Podcast
Questions and Answers
What is the primary goal of imaging in a patient with acute stroke?
What is the primary goal of imaging in a patient with acute stroke?
- Assess the level of consciousness
- Evaluate the duration of symptoms
- Differentiate between hemorrhage and ischemia (correct)
- Identify the exact location of the brain tumor
Which of the following is an early CT sign of ischemia?
Which of the following is an early CT sign of ischemia?
- Obscuration of the lentiform nucleus (correct)
- Bilateral cortical atrophy
- Increased density of brain tissue
- Thickening of the cranial bones
What does the Insular Ribbon sign indicate on a CT scan?
What does the Insular Ribbon sign indicate on a CT scan?
- Presence of a brain tumor
- Early infarction in the MCA territory (correct)
- Cortical necrosis
- Hemorrhagic transformation
Why do we observe ischemia on a CT scan?
Why do we observe ischemia on a CT scan?
What does the Dense MCA sign suggest in a CT angiography?
What does the Dense MCA sign suggest in a CT angiography?
What percentage of MCA infarcts are initially hemorrhagic?
What percentage of MCA infarcts are initially hemorrhagic?
What correlates with the decrease in CT attenuation when brain water content increases?
What correlates with the decrease in CT attenuation when brain water content increases?
What can be seen as a result of inadequate ATP supply in the brain?
What can be seen as a result of inadequate ATP supply in the brain?
What is the most common cause of traumatic intracranial hemorrhage?
What is the most common cause of traumatic intracranial hemorrhage?
Which type of intracranial hemorrhage occurs most commonly from rupture of an aneurysm?
Which type of intracranial hemorrhage occurs most commonly from rupture of an aneurysm?
What is a primary complication of traumatic intracranial hemorrhage?
What is a primary complication of traumatic intracranial hemorrhage?
What anatomical structure separates the dura mater from the skull?
What anatomical structure separates the dura mater from the skull?
Which layer of the meninges allows blood vessels to nourish the brain?
Which layer of the meninges allows blood vessels to nourish the brain?
In patients on anticoagulant therapy, which type of hematoma is most likely to occur?
In patients on anticoagulant therapy, which type of hematoma is most likely to occur?
What type of injury is characterized by diffuse axonal injury (DAI)?
What type of injury is characterized by diffuse axonal injury (DAI)?
Which of the following describes an epidural hematoma?
Which of the following describes an epidural hematoma?
What is the primary cause of an epidural hematoma?
What is the primary cause of an epidural hematoma?
How does a subdural hematoma typically present in terms of location?
How does a subdural hematoma typically present in terms of location?
Which population is most commonly associated with subdural hematomas?
Which population is most commonly associated with subdural hematomas?
What differentiates an acute subdural hematoma's appearance from a chronic one?
What differentiates an acute subdural hematoma's appearance from a chronic one?
In which scenario is a subdural hematoma most likely to be detected as isodense?
In which scenario is a subdural hematoma most likely to be detected as isodense?
What characteristic is common to both hyperacute and rebleeding subdural hematomas?
What characteristic is common to both hyperacute and rebleeding subdural hematomas?
Why is an epidural hematoma more likely to cross the midline than a subdural hematoma?
Why is an epidural hematoma more likely to cross the midline than a subdural hematoma?
What is a typical sign of active bleeding in an acute subdural hematoma?
What is a typical sign of active bleeding in an acute subdural hematoma?
Flashcards
What is the goal of imaging in acute stroke?
What is the goal of imaging in acute stroke?
The goal of imaging in a patient with acute stroke is to identify the cause of the stroke, determine the extent of brain damage, and assess the risk of further damage. This allows for appropriate medical management.
What does hypodense brain tissue on a CT scan suggest?
What does hypodense brain tissue on a CT scan suggest?
Hypodense brain tissue on a CT scan can indicate ischemia, which is a lack of blood flow to the brain. It typically occurs in the territory of the middle cerebral artery (MCA) and involves both gray and white matter.
