Podcast
Questions and Answers
Which muscle groups are commonly associated with increased tightness in cervicogenic headache patients?
Which muscle groups are commonly associated with increased tightness in cervicogenic headache patients?
- Pectoralis major and gluteus maximus
- Biceps brachii and triceps brachii
- Rectus abdominis and external obliques
- Upper trapezius and levator scapulae (correct)
What distinguishes cervicogenic headaches from migraine headaches?
What distinguishes cervicogenic headaches from migraine headaches?
- Increased frequency of unilateral symptoms
- The absence of headache pain
- Higher incidence of upper cervical joint dysfunctions (correct)
- Greater cervical range of motion
Which technique is effective for reducing cervicogenic headache symptoms?
Which technique is effective for reducing cervicogenic headache symptoms?
- Strengthening exercises for the hamstrings
- Static stretching of lower back muscles
- C1-C2 SNAG technique (correct)
- Aerobic exercise focusing on endurance
What is a common weakness observed in patients with cervicogenic headaches?
What is a common weakness observed in patients with cervicogenic headaches?
Which treatment modality is not typically used for cervicogenic headaches?
Which treatment modality is not typically used for cervicogenic headaches?
What does the performance index evaluate in muscle endurance?
What does the performance index evaluate in muscle endurance?
Which of the following is NOT considered a subjective feature of clinical cervical instability?
Which of the following is NOT considered a subjective feature of clinical cervical instability?
How do proprioception exercises benefit patients with cervical spine instability?
How do proprioception exercises benefit patients with cervical spine instability?
What is the purpose of spinal manipulation in physical therapy for cervical instability?
What is the purpose of spinal manipulation in physical therapy for cervical instability?
What does the activation score measure?
What does the activation score measure?
Which symptom is commonly associated with cervical spine instability?
Which symptom is commonly associated with cervical spine instability?
What is a common surgical intervention for severe cervical spine instability?
What is a common surgical intervention for severe cervical spine instability?
Why is improving posture important for those with cervical instability?
Why is improving posture important for those with cervical instability?
What characterizes movements occurring in the neutral zone of the spine?
What characterizes movements occurring in the neutral zone of the spine?
Which condition indicates a clinical spinal instability?
Which condition indicates a clinical spinal instability?
Which factor is NOT associated with degeneration or mechanical injury of the spinal stabilization components?
Which factor is NOT associated with degeneration or mechanical injury of the spinal stabilization components?
What are aberrant motions in the context of clinical instability?
What are aberrant motions in the context of clinical instability?
Which of the following symptoms is associated with cervical instability?
Which of the following symptoms is associated with cervical instability?
What does the Sharp-Purser test specifically assess?
What does the Sharp-Purser test specifically assess?
What should be expected during the Transverse Ligament Stress Test?
What should be expected during the Transverse Ligament Stress Test?
Which of the following symptoms is commonly reported with cervical degeneration?
Which of the following symptoms is commonly reported with cervical degeneration?
What is the primary dysfunction observed in patients with cervical hypomobility?
What is the primary dysfunction observed in patients with cervical hypomobility?
Which of the following is NOT a proposed intervention for managing cervical hypomobility?
Which of the following is NOT a proposed intervention for managing cervical hypomobility?
What percentage of cervical radiculopathy cases are typically caused by foraminal encroachment?
What percentage of cervical radiculopathy cases are typically caused by foraminal encroachment?
Which clinical examination test is used to identify cervical nerve root compression?
Which clinical examination test is used to identify cervical nerve root compression?
Which symptom is typically NOT associated with cervical radiculopathy?
Which symptom is typically NOT associated with cervical radiculopathy?
What range of motion indicates limited ipsilateral neck rotation for identifying cervical radiculopathy?
What range of motion indicates limited ipsilateral neck rotation for identifying cervical radiculopathy?
What is the common cause of cervical radiculopathy, accounting for less than 25% of cases?
What is the common cause of cervical radiculopathy, accounting for less than 25% of cases?
What is the primary focus of the pathoanatomical model in diagnosing conditions?
What is the primary focus of the pathoanatomical model in diagnosing conditions?
What is a common characteristic of patients with cervical hypomobility during motion testing?
What is a common characteristic of patients with cervical hypomobility during motion testing?
Which classification category does NOT fall under neck pain classifications?
Which classification category does NOT fall under neck pain classifications?
What does centralisation in the response to movement indicate?
What does centralisation in the response to movement indicate?
