Podcast
Questions and Answers
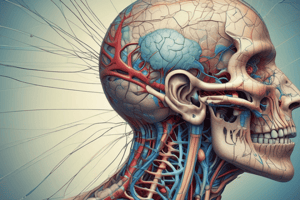
Why is understanding the anatomy, origin, and pathway of cranial nerves essential in clinical settings?
Why is understanding the anatomy, origin, and pathway of cranial nerves essential in clinical settings?
- It aids in interpreting neurological signs and identifying causes of dysfunction. (correct)
- It is crucial for understanding the emotional responses of patients.
- It simplifies the process of prescribing medications.
- It helps in selecting the appropriate surgical instruments.
A patient presents with symptoms suggesting cranial nerve dysfunction. Which of the following conditions is LEAST likely to be considered as a potential cause?
A patient presents with symptoms suggesting cranial nerve dysfunction. Which of the following conditions is LEAST likely to be considered as a potential cause?
- Congenital abnormalities
- Traumatic brain injury
- An acute viral infection (correct)
- Diabetic neuropathy
A lesion affecting the superior orbital fissure would MOST likely impact which combination of cranial nerves?
A lesion affecting the superior orbital fissure would MOST likely impact which combination of cranial nerves?
- Optic, Olfactory and Trigeminal (V1)
- Oculomotor, Trochlear, Abducens, and Trigeminal (V1) (correct)
- Facial, Vestibulocochlear, and Glossopharyngeal
- Vagus, Accessory, and Hypoglossal
Which cranial nerve does NOT pass through the jugular foramen?
Which cranial nerve does NOT pass through the jugular foramen?
Sensory information from the face is primarily carried by which of the following cranial nerves?
Sensory information from the face is primarily carried by which of the following cranial nerves?
A patient has lost the ability to smell following a traumatic head injury. Which of the following cranial nerves has MOST likely been damaged?
A patient has lost the ability to smell following a traumatic head injury. Which of the following cranial nerves has MOST likely been damaged?
Which of the following cranial nerves is NOT involved in taste sensation?
Which of the following cranial nerves is NOT involved in taste sensation?
The axons of the ganglion cells in the retina converge to form which of the following structures?
The axons of the ganglion cells in the retina converge to form which of the following structures?
A patient has difficulty moving their eyeball laterally. Which cranial nerve is MOST likely affected?
A patient has difficulty moving their eyeball laterally. Which cranial nerve is MOST likely affected?
In the visual pathway, which of the following structures is responsible for the decussation (crossing over) of nasal retinal fibers?
In the visual pathway, which of the following structures is responsible for the decussation (crossing over) of nasal retinal fibers?
Damage to Meyer's loop in the visual pathway will MOST likely result in which of the following visual field defects?
Damage to Meyer's loop in the visual pathway will MOST likely result in which of the following visual field defects?
A patient presents with a lesion in the left optic tract. What visual field deficit would you expect to observe?
A patient presents with a lesion in the left optic tract. What visual field deficit would you expect to observe?
Which of the following accurately describes the path of the optic nerve?
Which of the following accurately describes the path of the optic nerve?
Which of the following best describes the type of deficit one would expect with a pituitary tumor compressing the optic Chiasm?
Which of the following best describes the type of deficit one would expect with a pituitary tumor compressing the optic Chiasm?
What is the MOST likely cause of anosmia after a head trauma that involved the ethmoid bone?
What is the MOST likely cause of anosmia after a head trauma that involved the ethmoid bone?
Which statement accurately describes the role of the superior oblique muscle and its innervation?
Which statement accurately describes the role of the superior oblique muscle and its innervation?
When testing the function of the superior rectus muscle, in which position should the eye be placed to isolate its action effectively?
When testing the function of the superior rectus muscle, in which position should the eye be placed to isolate its action effectively?
Which of the following cranial nerves provide motor innervation to the extraocular muscles of the eye?
Which of the following cranial nerves provide motor innervation to the extraocular muscles of the eye?
A patient is unable to adduct their right eye. Which muscle is MOST likely affected, and which nerve innervates it?
A patient is unable to adduct their right eye. Which muscle is MOST likely affected, and which nerve innervates it?
A patient presents with diplopia and reports that the double vision is most noticeable when looking down and to the left. Which cranial nerve is MOST likely affected?