What is the significance of an obscured lentiform nucleus on a CT scan?
What is the significance of an obscured lentiform nucleus on a CT scan?
The lentiform nucleus is a part of the basal ganglia, a critical area for movement control. Obscuration, or blurring of the lentiform nucleus, is a major sign of stroke in the middle cerebral artery territory, as this area is almost always affected.
What is the insular ribbon sign and why is it important in stroke imaging?
What is the insular ribbon sign and why is it important in stroke imaging?
Signup and view all the flashcards
What is the 'dense MCA sign' and what does it tell us?
What is the 'dense MCA sign' and what does it tell us?
Signup and view all the flashcards
What are hemorrhagic infarcts and how are they viewed?
What are hemorrhagic infarcts and how are they viewed?
Signup and view all the flashcards
What is the significance of the middle cerebral artery (MCA) in stroke imaging?
What is the significance of the middle cerebral artery (MCA) in stroke imaging?
Signup and view all the flashcards
What is ATP and what role does it play in stroke?
What is ATP and what role does it play in stroke?
Signup and view all the flashcards
Traumatic Intracranial Hemorrhage
Traumatic Intracranial Hemorrhage
Signup and view all the flashcards
Subarachnoid Hemorrhage
Subarachnoid Hemorrhage
Signup and view all the flashcards
Subdural Hematoma
Subdural Hematoma
Signup and view all the flashcards
Epidural Hematoma
Epidural Hematoma
Signup and view all the flashcards
Intracerebral Hemorrhage
Intracerebral Hemorrhage
Signup and view all the flashcards
Diffuse Axonal Injury (DAI)
Diffuse Axonal Injury (DAI)
Signup and view all the flashcards
Dura Mater
Dura Mater
Signup and view all the flashcards
Pia Mater
Pia Mater
Signup and view all the flashcards
Subdural Hematoma Spread
Subdural Hematoma Spread
Signup and view all the flashcards
Heterogeneous Subdural Hematoma
Heterogeneous Subdural Hematoma
Signup and view all the flashcards
Isodense Subdural Hematoma
Isodense Subdural Hematoma
Signup and view all the flashcards
Midline Shift in Subdural Hematoma
Midline Shift in Subdural Hematoma
Signup and view all the flashcards
Density of Subdural Hematomas Over Time
Density of Subdural Hematomas Over Time
Signup and view all the flashcards
Density Variability in Subdural Hematoma
Density Variability in Subdural Hematoma
Signup and view all the flashcards
Study Notes
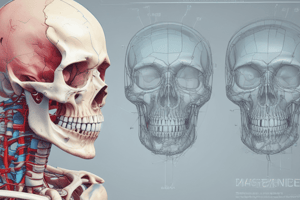
Computed Tomography (CT) Head Scan
- Prepared by Ahmed Jasem Abass, MSC Medical
Imaging in Acute Stroke
- Goal of imaging in acute stroke is to exclude hemorrhage
- Differentiate between irreversibly affected brain tissue and reversibly impaired tissue
- Identify stenosis or occlusion of major intracranial arteries
CT Early Signs of Ischemia
- Hypo-attenuating brain tissue
- Obscuration of the lentiform nucleus
- Insular Ribbon sign
- Dense MCA sign
- Hemorrhagic infarcts
Hypo Attenuating Brain Tissue
- Ischemia causes cytotoxic edema due to ion pump failure, requiring ATP
- 1% increase in brain water content results in a 2.5 HU decrease in CT attenuation
- Diagnosis of infarction is based on MCA location and involvement of gray and white matter
Obscuration of the Lentiform Nucleus
- Blurred basal ganglia, an important sign of infarction
- Seen in middle cerebral artery (MCA) infarction
- One of the earliest and most frequent signs
Insular Ribbon Sign
- Refers to hypodensity and swelling of the insular cortex
- A subtle early CT sign of infarction in the middle cerebral artery territory
- Sensitive to ischemia due to being furthest from collateral flow
- Differentiate from herpes encephalitis
Dense MCA Sign
- Result of thrombus or embolus in the MCA
- Visible on CT angiography as MCA occlusion
