Podcast
Questions and Answers
What is the primary cause of chronic pyelonephritis?
What is the primary cause of chronic pyelonephritis?
- Recurrent inflammation and scar
- Bacterial infection
- Chronic kidney disease
- Obstructive abnormalities or vesicoureteral reflux (correct)
What is a common clinical manifestation of chronic pyelonephritis?
What is a common clinical manifestation of chronic pyelonephritis?
- Mild proteinuria (correct)
- Recurrent upper respiratory infections
- Loss of renal function
- Severe hypertension
What is a complication of chronic pyelonephritis?
What is a complication of chronic pyelonephritis?
- Renal failure (correct)
- Lower respiratory infections
- Bone fractures
- Chronic kidney disease
What is the primary role of the kidney in renal osteodystrophy?
What is the primary role of the kidney in renal osteodystrophy?
What is a characteristic of low bone turnover of osteodystrophy?
What is a characteristic of low bone turnover of osteodystrophy?
What is a common symptom of renal osteodystrophy?
What is a common symptom of renal osteodystrophy?
What is a consequence of impaired kidney function in renal osteodystrophy?
What is a consequence of impaired kidney function in renal osteodystrophy?
What is the effect of chronic pyelonephritis on renal function?
What is the effect of chronic pyelonephritis on renal function?
What is a common finding in chronic pyelonephritis?
What is a common finding in chronic pyelonephritis?
What is a consequence of reflux in chronic pyelonephritis?
What is a consequence of reflux in chronic pyelonephritis?
What is the primary function of parathyroid hormone in maintaining stable calcium levels?
What is the primary function of parathyroid hormone in maintaining stable calcium levels?
What is the primary treatment for renal osteodystrophy?
What is the primary treatment for renal osteodystrophy?
What is the most common type of azotemia?
What is the most common type of azotemia?
What is the primary cause of acute tubular necrosis?
What is the primary cause of acute tubular necrosis?
What is the primary indicator of acute kidney injury?
What is the primary indicator of acute kidney injury?
What is the primary cause of glomerulonephritis?
What is the primary cause of glomerulonephritis?
What is the primary sign of acute glomerulonephritis?
What is the primary sign of acute glomerulonephritis?
What is the primary risk factor for developing Wilms' tumor?
What is the primary risk factor for developing Wilms' tumor?
What is the primary treatment for renal cell carcinoma?
What is the primary treatment for renal cell carcinoma?
What is the primary function of calcitriol in calcium absorption?
What is the primary function of calcitriol in calcium absorption?
Flashcards are hidden until you start studying
Study Notes
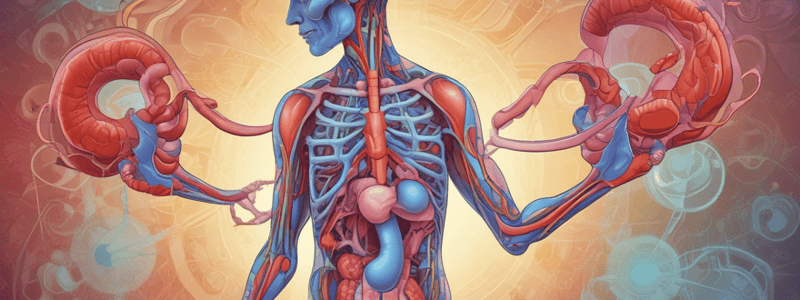
Chronic Pyelonephritis
- Characterized by scarring and deformation of renal calyces and pelvis
- Caused by bacterial infection superimposed on obstructive abnormalities or vesicoureteral reflux
- Occurs due to recurrent inflammation and scarring
- Reflux is the most common cause
- Clinical manifestations may include:
- Chills, high fever, and aches/tenderness of the flank and low back
- Urinary tract symptoms such as dysuria and frequency
- Recurrent UTIs
- Loss of tubular function and ability to concentrate urine
- Polyuria and nocturia
- Mild proteinuria
- Severe hypertension (progresses disease)
Reno Osteodystrophy
- Occurs in adults and children with chronic kidney disease
- Results from changes in mineral levels and hormones due to impaired kidney function
- Characterized by low bone turnover, decrease of osteoblasts, and low or reduced number of osteoclasts
- May cause bone tenderness, muscle weakness, and bone fractures
- Kidney roles in renal osteodystrophy:
- Decrease calcium levels
- Increase phosphorus levels
- Increase parathyroid hormone (PTH)
- Activate vitamin D to produce calcitriol, which aids in calcium absorption
- Treatment involves:
- Treating hyperphosphatemia and hypocalcemia
- Vitamin D to increase calcium levels
- Phosphate binding antacids
Prerenal Azotemia
- Most common type of azotemia
- Caused by accumulation of nitrogenous waste in the blood and a decrease in GFR
- Results in excretion of nitrogenous waste, reduction of fluid and electrolyte balance
- Seen in glomerular disorders
- Occurs when there is not enough blood flow to the kidney
- Causes include:
- Blood loss
- Dehydration
- Heart failure
- Liver failure
- Certain medications
Acute Tubular Necrosis
- Most common cause of intrinsic failure
- Occurs secondary to ischemic or toxic injury to renal tubules
- Occurs when arteriole pressure (MAP) is decreased
- Afferent and efferent arterioles lose their regulatory process with hypoperfusion
- Sympathetic stimulation and angiotensin II cause severe vasoconstriction
- Hypoxia leads to cellular damage, epithelial cells slough into the lumen, and tubular pressure increases
- Tubular injury and necrosis cause a leak of glomerular filtrate
- The tubular epithelial is disrupted, leading to increased BUN, creatinine, and potassium levels
Extreme Proteinuria
- Also known as nephrotic range proteinuria
- Defined as >3000 mg (3g) protein per day
- Associated with conditions such as nephrotic syndrome and glomerulonephritis
- Lab considerations include:
- Urine dipstick test
- 24-hour urine collection
- Albumin to creatinine ratio (ACR)
Glomerulonephritis
- Acute poststreptococcal Glomerulonephritis (PSGN) is the most common form
- Occurs 7-12 days following an infection (usually throat or skin infection with group A hemolytic strep)
- Caused by antigen/antibody complex formation and complement deposition on the glomerulus
- Signs and symptoms include:
- Sudden hematuria
- Edema
- Hypertension
- Renal insufficiency
- In children, the prognosis is favorable, with 95% recovering without renal damage
- In adults, only 60% recover favorably, with the remainder developing permanent kidney damage
Renal Cell Carcinoma
- Two major groups of renal neoplasms:
- Embryonic kidney tumors (e.g., Wilms' tumor)
- Renal cell carcinoma (accounts for 80-90% of kidney tumors)
- Lack of warning signs
- Resistant to chemo/radiation
- Diagnosed by ultrasound or CT scan
- Treatment involves surgical resection
- Five-year survival rate is 90% before metastasis
Syndrome of Inappropriate ADH (SIADH)
- Caused by increased ADH release
- Increased reabsorption of water in the collecting tube
- Decreased water in the filtrate
- Increased urinary output (as kidney absorbs more water)
- Concentrated urine (increased specific gravity, can be > 1.020)
- Clinically:
- Patient appears edematous
- Decreased sodium
- Increased weight gain
- Can be seen in patients with CNS disease
- Increased ADH when patients are in pain (e.g., surgery, asphyxia, pneumothorax)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.