A patient presents with diplopia and reports that the double vision is most noticeable when looking down and to the left. Which cranial nerve is MOST likely affected?
Which extraocular muscle does NOT originate from the common tendinous ring (annulus of Zinn)?
Which extraocular muscle does NOT originate from the common tendinous ring (annulus of Zinn)?
Lateral rectus is innervated by which cranial nerve?
Lateral rectus is innervated by which cranial nerve?
The swinging light test using a penlight would be used to assess which type of pupillary defect?
The swinging light test using a penlight would be used to assess which type of pupillary defect?
What is the primary function of Muller's muscle in the eyelid, and what type of innervation controls it?
What is the primary function of Muller's muscle in the eyelid, and what type of innervation controls it?
Which of the following are parts of the accommodation convergence reflex?
Which of the following are parts of the accommodation convergence reflex?
In the context of pupillary light reflex, what does a consensual response indicate?
In the context of pupillary light reflex, what does a consensual response indicate?
What is the expected outcome of the pupillary light reflex in someone with a complete lesion of the oculomotor nerve (CN III) on the right side?
What is the expected outcome of the pupillary light reflex in someone with a complete lesion of the oculomotor nerve (CN III) on the right side?
A patient presents with ptosis, miosis, and anhidrosis on the right side of their face. Which pathway is likely affected?
A patient presents with ptosis, miosis, and anhidrosis on the right side of their face. Which pathway is likely affected?
Which of these nerve(s) is NOT tested in the corneal reflex?
Which of these nerve(s) is NOT tested in the corneal reflex?
A patient with diabetes reports acute onset of double vision. On examination, they have impaired adduction of the right eye, but their pupillary response is normal. What is the MOST likely location of the lesion?
A patient with diabetes reports acute onset of double vision. On examination, they have impaired adduction of the right eye, but their pupillary response is normal. What is the MOST likely location of the lesion?
What is the MOST likely diagnosis if a patient has paralysis of external ocular muscles but normal pupillary function following a cavernous sinus lesion?
What is the MOST likely diagnosis if a patient has paralysis of external ocular muscles but normal pupillary function following a cavernous sinus lesion?
What is the condition where the eye is pulled 'down and out'?
What is the condition where the eye is pulled 'down and out'?
A patient presents to your office complaining of difficulty with tasks that require convergence of their eyes, tasks like reading and threading a needle. Which of the cranial nerves is potentially damaged?
A patient presents to your office complaining of difficulty with tasks that require convergence of their eyes, tasks like reading and threading a needle. Which of the cranial nerves is potentially damaged?
Superior Oblique (SO) is tested in which gaze position?
Superior Oblique (SO) is tested in which gaze position?
In internuclear ophthalmoplegia (INO), what part of the brain is likely lesioned?
In internuclear ophthalmoplegia (INO), what part of the brain is likely lesioned?
Following a stroke, a patient demonstrates a loss of contralateral horizontal gaze. Which is the MOST likely location of the lesion?
Following a stroke, a patient demonstrates a loss of contralateral horizontal gaze. Which is the MOST likely location of the lesion?
From what level of the spinal cord do the preganglionic neurons that supply the head with sympathetic fibers arise?
From what level of the spinal cord do the preganglionic neurons that supply the head with sympathetic fibers arise?
A patient exhibits anosmia following a fracture involving the cribriform plate. Which of the following mechanisms is the MOST likely cause of their loss of smell?
A patient exhibits anosmia following a fracture involving the cribriform plate. Which of the following mechanisms is the MOST likely cause of their loss of smell?
A patient reports progressive difficulty seeing objects in their peripheral vision. Visual field testing reveals bilateral temporal hemianopia. Where is the MOST likely location of a lesion causing these deficits?
A patient reports progressive difficulty seeing objects in their peripheral vision. Visual field testing reveals bilateral temporal hemianopia. Where is the MOST likely location of a lesion causing these deficits?
A person has a lesion affecting Meyer's loop. Which visual field deficit would MOST likely result from this lesion?
A person has a lesion affecting Meyer's loop. Which visual field deficit would MOST likely result from this lesion?
In a patient with a complete lesion of the right optic tract, which of the following visual field deficits would you expect to observe?
In a patient with a complete lesion of the right optic tract, which of the following visual field deficits would you expect to observe?
Which of the following is the MOST accurate description of the anatomical relationship between the optic chiasm and the pituitary gland?