Hemorrhagic Infarcts
- 15% of MCA infarcts are initially hemorrhagic
- Hemorrhage easily detected with CT, also visualized with gradient echo MR sequences
Traumatic Intracranial Hemorrhage
- Any bleeding inside the skull or brain is a medical emergency
- Common causes include stroke, trauma, and ruptured aneurysms
- Complications include increased intracerebral pressure, edema, and hydrocephalus
Localization of Hemorrhage
- Subarachnoid Hemorrhage: Acute bleeding under the arachnoid membrane, often due to aneurysm rupture
- Subdural Hematoma: Bleeding between the dura and arachnoid membranes, usually from bridging vein rupture, common in elderly and patients on anticoagulants
- Epidural Hematoma: Bleeding between the dura and skull, often due to temporal bone fracture and middle meningeal artery rupture
- Intra-axial Hemorrhage (Intracerebral): Cerebral hemorrhagic contusion, post-traumatic small hemorrhages located near the skull, often frontobasal and anterior in temporal lobes
- Diffuse Axonal Injury (DAI): Diffuse injury at the gray-white matter junction, seen in high-velocity injuries and low sensitivity for CT, better seen on MRI.
Anatomy of the Meninges
- Meninges are three membranes (dura, arachnoid, and pia) enveloping brain and spinal cord
- Cerebrospinal fluid (CSF) is found in the subarachnoid space between arachnoid and pia
- Dura mater is the outermost meningeal layer, with two layers (inner and outer)
- Arachnoid mater is the delicate layer with fibers extending to pia
- Pia mater is the innermost layer, allowing nutrient blood vessels to pass through the brain
Traumatic Hemorrhage (Epidural Hematoma)
- Bleeding between dura and skull
- Common in children with head injury and temporal bone fractures, leading to tearing of the middle meningeal artery
- Usually does not cross suture lines.
Subdural Hematoma
- Collection of blood between inner dura and arachnoid membranes
- Cannot cross the midline
- Usually due to cortical bridging vein rupture, especially in elderly and alcoholics with atrophy
- Venous structures are less packed, increasing space for rupture.
Subdural Hematoma (CT Findings)
- Acute: High-density, hyperdense
- Chronic: Low-density, hypodensity.
- Midline shift seen on CT (left image example given)
The Images Show a Subdural Hematoma
- Hematoma displays both hyperdense and isodense areas (indicative of both acute and chronic bleeding).
- Displacement of midline structures and CSF flow obstruction (dilated temporal horn of the right lateral ventricle).
- Acute: Hyperdense (clotted blood); Subacute: Isodense; Chronic: Hypodense (relative to brain parenchyma)
- Heterogeneous appearance in acute setting due to combination of both fresh and clotted blood.
Isodense Subdural Hematoma
- Aging hematomas decrease in density, matching that of the brain, making them harder to detect on CT.
- Can be bilateral.
- Rare case appearance: isodense to brain tissue; e.g., in patients with severe anemia, disseminated intravascular coagulation, or dilution with CSF.
Chronic Subdural Hematoma
- Appears hypodensity to parenchyma and isodensity to CSF after 21 days
- Can mimic a hygroma
- Hygroma is due to traumatic tear in the arachnoid layer that causes CSF leak into the subdural space
Subarachnoid Hemorrhage
- Hyperdense blood in the subarachnoid space (Sylvian fissure).
- Can have subgaleal hemorrhage in the occipital region.
- Often due to coupe contrecoup type injuries (double impact trauma)
Coupe Contrecoup Type of Injury
- Characterized by contusional hemorrhages, subdural hematoma, and subarachnoid hemorrhage on opposite side of the impact site.
- Often associated with parietal bone fracture and subarachnoid hemorrhage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.