Podcast
Questions and Answers
What is the greatest risk factor for chronic bronchitis?
What is the greatest risk factor for chronic bronchitis?
- Air pollution
- High altitude exposure
- Alpha1-antitrypsin deficiency
- Cigarette smoking (correct)
Which of the following symptoms is commonly associated with hypoxemia in COPD patients?
Which of the following symptoms is commonly associated with hypoxemia in COPD patients?
- Barrel chest (correct)
- Weight gain
- Bradycardia
- Increased appetite
Which of the following strategies is recommended for managing dyspnea in COPD patients?
Which of the following strategies is recommended for managing dyspnea in COPD patients?
- Avoiding all physical activity
- Eating large meals to maintain energy
- Pursed lip breathing before eating (correct)
- Engaging in high-intensity workouts
What is the target oxygen saturation range for patients with COPD during treatment?
What is the target oxygen saturation range for patients with COPD during treatment?
Which complication can arise due to high CO2 levels in COPD patients?
Which complication can arise due to high CO2 levels in COPD patients?
What type of dietary approach is recommended for COPD patients to prevent weight loss?
What type of dietary approach is recommended for COPD patients to prevent weight loss?
What is a common psychosocial recommendation for managing anxiety in COPD patients?
What is a common psychosocial recommendation for managing anxiety in COPD patients?
What is a key method to improve endurance in COPD patients?
What is a key method to improve endurance in COPD patients?
What is the primary goal of self-management education for a client with COPD?
What is the primary goal of self-management education for a client with COPD?
Which outcome indicates effective management of COPD in a patient?
Which outcome indicates effective management of COPD in a patient?
What statement by a COPD patient would indicate a possible increase in dyspnea?
What statement by a COPD patient would indicate a possible increase in dyspnea?
What assessment finding mandates nursing intervention for a client with a chest tube?
What assessment finding mandates nursing intervention for a client with a chest tube?
What is the primary problem in emphysema as it relates to lung function?
What is the primary problem in emphysema as it relates to lung function?
Which preventive measure is essential for managing COPD?
Which preventive measure is essential for managing COPD?
Which statement best describes chronic bronchitis?
Which statement best describes chronic bronchitis?
When a patient with asthma shows a PEF reading in the red zone, what is the most critical nursing action?
When a patient with asthma shows a PEF reading in the red zone, what is the most critical nursing action?
What clinical symptom is commonly associated with gas exchange problems in COPD?
What clinical symptom is commonly associated with gas exchange problems in COPD?
What is a key objective in conducting effective health promotion for clients with COPD?
What is a key objective in conducting effective health promotion for clients with COPD?
Which indicator most clearly suggests that a COPD patient's breathing pattern is improving?
Which indicator most clearly suggests that a COPD patient's breathing pattern is improving?
What is a consequence of the excessive mucus produced in chronic bronchitis?
What is a consequence of the excessive mucus produced in chronic bronchitis?
What triggers the inflammation seen in chronic bronchitis?
What triggers the inflammation seen in chronic bronchitis?
Which aspect of gas exchange is typically decreased in patients with COPD?
Which aspect of gas exchange is typically decreased in patients with COPD?
What is a significant outcome of hyperinflation of the lungs in emphysema?
What is a significant outcome of hyperinflation of the lungs in emphysema?
Which of the following best characterizes the pathophysiology of COPD?
Which of the following best characterizes the pathophysiology of COPD?
Which of the following complications can arise from chronic bronchitis in COPD patients?
Which of the following complications can arise from chronic bronchitis in COPD patients?
What is the primary benefit of pursed lip breathing for COPD patients?
What is the primary benefit of pursed lip breathing for COPD patients?
Which dietary approach is advised for COPD patients to combat weight loss?
Which dietary approach is advised for COPD patients to combat weight loss?
Why is careful monitoring of CO2 levels crucial in COPD patients?
Why is careful monitoring of CO2 levels crucial in COPD patients?
What is the common psychosocial challenge faced by COPD patients?
What is the common psychosocial challenge faced by COPD patients?
What is an effective strategy for improving endurance in COPD patients?