Which of the following is the MOST accurate description of the anatomical relationship between the optic chiasm and the pituitary gland?
Following a head injury, a patient is unable to elevate their right eye when it is in the abducted position. Which muscle is MOST likely affected, and which nerve innervates it?
Following a head injury, a patient is unable to elevate their right eye when it is in the abducted position. Which muscle is MOST likely affected, and which nerve innervates it?
A patient describes double vision that is WORSE when they look down and in (towards their nose). Which cranial nerve is MOST likely affected?
A patient describes double vision that is WORSE when they look down and in (towards their nose). Which cranial nerve is MOST likely affected?
Which of the following cranial nerves provides motor innervation to the lateral rectus muscle, and what is the PRIMARY action of this muscle?
Which of the following cranial nerves provides motor innervation to the lateral rectus muscle, and what is the PRIMARY action of this muscle?
Where does the superior oblique muscle insert onto the eye, and what is its PRIMARY action when the eye is in an adducted position?
Where does the superior oblique muscle insert onto the eye, and what is its PRIMARY action when the eye is in an adducted position?
During an eye exam, the physician asks the patient to look to their left. Which muscle is primarily responsible for this movement of the right eye, and which cranial nerve innervates it?
During an eye exam, the physician asks the patient to look to their left. Which muscle is primarily responsible for this movement of the right eye, and which cranial nerve innervates it?
A patient exhibits ptosis, miosis, and anhidrosis on the left side of their face. Where is the MOST likely location of the lesion causing these symptoms?
A patient exhibits ptosis, miosis, and anhidrosis on the left side of their face. Where is the MOST likely location of the lesion causing these symptoms?
A patient exhibits a drooping eyelid (ptosis) and impaired pupillary constriction in their right eye. The MOST likely location of the lesion is the:
A patient exhibits a drooping eyelid (ptosis) and impaired pupillary constriction in their right eye. The MOST likely location of the lesion is the:
A patient with a lesion compressing the oculomotor nerve (CN III) exhibits a dilated pupil. Which muscle is MOST directly affected by the disruption of parasympathetic innervation?
A patient with a lesion compressing the oculomotor nerve (CN III) exhibits a dilated pupil. Which muscle is MOST directly affected by the disruption of parasympathetic innervation?
A patient is unable to adduct their right eye. Which of the following muscles is likely affected?
A patient is unable to adduct their right eye. Which of the following muscles is likely affected?
A patient is being tested using the 'H' test, otherwise known as the broad 'H' test. In order to properly assess the Inferior Oblique muscle, in which position should the eye be placed?
A patient is being tested using the 'H' test, otherwise known as the broad 'H' test. In order to properly assess the Inferior Oblique muscle, in which position should the eye be placed?
A patient is being tested using the 'H' test, otherwise known as the broad 'H' test. In order to properly assess the Superior Rectus muscle, in which position should the eye be placed?
A patient is being tested using the 'H' test, otherwise known as the broad 'H' test. In order to properly assess the Superior Rectus muscle, in which position should the eye be placed?
Of the extraocular muscles, which does NOT originate from the common tendinous ring (annulus of Zinn)?
Of the extraocular muscles, which does NOT originate from the common tendinous ring (annulus of Zinn)?
You suspect a patient has damage to their Trochlear nerve (CN IV). In what position should you have your patient look to best isolate this nerve's functionality?
You suspect a patient has damage to their Trochlear nerve (CN IV). In what position should you have your patient look to best isolate this nerve's functionality?
A patient presents with diplopia and demonstrates limited adduction of the right eye. Which of the following muscles and innervating cranial nerves is MOST likely affected?
A patient presents with diplopia and demonstrates limited adduction of the right eye. Which of the following muscles and innervating cranial nerves is MOST likely affected?
Which nerve provides parasympathetic innervation to the ciliary muscle, facilitating accommodation for near vision?
Which nerve provides parasympathetic innervation to the ciliary muscle, facilitating accommodation for near vision?
A patient has difficulty with accommodation, specifically focusing on near objects. Which muscle is likely affected?
A patient has difficulty with accommodation, specifically focusing on near objects. Which muscle is likely affected?
Following a traumatic brain injury, a patient displays a loss of pupillary constriction in response to light in the left eye, but the pupillary constriction reflex is still intact in the right eye. Where is the MOST likely location of the lesion?
