Podcast
Questions and Answers
What is the recommended dose of aspirin for secondary prevention?
What is the recommended dose of aspirin for secondary prevention?
- 150 mg/day (correct)
- 75 mg/day
- 100 mg/day
- 300 mg/day
What is the treatment of choice for carotid stenosis?
What is the treatment of choice for carotid stenosis?
- Lifestyle modifications
- Surgical intervention
- Interventional (endarterectomy or stenting) (correct)
- Medical treatment
What is the typical clinical presentation of subarachnoid hemorrhage?
What is the typical clinical presentation of subarachnoid hemorrhage?
- Gradual onset of headache
- Sudden onset, severe headache (correct)
- Mild headache with nausea
- Chronic headache with no other symptoms
What is the name of the sign that is positive when the patient's neck is painful and stiff?
What is the name of the sign that is positive when the patient's neck is painful and stiff?
What is the treatment of choice for intracranial stenosis?
What is the treatment of choice for intracranial stenosis?
What is the name of the syndrome that occurs due to subarachnoid hemorrhage?
What is the name of the syndrome that occurs due to subarachnoid hemorrhage?
What is a common cause of spontaneous intracranial hemorrhage?
What is a common cause of spontaneous intracranial hemorrhage?
What is the dose of clopidogrel recommended for secondary prevention?
What is the dose of clopidogrel recommended for secondary prevention?
What is the name of the sign that is positive when the patient's leg is painful and stiff?
What is the name of the sign that is positive when the patient's leg is painful and stiff?
What is the treatment of carotid stenosis that involves opening the blocked artery?
What is the treatment of carotid stenosis that involves opening the blocked artery?
Flashcards are hidden until you start studying
Study Notes
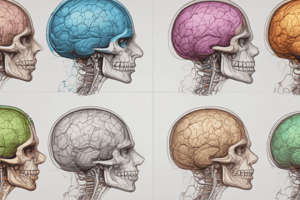
Blood Supply of the Brain
- The brain, which accounts for about 2% of the total body weight, receives 15% of the cardiac output and 25% of the total inspired air O2.
- The cerebral blood flow (CBF) is approximately 50-60 ml blood/100gm brain/minute in the vital grey matter and about 40ml blood/100g brain/minute in the white matter.
Regulation of Cerebral Blood Flow (CBF)
- Arterial CO2 tension: an increase of 1mmHg in Pa CO2 causes an immediate 5% increase in CBF.
- Arterial O2 tension: its effect is less than that of CO2.
- Blood viscosity (hematocrite): CBF is inversely related to the whole blood viscosity.
- Arterial blood pressure: CBF remains constant when the mean systemic blood pressure is between 60-160mmHg, which is known as autoregulation.
- Decrease in systemic arterial blood pressure: vasodilation occurs, leading to an increase in CBF, until exhaustion occurs, resulting in oligemia and ischemia.
- Increase in systemic blood pressure: vasoconstriction occurs, leading to a decrease in CBF, until exhaustion occurs, resulting in hyperemia and ischemia.
- In chronic hypertensive patients, the autoregulation range is shifted upwards.
- Autoregulation is impaired in: previously damaged brain, elderly, organ failure, and metabolic impairment.
Pathophysiology of Stroke
- The causes of stroke: 80% ischemic, 10% hemorrhagic, and 5% uncertain.
- Risk factors for stroke: age, sex, hypertension, diabetes mellitus, cardiac diseases, dyslipidemia, hypercoagulability, alcohol consumption, coffee, cigarettes smoking, dietary habits, drug-induced stroke, past history of TIA or mild stroke, family history of stroke, lower social class, and body built.
Clinical Features of Stroke
- Onset: usually sudden in hemorrhage, may be subacute in thrombosis, and acute or sudden in embolic.
- Course: may be regressive.
- Weakness: usually affects one half of the body, UL, LL in equal degree or one may be affected more than the other.
- Muscles tone: in acute lesions, there is a shock stage lasting for 2-6 weeks, during which there is a complete loss of tone of the paralyzed side; after this stage, tone gradually returns, and spasticity appears.
- Deep tendon reflexes in the affected limbs are exaggerated, and pathological reflexes and clonus may be elicited.
- Gait: usually circumduction.
Levels of Hemiplegia
- Cerebral
- Subcortical
- Capsular
- Brain stem
- Spinal cord
Cortical Lesions
- Usually, hemiplegia is not complete, monoplegia is more encountered.
- Cloudiness of consciousness is common.
- Contra lateral cortical sensory loss in involvement of the parietal lobe.
- Convulsions, which may be focal or secondary generalized, in cases of irritative or extensive lesions.
- Higher mental functions disorders, e.g., aphasia, agraphia, and agnosia, in lesions affected specific lobes, centers, or sites.
Subcortical Lesions
- As in cortical, but weakness is more extensive.
Capsular Lesions
- Hemiplegia is complete.
- Hemi hypothesia on the paralyzed side.
- UMN facial and hypoglossal on the same side of paralysis.
Brain Stem Lesions
- Hemiplegia is termed crossed hemiplegia, characterized by hemiplegia on the opposite of the lesion with LMN cranial nerves affection on the same side of the lesions.
Midbrain Syndromes
- Weber's syndrome: ipsilateral 3rd cranial nerve lesion, crossed hemiplegia (contralateral).
Pons Syndromes
- Millard Gubler syndrome: ipsilateral 6th, 7th cranial nerves lesion, crossed hemiplegia.
Medullary Syndromes
- Wallenberg syndrome: ipsilateral Horner's syndrome, ataxia, 9, 10, 11th cranial nerves, and decrease sensation over the face; contralateral hemianathesia.
Spinal Cord Lesions (Brown Sequard's Syndrome)
- At the level of the lesions: ipsilateral LMN weakness of muscles supplied by the affected segments, loss of reflexes mediated by the interrupted segments, and loss of sensation (radicular) in the area supplied by the diseased segments.
- Below the level of the lesion: ipsilateral hemiplegia, ipsilateral deep sensory loss, and contralateral superficial sensory loss.
Secondary Prevention
- First of all: tight control of all risk factors.
- Aspirin: for life, 150mg/day.
- Clopidogrel: for the first 3 weeks, 75mg/day.
- Oral anticoagulant: warfarin or NOAC.
- Treatment of carotid stenosis: interventional (endarterectomy or stenting).
- Treatment of intracranial stenosis: mainly medical treatment.
Cerebral Hemorrhage
- Clinical presentation: deficit plus headache or other symptoms of ICT.
- Extradural hematoma
- Subdural hematoma
- Intracerebral hematoma
- Intraventricular hematoma
- Subarachnoid hemorrhage
Subarachnoid Hemorrhage
- Clinical presentation: sudden onset, severe headache, nausea, vomiting, fever, and vertigo.
- Signs and symptoms of meningeal irritation: stiff neck, painful back, painful restricted straight leg rising sign, and positive Kerning's sign and Brudzinski signs.
- Neurological symptoms: seizures, loss of consciousness, and focal S&S may suggest intracerebral hemorrhage or local pressure.
- Terson syndrome: cranial nerves palsy, e.g., (3rd, 4th, and 6th) from local pressure.
- Causes of spontaneous intracranial hemorrhage: hypertension, amyloid angiopathy, vascular malformation, aneurysms, arteriovenous malformation, dural arteriovenous malformation, hemorrhagic blood diseases, vascular tumors, and drug-induced.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.