What is an effective strategy for improving endurance in COPD patients?
What is the primary pathological change that occurs in emphysema?
What is the primary pathological change that occurs in emphysema?
Which risk factor aside from smoking can significantly contribute to COPD?
Which risk factor aside from smoking can significantly contribute to COPD?
Which of the following accurately describes the physiological impact of chronic bronchitis on airflow?
Which of the following accurately describes the physiological impact of chronic bronchitis on airflow?
What does a high CO2 level in COPD patients indicate about their condition?
What does a high CO2 level in COPD patients indicate about their condition?
What sensory experience might a COPD patient report due to impaired gas exchange?
What sensory experience might a COPD patient report due to impaired gas exchange?
Which statement is true regarding the role of irritants in the pathophysiology of chronic obstructive pulmonary disease?
Which statement is true regarding the role of irritants in the pathophysiology of chronic obstructive pulmonary disease?
What effect does hyperinflation of the lungs have on the respiratory system in patients with emphysema?
What effect does hyperinflation of the lungs have on the respiratory system in patients with emphysema?
Which characteristic is typical of the bronchial response in chronic bronchitis?
Which characteristic is typical of the bronchial response in chronic bronchitis?
What is a common pathological result of bronchial thickening due to chronic inflammation in COPD?
What is a common pathological result of bronchial thickening due to chronic inflammation in COPD?
How does chronic exposure to cigarette smoke impact airway physiology in COPD?
How does chronic exposure to cigarette smoke impact airway physiology in COPD?
Which outcome is least likely to be expected in a client with COPD related to effective self-management?
Which outcome is least likely to be expected in a client with COPD related to effective self-management?
What clinical finding in a patient with COPD suggests poor gas exchange should be addressed promptly?
What clinical finding in a patient with COPD suggests poor gas exchange should be addressed promptly?
Which statement about drug therapy in COPD management is most accurate?
Which statement about drug therapy in COPD management is most accurate?
Which strategy is least beneficial for a COPD patient to enhance breathing patterns?
Which strategy is least beneficial for a COPD patient to enhance breathing patterns?
What is the main objective of health care resources for patients with COPD?
What is the main objective of health care resources for patients with COPD?
Which assessment finding would most likely indicate worsening lung function in a COPD patient?
Which assessment finding would most likely indicate worsening lung function in a COPD patient?
Which patient education topic is essential for preventing respiratory infections in COPD patients?
Which patient education topic is essential for preventing respiratory infections in COPD patients?
What can be inferred if a COPD patient maintains a consistent body weight outside of 10% of their ideal weight?
What can be inferred if a COPD patient maintains a consistent body weight outside of 10% of their ideal weight?
Flashcards are hidden until you start studying
Study Notes
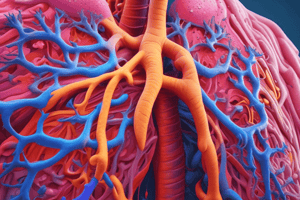
COPD Overview
- Chronic Obstructive Pulmonary Disease (COPD) affects approximately 15 million people in the U.S. and 900,000 in Canada.
- It is the 4th leading cause of morbidity and mortality in the U.S.
- COPD encompasses disorders that interfere with airflow and gas exchange, primarily including emphysema and chronic bronchitis.
Emphysema
- Characterized by the destruction of lung elastic tissue, reducing recoil ability, and leading to lung hyperinflation.
- Damaged alveoli result in air trapping, decreased gas exchange, increased work of breathing, and sensations of "air hunger."
- Common symptoms include increased CO2 retention and respiratory acidosis.
Chronic Bronchitis
- Inflammation of bronchi and bronchioles due to irritants, especially cigarette smoke.
- Causes airflow impairment through increased mucus secretion and thickening of bronchial walls.
- Contributes to chronic infection due to mucus accumulation and provides a breeding ground for pathogens.
Risk Factors
- Major risk factor for COPD is cigarette smoking.
- Genetic risk includes alpha1-antitrypsin deficiency.
- History of asthma may increase susceptibility to COPD.