Following a traumatic brain injury, a patient displays a loss of pupillary constriction in response to light in the left eye, but the pupillary constriction reflex is still intact in the right eye. Where is the MOST likely location of the lesion?
Which structure is responsible for relaying visual information from the optic tract to the visual cortex?
Which structure is responsible for relaying visual information from the optic tract to the visual cortex?
A patient has a lesion that disrupts the sympathetic innervation to their right eye. Which sign would you MOST likely observe?
A patient has a lesion that disrupts the sympathetic innervation to their right eye. Which sign would you MOST likely observe?
What is the PRIMARY function of the swinging flashlight test, and what does a positive result indicate?
What is the PRIMARY function of the swinging flashlight test, and what does a positive result indicate?
What part of the reflexive response of the Accommodation Convergence Reflex changes the shape of the lens?
What part of the reflexive response of the Accommodation Convergence Reflex changes the shape of the lens?
If damage to the Optic nerve is suspected, what test should be used, and what is the clinical sign that will be seen?
If damage to the Optic nerve is suspected, what test should be used, and what is the clinical sign that will be seen?
You suspect your patient exhibits cavernous sinus thrombosis. Which symptoms might you expect to see?
You suspect your patient exhibits cavernous sinus thrombosis. Which symptoms might you expect to see?
Flashcards
Why study cranial nerves?
Why study cranial nerves?
Cranial nerve can be affected in numerous medical and surgical conditions.
CN I
CN I
Olfactory nerve; detects smells.
CN II
CN II
Optic nerve; vision.
CN III
CN III
Signup and view all the flashcards
CN IV
CN IV
Signup and view all the flashcards
CN V
CN V
Signup and view all the flashcards
CN VI
CN VI
Signup and view all the flashcards
CN VII
CN VII
Signup and view all the flashcards
CN VIII
CN VIII
Signup and view all the flashcards
CN IX
CN IX
Signup and view all the flashcards
CN X
CN X
Signup and view all the flashcards
CN XI
CN XI
Signup and view all the flashcards
CN XII
CN XII
Signup and view all the flashcards
Cribriform Plate
Cribriform Plate
Signup and view all the flashcards
Optic Canal
Optic Canal
Signup and view all the flashcards
Superior Orbital Fissure
Superior Orbital Fissure
Signup and view all the flashcards
Foramen Rotundum
Foramen Rotundum
Signup and view all the flashcards
Foramen Ovale
Foramen Ovale
Signup and view all the flashcards
Internal Acoustic Meatus
Internal Acoustic Meatus
Signup and view all the flashcards
Stylomastoid Foramen
Stylomastoid Foramen
Signup and view all the flashcards
Jugular Foramen
Jugular Foramen
Signup and view all the flashcards
Hypoglossal Canal
Hypoglossal Canal
Signup and view all the flashcards
Sensory Nerves
Sensory Nerves
Signup and view all the flashcards
Purely Sensory CNs
Purely Sensory CNs
Signup and view all the flashcards
Motor Nerves
Motor Nerves
Signup and view all the flashcards
Purely Motor CNs
Purely Motor CNs
Signup and view all the flashcards
Mixed Nerves
Mixed Nerves
Signup and view all the flashcards
Mixed Sensory & Motor
Mixed Sensory & Motor
Signup and view all the flashcards
Parasympathetic Nerves
Parasympathetic Nerves
Signup and view all the flashcards
Parasympathetic CNs
Parasympathetic CNs
Signup and view all the flashcards
Iris
Iris
Signup and view all the flashcards
Ciliary Muscle
Ciliary Muscle
Signup and view all the flashcards
Sympathetic Supply
Sympathetic Supply
Signup and view all the flashcards
CN III Exits
CN III Exits
Signup and view all the flashcards
Complete CN III Palsy
Complete CN III Palsy
Signup and view all the flashcards
CN VI Palsy
CN VI Palsy
Signup and view all the flashcards
Horizontal Diplopia
Horizontal Diplopia
Signup and view all the flashcards
Conjugate gaze
Conjugate gaze
Signup and view all the flashcards
PPRF
PPRF
Signup and view all the flashcards
Corneal Reflex
Corneal Reflex
Signup and view all the flashcards
Pupillary Light Reflex
Pupillary Light Reflex
Signup and view all the flashcards
Relative Afferent Pupillary Defect
Relative Afferent Pupillary Defect
Signup and view all the flashcards
Accommodation Convergence
Accommodation Convergence
Signup and view all the flashcards
Cavernous Sinus Thrombosis
Cavernous Sinus Thrombosis
Signup and view all the flashcards
Trochlear Nerve
Trochlear Nerve
Signup and view all the flashcards
Muscle Function Problem
Muscle Function Problem
Signup and view all the flashcards
MLF Lesion
MLF Lesion
Signup and view all the flashcards
Abducens Nerve
Abducens Nerve
Signup and view all the flashcards
Oculomotor Nerve
Oculomotor Nerve
Signup and view all the flashcards
Study Notes
- The lecture provides valuable clinical neuroanatomy insights into the cranial nerves (CNs).