How did the treatment-based classification of neck pain evolve after the 2008 update?
How did the treatment-based classification of neck pain evolve after the 2008 update?
Which aspect is commonly assessed in the response to movement model?
Which aspect is commonly assessed in the response to movement model?
What is NOT a characteristic of the treatment-based classification system?
What is NOT a characteristic of the treatment-based classification system?
Which of the following is a treatment-oriented subgroup for acute spinal pain syndromes?
Which of the following is a treatment-oriented subgroup for acute spinal pain syndromes?
What is the intended purpose of the categorization system proposed by Werneke et al.?
What is the intended purpose of the categorization system proposed by Werneke et al.?
What is the primary focus of a cervical collar in managing cervical pain?
What is the primary focus of a cervical collar in managing cervical pain?
What is a recommended approach to help manage pain through exercise?
What is a recommended approach to help manage pain through exercise?
Which test is specifically used to assess the neuromotor control of deep flexors in the cervical spine?
Which test is specifically used to assess the neuromotor control of deep flexors in the cervical spine?
How can cervicogenic headaches be differentiated from migraines based on physical examination?
How can cervicogenic headaches be differentiated from migraines based on physical examination?
What implication does a reduced range of motion more than 10° during the CFRT suggest?
What implication does a reduced range of motion more than 10° during the CFRT suggest?
What is a key feature of the pain experienced by patients with cervicogenic headaches?
What is a key feature of the pain experienced by patients with cervicogenic headaches?
What is the estimated incidence of cervicogenic headaches among chronic headache sufferers?
What is the estimated incidence of cervicogenic headaches among chronic headache sufferers?
Which muscle group is primarily strengthened in the craniocervical flexion training?
Which muscle group is primarily strengthened in the craniocervical flexion training?
Flashcards
Clinical Condition Model
Clinical Condition Model
A medical model that focuses on identifying the specific condition based on signs and symptoms, such as cervicogenic headache.
Pathoanatomical Model
Pathoanatomical Model
A medical model that emphasizes identifying the dysfunctional structure, such as the facet joint, intervertebral disc, or myofascial tissues.
Response to Movement Model
Response to Movement Model
A model based on how movement affects symptoms, such as observing changes with repeated movements and the centralizing phenomenon.
Treatment-Based Classification
Treatment-Based Classification
Signup and view all the flashcards
Treatment-Oriented Subgroup
Treatment-Oriented Subgroup
Signup and view all the flashcards
Cervical Hypomobility
Cervical Hypomobility
Signup and view all the flashcards
Cervical Radiculopathy
Cervical Radiculopathy
Signup and view all the flashcards
Clinical Instability
Clinical Instability
Signup and view all the flashcards
Cervical Radiculopathy (CR)
Cervical Radiculopathy (CR)
Signup and view all the flashcards
Spurling's Test
Spurling's Test
Signup and view all the flashcards
Neck Distraction Test
Neck Distraction Test
Signup and view all the flashcards
Upper Limb Neurodynamic Test 1 (ULNT 1)
Upper Limb Neurodynamic Test 1 (ULNT 1)
Signup and view all the flashcards
Ipsilateral Neck Rotation
Ipsilateral Neck Rotation
Signup and view all the flashcards
Foraminal Encroachment
Foraminal Encroachment
Signup and view all the flashcards
Herniation of the Intervertebral Disc
Herniation of the Intervertebral Disc
Signup and view all the flashcards
Activation Score
Activation Score
Signup and view all the flashcards
Performance Index
Performance Index
Signup and view all the flashcards
Clinical Cervical Instability
Clinical Cervical Instability
Signup and view all the flashcards
Subjective Feature of Cervical Instability
Subjective Feature of Cervical Instability
Signup and view all the flashcards
Objective Feature of Cervical Instability
Objective Feature of Cervical Instability
Signup and view all the flashcards
Proprioception Exercises
Proprioception Exercises
Signup and view all the flashcards
Anterior Cervical Fusion
Anterior Cervical Fusion
Signup and view all the flashcards
Physical Therapy Management for Cervical Instability
Physical Therapy Management for Cervical Instability
Signup and view all the flashcards
