Podcast
Questions and Answers
What is the primary function of the atlanto-occipital joint?
What is the primary function of the atlanto-occipital joint?
- To allow for nodding movements of the head (correct)
- To allow for rotation of the head
- To allow for lateral flexion of the head
- To allow for posterior linear translation of the vertebrae
What is the primary function of the alar ligaments in the craniocervical region?
What is the primary function of the alar ligaments in the craniocervical region?
- To maintain the position of the dens
- To allow for flexion and extension of the cervical spine
- To limit rotation of the atlanto-axial joint (correct)
- To provide stability to the atlanto-occipital joint
During cervical extension, what is the primary motion occurring at the atlanto-axial joint?
During cervical extension, what is the primary motion occurring at the atlanto-axial joint?
- The atlas tilts backwards by approximately 15 degrees (correct)
- The ring-shaped atlas tilts forwards
- The occipital condyles roll backwards and slide forwards
- The superior facets slide inferiorly and posteriorly
What is the approximate range of motion for cervical rotation?
What is the approximate range of motion for cervical rotation?
What is the primary function of the facet joints in the cervical spine during lateral flexion?
What is the primary function of the facet joints in the cervical spine during lateral flexion?
How many cervical vertebrae are there in the human body?
How many cervical vertebrae are there in the human body?
Which of the following is NOT a function of the neck?
Which of the following is NOT a function of the neck?
Which of the following is NOT a cranial bone?
Which of the following is NOT a cranial bone?
Which of the following is a characteristic of a typical vertebra?
Which of the following is a characteristic of a typical vertebra?
Which curvature of the vertebral column is associated with the development of upright posture?
Which curvature of the vertebral column is associated with the development of upright posture?
What is the most common direction of disc herniation in the cervical spine?
What is the most common direction of disc herniation in the cervical spine?
Which ligament is primarily responsible for preventing hyperextension of the vertebral column?
Which ligament is primarily responsible for preventing hyperextension of the vertebral column?
Which cervical vertebral levels are most commonly affected by disc herniation?
Which cervical vertebral levels are most commonly affected by disc herniation?
What is the function of the ligamentum nuchae?
What is the function of the ligamentum nuchae?
Which ligament is located within the vertebral canal and attaches to the intervertebral discs?
Which ligament is located within the vertebral canal and attaches to the intervertebral discs?
Which ligament is located between the laminae of adjacent vertebrae and limits flexion of the vertebral column?
Which ligament is located between the laminae of adjacent vertebrae and limits flexion of the vertebral column?
Which structure connects the transverse processes of adjacent vertebrae?
Which structure connects the transverse processes of adjacent vertebrae?
What are the branches of the vertebral arteries?
What are the branches of the vertebral arteries?
Which vertebra is referred to as the 'Vertebra Prominens'?
Which vertebra is referred to as the 'Vertebra Prominens'?
What is the condition known as 'Disc Herniation'?
What is the condition known as 'Disc Herniation'?
Which joint allows for the rotation of the head on the axis?
Which joint allows for the rotation of the head on the axis?
What is the primary component of the nucleus pulposus of the intervertebral disc?
What is the primary component of the nucleus pulposus of the intervertebral disc?
Which vertebra has no body, pedicle, lamina, or spinous process?
Which vertebra has no body, pedicle, lamina, or spinous process?
What is 'Spinal Stenosis'?
What is 'Spinal Stenosis'?
What is the primary action of the Sternocleidomastoid muscle?
What is the primary action of the Sternocleidomastoid muscle?
What a function of the Semispinalis muscle?
What a function of the Semispinalis muscle?