Why Study Cranial Nerves?
- Cranial nerves, or CNs, are susceptible to various medical and surgical conditions.
- Common causes of CN dysfunction include: diabetic/hypertensive neuropathy, stroke, compressive lesions like tumors or aneurysms, trauma such as fractures/lacerations, vasculitis, and congenital issues.
- Comprehending CN functions, anatomy, pathways, and significant relations aids in testing CNs and interpreting neurological signs to determine causes of dysfunction.
Overview of Cranial Nerves
- CN I is the Olfactory nerve responsible for the sense of smell and exits from nerves through bones.
- CN II is the Optic nerve which facilitates vision.
- CN III is the Oculomotor nerve, crucial for eye movement and exists between cerebral peduncles.
- CN IV is the Trochlear nerve also involved in eye movement.
- CN V is the Trigeminal nerve, the largest cranial nerve, responsible for facial sensation and chewing.
- CN VI is the Abducens nerve, important for eye abduction and is tiny, originating at the midline.
- CN VII is the Facial nerve, lateral to the abducens, for facial expressions and taste.
- CN VIII is the Vestibulocochlear nerve, positioned at the cerebellopontine angle, responsible for hearing and balance.
- CN IX is the Glossopharyngeal nerve, contributing to swallowing, salivation, and taste.
- CN X is the Vagus nerve, influential in various bodily functions, including heart rate and digestion, originating in the medulla between the olive.
- CN XI is the Accessory nerve, which controls neck and shoulder muscles, runs between medulla and inferior cerebellar peduncle.
- CN XII is the Hypoglossal nerve, essential for tongue movement, emerging between the pyramid and olive.
Cranial Nerves and Foramina
- Understanding which cranial nerves pass through specific foramina is crucial for diagnosing neurological conditions.
- CN I (Olfactory) passes through the cribriform plate of the ethmoid bone.
- CN II (Optic) passes through the optic canal.
- CN III (Oculomotor), CN IV (Trochlear), CN V₁ (Ophthalmic branch of Trigeminal), and CN VI (Abducens) pass through the superior orbital fissure.
- CN V₂ (Maxillary branch of Trigeminal) passes through the foramen rotundum.
- CN V₃ (Mandibular branch of Trigeminal) passes through the foramen ovale.
- CN VII (Facial) and CN VIII (Vestibulocochlear) pass through the internal acoustic meatus and the facial N then continues through the stylomastoid foramen.
- CN IX (Glossopharyngeal), CN X (Vagus), and CN XI (Accessory) pass through the jugular foramen.
- CN XII (Hypoglossal) passes through the hypoglossal canal.
Functional Classification of Cranial Nerves
- Cranial nerves are categorized by function: sensory, motor, mixed sensory & motor, and parasympathetic.
- Sensory nerves include: CN I (Olfactory), CN II (Optic), and CN VIII (Vestibulocochlear).
- Motor nerves include: CN III (Oculomotor), CN IV (Trochlear), CN VI (Abducens), CN XI (Accessory), and CN XII (Hypoglossal).
- Mixed sensory & motor nerves include: CN V (Trigeminal), CN VII (Facial), CN IX (Glossopharyngeal), and CN X (Vagus).
- Parasympathetic nerves include: CN III (Oculomotor), CN VII (Facial), CN IX (Glossopharyngeal), and CN X (Vagus).
Cranial Nerve Nuclei
- Specific nuclei in the brainstem are associated with particular cranial nerves and their functions.
- Sensory nuclei: Mesencephalic, Chief sensory, and Spinal nuclei.
- Trigeminal nuclei are located in the pons.
- Spinal nuclei extend from the pons to the medulla.