Cervicogenic Headache
Cervicogenic Headache
Signup and view all the flashcards
Overactive Muscles in Cervicogenic Headache
Overactive Muscles in Cervicogenic Headache
Signup and view all the flashcards
Limited Cervical Range of Motion
Limited Cervical Range of Motion
Signup and view all the flashcards
Cervical Facet Joint Dysfunction
Cervical Facet Joint Dysfunction
Signup and view all the flashcards
Strengthening Exercises for Cervicogenic Headache
Strengthening Exercises for Cervicogenic Headache
Signup and view all the flashcards
Neutral Zone
Neutral Zone
Signup and view all the flashcards
Elastic Zone
Elastic Zone
Signup and view all the flashcards
Clinical Spinal Instability
Clinical Spinal Instability
Signup and view all the flashcards
Degeneration and Mechanical Injury
Degeneration and Mechanical Injury
Signup and view all the flashcards
Aberrant Motions
Aberrant Motions
Signup and view all the flashcards
Sharp-Purser Test
Sharp-Purser Test
Signup and view all the flashcards
Transverse Ligament Stress Test
Transverse Ligament Stress Test
Signup and view all the flashcards
Neck Flexor Muscle Endurance Test
Neck Flexor Muscle Endurance Test
Signup and view all the flashcards
Cranio Cervical Flexion Test (CCFT)
Cranio Cervical Flexion Test (CCFT)
Signup and view all the flashcards
Cervical Flexion-Rotation Test (CFRT)
Cervical Flexion-Rotation Test (CFRT)
Signup and view all the flashcards
Gradual Aerobic Exercise Program
Gradual Aerobic Exercise Program
Signup and view all the flashcards
Intermittent Cervical Collar Use
Intermittent Cervical Collar Use
Signup and view all the flashcards
Craniocervical Flexion Training Program
Craniocervical Flexion Training Program
Signup and view all the flashcards
Neuromotor Control of Cervical Spine
Neuromotor Control of Cervical Spine
Signup and view all the flashcards
Airbag Pressure Biofeedback Device
Airbag Pressure Biofeedback Device
Signup and view all the flashcards
Study Notes
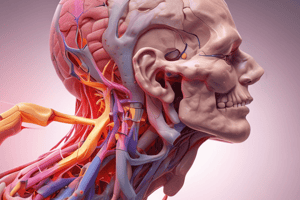
Cervical Spine Disorders
- These disorders involve the cervical vertebrae, encompassing anatomy, biomechanics, red flags, and treatment classifications.
Objectives
- Students should master the clinical anatomy related to the cervical spine.
- Students should understand the clinical biomechanics of the cervical spine.
- Students need to identify red flags associated with cervical spine issues.
- Students should understand the classification and treatment of cervical disorders.
Cervical Vertebrae Characteristics
- The transverse processes in the upper six cervical vertebrae contain a foramen (transversarium).
- Typical cervical transverse processes have anterior and posterior tubercles for muscle attachment.
- The body's superior surface projects upward, while the inferior surface is angled.
- The spinous processes are short and bifid (except the seventh).
Joints of Cervical Spine
- Craniovertebral (atlanto-occipital, atlanto-axial) joints connect the skull to the cervical spine.
- Zygapophyseal (facet) joints connect adjacent vertebrae, restricting excessive movement.
- Uncovertebral joints uniquely found in the cervical spine connect adjacent vertebrae.
Uncovertebral Joints
- These joints are located between the C3 and C7 vertebrae.
- They consist of unique processes (uncinate processes) that articulate with the level vertebra above.
- The facet joints comprise the superior and inferior articular processes of the adjacent vertebra.
Facet Joints
- In the middle and lower cervical spine (C2-C7), facet joints are in the sagittal plane, inclined upward and forward at approximately 45 degrees.
- The facet joints of C1-C2 are more horizontally aligned to facilitate greater neck mobility (roughly 50% of rotation occurs at this level).
Motions Available
- Spinal motions occur simultaneously and are coupled.
- In the cervical and upper thoracic regions, side bending is coupled with axial rotation moving in the same direction.
- In the upper cervical spine, relative rotation happens during cervical lateral flexion at the C1-C2 and occiput-C1 levels.
Ligaments of Cervical Spine
- Ligaments for the cervical and upper regions of the neck include the anterior longitudinal ligament, posterior longitudinal ligament, ligamentum flavum, interspinal ligament, and nuchal ligament.
- The transverse ligament of the atlas encloses and lubricates the dens as the atlas pivots.
- The alar ligament runs from the dens' lateral borders to the occiput—part of the upper cervical spine stabilization.
- The apical ligament runs from the dens' tip to the occiput, taut in head traction.