Study Notes
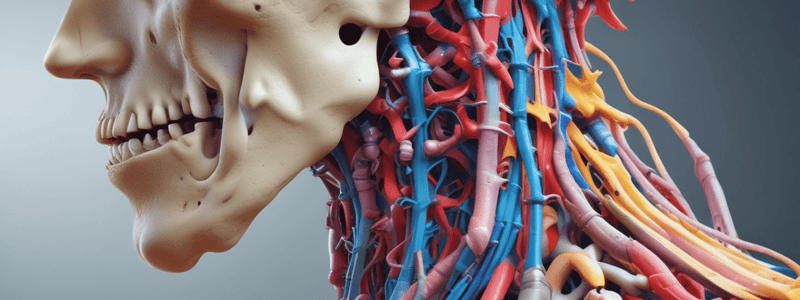
Vertebral Artery
- Right and left vertebral arteries arise from the subclavian arteries
- They ascend through the foramen transversarium
- They enter the cranial cavity via the foramen magnum
- They give off branches: meningeal, spinal, and cerebellar arteries
- They combine to form the basilar artery, which supplies the cerebellum, pons, and contributes to the circle of Willis
C1 - Atlas
- No body, pedicle, lamina, or spinous process
- Large transverse process for muscle attachment
- Ring formed by anterior and posterior arch and 2 lateral masses
- Superior articular facets articulate with occipital condyles, forming the atlanto-occipital joint
- Inferior articular facets articulate with C2 articular processes
- Dens (C2) articulates with the anterior arch, forming the atlanto-axial joint (C1/2)
- Transverse ligament between lateral masses
C2 - Axis
- The odontoid process (dens) projects superiorly to articulate with the atlas
- This articulation forms a vertical axis for rotation of the head (and atlas) on the axis, approximately 90 degrees
- Short transverse process
- Bifid spinous process
- No disc between atlas and axis
C7 - Vertebra Prominens
- Largest cervical vertebra
- Similar in shape to thoracic vertebrae
- Large non-bifid spinous process
- Clinical significance: Spinal Stenosis
Spinal Stenosis
- Narrowing of the spinal canal, reducing space for the spinal cord and associated nerves
- Causes: degenerative changes, spinal tumors, congenital conditions (Achondroplasia)
- Symptoms: extension-related radiculopathy, myelopathy
Joints of the Vertebral Column
- Intervertebral Facet or Zygapophyseal Joints
- Uncovertebral Joints (Cx)
- Atlanto-occipital/Craniovertebral Joints (Cx)
- Atlanto-axial Joints (Cx)
- Costovertebral Joints (Tx)
- Costotransverse Joints (Tx)
- Lumbosacral Joints
- Sacroiliac Joints
Intervertebral Disc (IVD)
- Endplate: Hyaline and fibrocartilage
- Diffusion of nutrients through endplate arteries
- Outer annulus fibrosus: rings of fibrocartilage (20), attaches to rims of vertebral bodies
- Inner nucleus pulposus: gelatinous (toothpaste) centre, cartilage cells, collagen fibers (Type II), semifluid ground substance – proteoglycan gel
- 60-70% water in the outer annulus, 70-90% water in the inner nucleus
Clinical - Disc Herniation
- Disc Protrusion, Prolapse, Extrusion, Sequestration
Spinal Coupling
- In the typical cervical spine, lateral flexion is coupled with ipsilateral rotation
- Due to the 45-degree inclination of articular facets
- Movement occurs in the coronal (LF) and transverse (Rot) planes simultaneously
- Note: at the craniovertebral level, a contralateral spinal coupling pattern exists
Neck Muscles
- Superficial: Anterior, Intermediate, Posterior, Lateral, Trapezius, Sternocleidomastoid, Levator Scapulae, Anterior Scalene, Splenius Cervicis/Capitis, Middle Scalene, Iliocostalis Cervicis, Posterior Scalene, Longissimus Cervicis/Capitis, Spinalis Cervicis/Capitis
- Deep: Anterior, Posterior, Longus Colli, Semispinalis, Multifidus, Longus Capitis, Rectus Capitis Posterior Major, Rectus Capitis Posterior Minor, Rectus Capitis Anterior, Rectus Capitis Lateralis, Obliquus Capitis Superior, Obliquus Capitis Inferior
Role of Muscles in the Cervical Spine
- 80% of cervical stability provided by the muscle system in mid-range and functional posture
- Deep sleeve of muscle envelops the cervical spine, providing segmental control
- High density of muscle spindles in deep muscles – sensorimotor control
- Superficial muscles have a greater role in torque production
Posterior Neck Muscles
- Superficial: Splenius Capitis and Cervicis, Iliocostalis Cervicis, Longissimus Cervicis and Capitis, Spinalis Cervicis and Capitis
- Deep: Semispinalis, Multifidus
Lateral Muscles of the Neck
- Sternocleidomastoid, Scalenes (Anterior, Middle, Posterior)
Suboccipital Muscles
- Rectus Capitis Major and Minor, Obliquus Capitis Superior and Inferior
The Triangles of the Neck
- Anterior Triangle: Borders - Superior: Mandible, Lateral: Sternocleidomastoid, Medial: Midline of neck
- Posterior Triangle: Borders - Anterior: Sternocleidomastoid, Posterior: Trapezius, Inferior: Clavicle
Clinical Conditions
- Facet Strain/Arthritis
- Spinal Stenosis
- Disc Herniation
- Myogenic Strain
- Cervical Radiculopathy
- Spinal Cord Compression
- Cervicogenic Headaches
- Cervicogenic Dizziness
- Vertebrobasilar Insufficiency (VBI)
- Craniocervical Instability
- TMJ Dysfunction
- Whiplash Associated Disorder (WAD)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the structure and function of the vertebral column, including the anatomical features, joint structures, and movement patterns in the cervical spine. Learn about vertebrae articulation, joint shapes, and the role of ligaments in maintaining stability.