- Motor nuclei: Edinger-Westphal, Oculomotor, Trochlear, Trigeminal Motor, Abducens, Facial Motor, Superior salivatory, Inferior salivatory, Ambiguus, and Hypoglossal.
- The Edinger-Westphal nucleus is located in the superior midbrain. Oculomotor and Trochlear nuclei are in the midbrain, posterior. motor nuclei found in lower pons
- Abducens and Facial Motor nuclei are located in the lower pons. The superior salivatory nucleus is located in the lower pons, in pontine tegmentum. Ambiguus is found in the medulla. Hypoglossal found in medulla, more medial.
- Parasympathetic system: Cell bodies of preganglionic neurons are always in the CNS; postganglionic neurons are outside the CNS within peripheral ganglia.
CN I - Olfactory Nerve & Pathway
- The olfactory pathway begins in the olfactory neuroepithelium in the roof of the nose.
- Olfactory nerves pass through the cribriform plate of the ethmoid bone and synapse with second-order neurons in the olfactory bulb.
- The olfactory tract then leads to the olfactory cortex.
- There is bilateral cortical representation of smell.
- Olfactory nerve damage can lead to anosmia (loss of smell), often caused by local issues like upper respiratory tract infections or head injuries involving the ethmoid bone.
Optic Nerve & Vision - Visual Fields
- The entire area visible to an eye when focused on a single point constitutes the visual field.
- Each eye has its own monocular visual field.
- Visual fields are divided into superior, inferior, nasal (medial), and temporal (lateral) quadrants for descriptive purposes.
Extents of Monocular Visual Fields
- The shape of the visual field of each eye is oval and spans approximately 60º nasally, 100º temporally, 60º superiorly, and 70° inferiorly.
- Central (macular) vision (central 30°) is used for focused activities like reading and recognizing faces.
- Peripheral vision detects motion and provides spatial awareness.
Binocular Visual Field
- Binocular vision results from the overlap of the visual fields of both eyes when used simultaneously.
- Binocular vision allows for increased depth perception and a better ability to perceive 3D space.
Visual Pathway - Representation of Visual Fields in Retina
- Visual fields are registered as left-right reversed and inverted on the retina.
- The temporal field projects to the nasal retina, and the nasal field projects to the temporal retina.
- The superior field projects to the inferior retina, and the inferior field projects to the superior retina.
Visual Pathway - Retina & Optic Nerve
- The visual pathway begins in the photoreceptor layer of the retina.
- Rods, highly sensitive to light, facilitate night vision and peripheral vision (low resolution).
- Cones mediate color vision and high-resolution vision (high acuity).
- Photoreceptors synapse with bipolar cells, which then synapse with ganglion cells; these ganglion cell axons make up the optic nerve.
Visual Pathway - Components
- The optic nerve carries visual information from the retina to the optic chiasm.
- At the optic chiasm, fibers from the nasal visual fields cross (decussation).
- The optic tract carries information to the lateral geniculate nucleus in the thalamus.
- From there, the optic radiation projects to the primary visual cortex (on either side of the calcarine sulcus via Meyer's loop and Baum's loop).
Field Defects
- Various lesions along the visual pathway result in specific visual field defects.
- A lesion at the optic chiasm can cause bitemporal hemianopia.
- A lesion after the optic chiasm, such as the optic tract, Meyer's loop, or optic radiation, can cause homonymous hemianopia.
CN II - Optic Nerve & Visual Pathway
- The optic nerve carries axons from the four quadrants of each retina.
- It travels backward through the orbital cavity and optic canal.
- Nasal fibers from both nerves cross at the optic chiasm, which lies anterior to the pituitary gland.
Testing Visual Fields and Acuity
- Visual field examination is performed clinically using confrontation testing but can also be examined using perimetry.
- Visual acuity can be tested using a Snellen's chart
- Ishihara charts are used to test color vision .
Cranial Nerves III, IV, VI
- Cranial nerves III, IV, and VI are pure motor nerves.
- These innervate the muscles related to eyes.
- They innervate skeletal muscles (extraocular muscles).
- As well as smooth muscles.
Extra Ocular Muscles
Note that there are 6 extra-ocular muscles (4 recti + 2 obliques). The four recti muscles are superior rectus, medial rectus, inferior rectus, and lateral rectus. The two oblique muscles are superior oblique and inferior oblique. All muscles except inferior oblique originate from the common tendinous ring (around the optic nerve).