Vertebral Artery
- The vertebral artery provides crucial blood supply to the brain stem and cerebellum.
- Occlusion of the vertebral artery, particularly with neck extension and rotation, can cause dizziness, nystagmus, slurring of speech, and loss of consciousness.
- Testing the arteries is essential before neck traction or manipulation.
Red Flags
- This is a list of features that could indicate a serious underlying condition needing further investigation.
- Conditions listed includes cervical myelopathy, neoplastic conditions, upper cervical instability, inflammatory/systemic diseases, and vertebral artery insufficiency.
- Specific symptoms such as sensory disturbances in the hands, muscle wasting, unsteady gait, hyperreflexia, bowel and bladder disturbances, specific ages, histories of cancer, unexplained weight loss, constant pain, and night pain are among the features.
Classification Types
- Neurological or non-specific pain: categorized as having neurological involvement or mechanical pain.
- Clinical condition: based on signs and symptoms (e.g., cervicogenic headache).
- Pathoanatomical: based on the structure dysfunction (e.g., facet joint issues).
- Based on response to movement: centralisation and changes in pain location with movement.
Treatment-Based Cervical Spine Classification
- 1-Cervical hypomobility: neck pain with restricted mobility.
- 2-Cervical radiculopathy: neck pain radiating into the arm.
- 3-Clinical instability: neck pain with movement coordination issues.
- 4-Acute pain (whiplash): pain related to movement coordination impairments.
- 5-Cervicogenic headache: neck pain with headache symptoms.
Examination Findings and Interventions for Cervical Hypomobility
- Examination frequently finds restricted AROM (active range of motion) and PROM (passive range of motion), PIVM (passive intervertebral motion) testing in the cervical and upper thoracic regions.
- Interventions often include AROM exercises, muscle energy techniques, mobilization/manipulation techniques, and in subacute and chronic patients.
Cervical Radiculopathy
- A common cause is foraminal encroachment due to factors like decreased disc height and degenerative changes in the uncovertebral or zygapophysial joints.
- Herniation of the intervertebral disc contributes about 25%.
- Symptoms usually involve pain in the neck and one arm, motor/reflex changes, and may be unilaterally or bilaterally present if severe "bony spurs" are present, impinging on nerve root(s)
- If peripheral pain, weakness, or "pins and needles" symptoms exist, they tend to match dermatomal (nerve root) patterns.
Clinical Instability
- This refers to the spine's inability to maintain proper placement during physiological activities.
- This can lead to spinal cord/nerve root damage, pain, and deformity.
- The larger the neutral zone and lessened passive resistance to movement, the greater the chance of clinical instability.
- Poor posture, repetitive trauma, acute trauma, and/or cervical musculature weakness can contribute.
Acute Pain and Whiplash-Associated Disorders
- Whiplash involves sudden acceleration-deceleration forces resulting in a complex array of issues affecting muscles, joints, ligaments, discs, and nerves.
- The Quebec task force categorizes whiplash-associated disorders by clinical presentations.
Physical Examination- Related Tests
- Positive Spurling test (cervical compression test), neck distraction test, Upper limb neurodynamic test 1 (ULNT 1), and limited ipsilateral neck rotation.
- Other assessments to measure cervical instability includes Sharp-Purser test, Transverse Ligament Stress Test, Neck Flexor Muscle Endurance, and Craniocervical flexion test.
Cervicogenic Headaches
- These headaches stem from musculoskeletal dysfunction in the cervical spine (14% - 18% of chronic headache cases).
- Physical examination typically involves the CCFT for evaluating the neuromotor control of deep neck flexors (e.g., rectus capitis anterior, rectus capitis lateralis, longus colli, longus capitis)
- The CFRT (Cervical Flexion-Rotation Test) is used to assess movement impairment in the cervical spine.
- Other symptoms of cervicogenic headaches could include restricted and/or painful movement towards the affected side, unilaterally restricted range of motion of 10+ degrees versus other side, pressure on posterior neck, and muscle tension of the upper traps, SCM, and/or levator scapulae.
Physical Therapy Management
- Emphasizes proper posture, spinal manipulation, strengthening deep neck flexors, and proprioceptive exercises.
- Activity modification and aerobic exercise can assist in pain management.
- Specific types of interventions for particular presenting complaints may include using craniocervical flexion training programs, biofeedback, cervical spine manipulation or mobilization, and exercises targeting thoracic spine, postural education.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.