Complications of COPD
- Hypoxemia and acidosis are significant concerns.
- Common complications include respiratory infections, cor pulmonale (cardiac failure due to lung disease), dysrhythmias, and respiratory failure.
Assessment of COPD
- Physical assessment should recognize signs like barrel chest, abnormal respiratory and cardiac changes.
- Laboratory assessment might include arterial blood gases (ABGs), indicating hypoxemia and hypercapnia (excess CO2).
- Monitor oxygen saturation (aim for 88-92%) and assess treatment responses.
Management Strategies
- Focus on dyspnea management through small, high-calorie meals and controlled breathing techniques (e.g., pursed-lip breathing).
- Address anxiety through counseling, relaxation techniques, and support systems.
- Encourage smoking cessation as a critical intervention for improving patient outcomes.
Health Promotion and Maintenance
- Educate patients about self-management strategies, including drug therapy and effective breathing techniques.
- Emphasize the importance of avoiding respiratory infections and achieving baseline gas exchange levels.
Evaluation of Patient Outcomes
- Goals include maintaining a stable gas exchange, an effective breathing pattern, patent airways, ideal body weight, decreased anxiety, and acceptable activity levels.
NCLEX Style Questions
- Recognize the significance of patient statements that may indicate worsening conditions (e.g., sleep positioning in COPD patients).
- Assess findings from procedures such as pneumonectomy recovery and the implications for nursing intervention.
- Understand priority actions in acute asthma management based on peak flow meter readings.
COPD Overview
- Chronic Obstructive Pulmonary Disease (COPD) affects approximately 15 million people in the U.S. and 900,000 in Canada.
- It is the 4th leading cause of morbidity and mortality in the U.S.
- COPD encompasses disorders that interfere with airflow and gas exchange, primarily including emphysema and chronic bronchitis.
Emphysema
- Characterized by the destruction of lung elastic tissue, reducing recoil ability, and leading to lung hyperinflation.
- Damaged alveoli result in air trapping, decreased gas exchange, increased work of breathing, and sensations of "air hunger."
- Common symptoms include increased CO2 retention and respiratory acidosis.
Chronic Bronchitis
- Inflammation of bronchi and bronchioles due to irritants, especially cigarette smoke.
- Causes airflow impairment through increased mucus secretion and thickening of bronchial walls.
- Contributes to chronic infection due to mucus accumulation and provides a breeding ground for pathogens.
Risk Factors
- Major risk factor for COPD is cigarette smoking.
- Genetic risk includes alpha1-antitrypsin deficiency.
- History of asthma may increase susceptibility to COPD.
Complications of COPD
- Hypoxemia and acidosis are significant concerns.
- Common complications include respiratory infections, cor pulmonale (cardiac failure due to lung disease), dysrhythmias, and respiratory failure.
Assessment of COPD
- Physical assessment should recognize signs like barrel chest, abnormal respiratory and cardiac changes.
- Laboratory assessment might include arterial blood gases (ABGs), indicating hypoxemia and hypercapnia (excess CO2).
- Monitor oxygen saturation (aim for 88-92%) and assess treatment responses.
Management Strategies
- Focus on dyspnea management through small, high-calorie meals and controlled breathing techniques (e.g., pursed-lip breathing).
- Address anxiety through counseling, relaxation techniques, and support systems.
- Encourage smoking cessation as a critical intervention for improving patient outcomes.
Health Promotion and Maintenance
- Educate patients about self-management strategies, including drug therapy and effective breathing techniques.
- Emphasize the importance of avoiding respiratory infections and achieving baseline gas exchange levels.
Evaluation of Patient Outcomes
- Goals include maintaining a stable gas exchange, an effective breathing pattern, patent airways, ideal body weight, decreased anxiety, and acceptable activity levels.
NCLEX Style Questions
- Recognize the significance of patient statements that may indicate worsening conditions (e.g., sleep positioning in COPD patients).
- Assess findings from procedures such as pneumonectomy recovery and the implications for nursing intervention.
- Understand priority actions in acute asthma management based on peak flow meter readings.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.