Axis of Eye Movements
- Vertical Axis involves Abduction / Adduction
- Horizontal Axis involves Intorsion / Extorsion
- AP Axis Elevation / Depression
Eye Muscles
- Medial rectus and Lateral rectus rotate only around Vertical axis.
- Medial rectus is the main Adductor of eyeball.
- Lateral rectus is the main Abductor of eyeball.
- Best position to test the SR is Elevation in the abducted position
- Best position to test the SR is Elevation in the abducted position
Superior Oblique Muscles
- AP axis is the main axis involves Intortion.
- Vertical axis is the main axis Abduct.
- Transverse axis is the main axis Depress. Best position to test the SO is Depression in the adducted position.
Inferior Rectus Muscles
- Involves Adduct and Extort.
- The best position to test the IR is Depression in the abducted position.
Innervation of the Extra Ocular Muscles
- Lateral rectus is CN – VI.
- Superior Oblique is CN – IV.
- All other muscles CN - III.
Oculomotor Nerve – Somatic Innervation
- CN III innervates the Levator palpebrae superioris Muscle and elevates eyelid
- Controls Nucleus in Upper Midbrain and is responsible for elevating abducted/neutral eye
Oculomotor Nerve – Visceral Innervation
- Alters pupillary diameter by controlling the amount of light entering the retina with Dilators pupillae and Sphincter pupillae
- Alters lens curvature to Focus distant and near objects on retina (Accommodation).
Head & Neck sympathetic Supply
- Sympathetic pathways start from the hypothalamus, the control centre of the autonomic nervous system.
- From hypothalamus, the descending sympathetic pathway runs through the brainstem (note this runs in the lateral medulla*) into the spinal cord where sympathetic out flow (Lateral gray horns of T1 to L2 segments) is located.
- Preganglionic neurons that supply upper limb and head starts in the T1 lateral horn.
- These preganglionic neurons exit the spinal cord with the motor roots and then pass into the sympathetic chain. Then ascends and synapses with the post ganglionic neurons inside cervical sympathetic ganglia.
- Postganglionic Neurons then exits the ganglia and travels with the internal carotid artery (internal carotid plexus) to supply smooth muscles related to eye.
- Post ganglionic Neurons that join the external carotid artery supply the sweat glands and blood vessels in face.
- In the cavernous sinus these neurons join the terminal branches of the ophthalmic nerve that runs into the eye (Long ciliary nerves) to supply ciliary and iris muscles.
Pathway of CN III Exit
- CN III enters in interpeduncular fossa
- Passes through Medial Temporal lobe – Uncus
- Lies Between PCA & Sup cerebellar. A
- Runs with P Com A* and along the Lateral wall of Cavernous sinus (with CNIV, V, VI)
- Exits through the Superior Orbital fissure (with CNIV,V, VI)
Complete CN III Palsy
- Consists of Complete Ptosis due to loss of support of LPS
- Leads to Elevation issues in the Superior rectus leading to not elevating abducted/neutral/Adducted eye
- Causes Depression issues due to loss of support to Inferior rectus leading to a failure to depress the abducted eye
- Can cause Adduction issues as the Medial rectus faces Adduction deficit
- Constrictor pupillae stops working as it struggles to react to light and CANNOT Dilate
- Ciliary muscle stops working which causes a loss of accomodation
Clinical Scenario 1 of eye
- Patient presents with pain on the right eye and inability to open the eye because of diabetic
- Examination reveals
- Causing Complete ptosis of right eye
- Leads to Abduction and slight depression of the right eye
- This makes the patients Unable to adduct or even pass midline
- Causes Elevation and depression of the right eye to become compromised
- Leads to Both pupils being equal in size and reactive to light
- Indicates that Parasympathetic axons are in the periphery to Motor axons are in the centre
Path of Abducens Nerve
- Lateral rectus is CN – VI
- Superior Oblique is CN – IV
- All other CN - III
Function of Oculomotor Lesion
- Anteriorly over petrous bone, + cavernous sinus, inside the sinus - to superior orbital fissure Vulnerable for injury due to raised ICP
- Stretching/compression, Sudden movement of the brain - stretching/sever
Abducens Nerve Palsy
- These patients presents with Binocular horizontal diplopia from Horizontal double vision.
