
- Epithelial tissue modified to act as a receptor.
- Consists of three types of cells: sensory cells, supporting cells, and basal cells.
- Found in taste buds in the tongue and olfactory epithelium in the nose.
Connective Tissue: Components and Functions
- Connective tissue is a basic tissue comprising of 3 components:
- Connective tissue cells, connective tissue fibres, ground substance and tissue fluid
- Functions:
- Connects and holds other tissues together.
- Nutrients are transported from capillaries to the cells of other tissues.
- Mechanism for defence and immunity.
Connective Tissue Fibres
- Types: collagenic, elastic, and reticular fibres.
- Collagen (white) fibres:
- Composed of the protein collagen
- Colourless elongated/wavy bundles
- They are non-branching, small fibrils.
- Collagenic fibres are acidophilic, thus staining pink with H&E stain
- Provide strength to the tissue
- Elastic (yellow) fibres:
- Composed of the protein elastin
- Long, thin, branched fibres form irregular networks.
- Elastic fibres are weakly acidophilic with Hx&E stain
- Take a dark brown colour with orcein stain
- Provide elasticity and strength to the tissue
- Reticular fibres:
- Fine fibres arranged in networks.
- Mainly formed of the protein collagen with carbohydrate.
- Not visible in H&E preparations, but with silver stains, they take a black colour.
- Provide the framework of the organs.
Connective Tissue Cells
- Fixed cells:
- Stable, long-lived cells.
- Include fibroblasts, fat (adipose) cells, and mesenchymal cells.
- Free (wandering) cells:
- Short-lived, changing population.
- Includes mast cells, plasma cells, macrophages, and leukocytes.
- Fibroblast:
- The most common cell in connective tissue proper.
- Originates from mesenchymal cells dividing and differentiating into active young fibroblasts and older fibroblasts are called fibrocytes
- Active young cells have an oval pale nucleus with a prominent nucleolus and abundant basophilic cytoplasm.
- Contains numerous rough endoplasmic reticulum, well-developed Golgi stacks, and transfer vesicles.
- Functions include formation of both components of the intercellular substance, secretion of mucopolysaccharide (GAG) of the matrix, secretion of tropocollagen to form collagenic fibers, secretion of elastin to give elastic fibers, and repair of wounds.
- Plasma cells:
- Origin: from B – lymphocytes that enter the loose connective tissue from the blood stream, and are not developed from mesenchymal cells.
- Spherical or ovoid cells with an eccentric nucleus which has coarse heterochromatin (clock – face chromatin).
- The cytoplasm is intensely basophilic except near the nucleus, where it is pale (negative Golgi area).
- EM: numerous RER and free ribosomes, Golgi located near the nucleus, and secretory vesicles containing immunoglobulin. The cytoplasm contains rounded acidophilic Russell bodies.
- Function: the formation of antibodies that circulate into the blood (humoral antibodies).
- Mast cells are rounded/spindle shaped with a rounded central nucleus.
- The cytoplasm is studded with basophilic granules that stain metachromatically (purple to red) with Toluidine blue.
- Function: secretion of heparin and histamine.
- Macrophages (histiocytes): derived from mesenchymal cells in prenatal life and from monocytes in postnatal life.
- Oval shaped with eccentric condensed indented nucleus
- The cytoplasm contains lysosomes.
- Function: phagocytosis of foreign materials.
Ground Substances of Connective Tissue
- Composed of hyaluronic acid (a non-sulphated acid mucopolysaccharide glucosaminoglycan, GAG).
- Sulphated acid mucopolysaccharids and Glycoprotein, functions in attaching cells to fibres.
- Function: transport of nutrients and oxygen from capillaries to other tissues.
Classification of Connective Tissues
- Types of connective tissues:
- Connective tissue proper:
- Loose connective tissue
- Dense white fibrous connective tissue
- Dense elastic connective tissue
- Reticular tissue
- Adipose tissue
- Mucous (embryonic) connective tissue
- Specialized connective tissue:
- Cartilage
- Bone
- Blood
- Connective tissue proper:
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.