- Paralysis may occur in neutral position and aggravates when looking to the side of paralytic muscle
Diagnosing Diplopia
- Patient has diplopia looking to the Right
- That means either Left medial rectus or Right lateral rectus may be paretic
- The most lateral image is the one you have to focus on
- To Test deficits, check covering of which eye cause disappearance of the peripheral image
Extra Ocular Muscles - Conjugate Gaze
- Eyes in same direction at same time.
- The conjugate gaze is the movement of both eyes in the same direction at the same time. (Convergence gaze is where both eyes move inwards at the same time.)
- Leads to Conjugate gaze involving simultaneous contraction of a set of ipsilateral
- Can produce contralateral muscles that control Yoke muscles in (Eg: LR and MR during horizontal gaze).
- Form images in spatially analogous parts of retina then allows braion to interpret as single images. To aid functionality Conjugate gaze helps both eyes in coordinated manner to help form a single sharp image of an object in spatially analogous parts of the 2 retinae for e.g. fovea - information goes to analogous parts of the visual cortex helps brain interpret it as single image.
- Creates Disconjugated gaze when muscle or nerve pathology occurs which results in Binocular diplopia and Double vision. To counteract disconjugate images:
- Leads to Binocular diplopia which can be avoided by closing one eye or by sometimes by compensatory head tilts/movements.
Control of Conjugate Gaze
- Most of our normal voluntary conjugate eye movements occur in small "jumps" or saccades
- When tracking a moving object, , instead of saccades, we use smooth pursuit movements.
Pathway - Cranial Nerves
- Cranial Nerves use Saccades which run Contralateral from FEF or Ipsilateral with Parapontine reticular form via the main system
- For Vertical eye tracking it runs from Multiple Cortical sites - Upper Dorsal Midbrain complex
Cavernous Sinus
- Contains multipel cranial nerve III, IV, opthalmic
- Has to be connected and around Abducens
- Connects to internal carotid artery
- Then CN III, IV, Maxillary and Ophthalmic nerves inside the lateral wall
- Helps Veins Drain blood from Face, Maxillary teeth, Pharynx and Air sinuses
Cavernous sinus thrombosis
- Often as Infections spread via these veins to the CS
- Results Swellings increase pressure over Sinus
- Affects venous drainage of eye causing oedema/pain/headache
- Then puts Pressure on CNs – Single or Multiple CN palsies in (III, IV, V3, VI)
- While increasing Pressure on Carotid artery – Cerebral ischemia can occur
Corneal Reflex
- Aids Protective reflex against FB touching the cornea and is Operates at the level of the pons
- By producing Sensory responses such as- Touching the Stimulus Touch to Sclera or Cornea with facial nerve and ophthalmic nerve
- Which aids Motor responses such a Contraction through muscle in bilateral orbicularis oculi supplied in by facial nerve
- Therefore Corneal reflex on the right side is absent when there is left cerebral peduncle infarct.
- While on the other hand if Left sided blindness wont lead to abolition of left corneal reflex. False false
Pupillary Light Reflex
Used in test through components such as what's sensory such as light via optic nerve or components Such as Constriction via Oculomotor when tested Shining test such as if "What is direct pupillary light reflex?" If its right what about opposite
Efferent Pupillary Defect (PS)
- In order to check we must consider eye position if
- Efferent pathway "What is efferent pathway” lesions do abolishing the Direct and consensual test, what other response it effects
Afferent Pupillary Defect Path
what would be the test if afferent in CN test of what happens to afferent eye tests while check the other side Then check if signal still work both eye Therefore “Afferent pathway” lesions is abolish direct test so you can the damage to right and left
Relative Afferent Pupillary
defects (RAPD) - Helps identify damage due to partial damage in retinal nerve Using by presenting a reduced vision of by unilateral partial lesion Involve Swinging light test (located in optic nerve/retina) in "locate lesions" Which results in Common conditions are found in (Eg.MS) in:
- Optic neuritis (Eg.MS) ,Optic nerve ischaemia, Glaucoma, Retinal detachment
RAPD - Swinging Light Test
- Needs to be Bright but Dim light conditions (and make sure make to Gaze condition) into the distance
- Then Shine Penlight into 1 eye and look for the Maximum test Pupil Constriction
- Repeat by: Switching Quickly to Test light in "Test switch" -Other eye
Common Disodes Test
- Help Find Nerves using Optics
- Retina aids to find if there What about - APD, "signs" and "affects"
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.