Podcast
Questions and Answers
What is the focus of the first topic in this course?
What is the focus of the first topic in this course?
- Renal physiology
- Digestive physiology
- Cardiovascular physiology (correct)
- Respiratory physiology
What does the electrical axis of the heart represent?
What does the electrical axis of the heart represent?
- Overall heart rate
- Endogenous pacemaker cells
- Conductivity of the heart
- Direction of electrical activity flow in the heart (correct)
What function do endogenous pacemaker cells serve in the heart?
What function do endogenous pacemaker cells serve in the heart?
- Contraction of the heart
- Production of electrical activity
- Maintenance of heart rhythm (correct)
- Regulation of blood pressure
What is the purpose of an ECG (electrocardiogram) in diagnosing heart conditions?
What is the purpose of an ECG (electrocardiogram) in diagnosing heart conditions?
Which part of the cardiovascular system is responsible for producing the familiar heartbeat pattern on an ECG?
Which part of the cardiovascular system is responsible for producing the familiar heartbeat pattern on an ECG?
How many major topics does this course cover?
How many major topics does this course cover?
What is the function of the right ventricle?
What is the function of the right ventricle?
Which septa separates the two ventricles of the heart?
Which septa separates the two ventricles of the heart?
What is the function of the left ventricle?
What is the function of the left ventricle?
Why does the right ventricle not need to pump with as much force compared to the left ventricle?
Why does the right ventricle not need to pump with as much force compared to the left ventricle?
Where is the electrical activity that causes the heart muscle to depolarize and contract generated?
Where is the electrical activity that causes the heart muscle to depolarize and contract generated?
What is the function of the internodal pathways in the heart's conduction system?
What is the function of the internodal pathways in the heart's conduction system?
What prevents electrical activity in the heart from simply going anywhere and ensures that it must go through a specific point?
What prevents electrical activity in the heart from simply going anywhere and ensures that it must go through a specific point?
What is the role of Purkinje fibers in the heart's conduction system?
What is the role of Purkinje fibers in the heart's conduction system?
How are cells within the heart electrically coupled?
How are cells within the heart electrically coupled?
What is the purpose of gap junctions in cardiac muscle cells?
What is the purpose of gap junctions in cardiac muscle cells?
Why is stretching and enlargement of cardiac muscle cells undesirable?
Why is stretching and enlargement of cardiac muscle cells undesirable?
What is the equation for cardiac output?
What is the equation for cardiac output?
What is the main function of cardiovascular regulatory systems?
What is the main function of cardiovascular regulatory systems?
Which factor primarily affects blood pressure within the circulatory system?
Which factor primarily affects blood pressure within the circulatory system?
What is the primary function of the atrioventricular valve?
What is the primary function of the atrioventricular valve?
What is the role of spirometry in respiratory physiology?
What is the role of spirometry in respiratory physiology?
What is the main topic of the next lecture after discussing respiratory physiology?
What is the main topic of the next lecture after discussing respiratory physiology?
What does alveolar ventilation look at in respiratory physiology?
What does alveolar ventilation look at in respiratory physiology?
What are the primary components of the digestive system?
What are the primary components of the digestive system?
What is the main function of the accessory organs in the digestive system?
What is the main function of the accessory organs in the digestive system?
What is the role of renal physiology in the body?
What is the role of renal physiology in the body?
What are the components involved in ventilation-perfusion matching?
What are the components involved in ventilation-perfusion matching?
What does blood-gas transport in respiratory physiology refer to?
What does blood-gas transport in respiratory physiology refer to?
What causes the large upswing in depolarization during the third phase of the cardiac action potential?
What causes the large upswing in depolarization during the third phase of the cardiac action potential?
What leads to the repolarization in the fourth phase of the cardiac action potential?
What leads to the repolarization in the fourth phase of the cardiac action potential?
What is the role of calcium channels in the plateau phase (phase 2) of the cardiac action potential?
What is the role of calcium channels in the plateau phase (phase 2) of the cardiac action potential?
What happens in phase 3 of the cardiac action potential?
What happens in phase 3 of the cardiac action potential?
What causes the large upswing in depolarization in the pacemaker potential?
What causes the large upswing in depolarization in the pacemaker potential?
What brings about repolarization in the pacemaker potential?
What brings about repolarization in the pacemaker potential?
What is the role of calcium channels in the pacemaker potential?
What is the role of calcium channels in the pacemaker potential?
What happens in phase 1 of the cardiac action potential?
What happens in phase 1 of the cardiac action potential?
How long is the cardiac action potential?
How long is the cardiac action potential?
What is the resting potential for contractile muscle cells during the cardiac action potential?
What is the resting potential for contractile muscle cells during the cardiac action potential?
What leads to the initial depolarization during phase 0 of the cardiac action potential?
What leads to the initial depolarization during phase 0 of the cardiac action potential?
What is responsible for preventing the atria from contracting while the ventricles are contracting?
What is responsible for preventing the atria from contracting while the ventricles are contracting?
What percentage of blood flow under resting conditions does the contraction of the atria account for?
What percentage of blood flow under resting conditions does the contraction of the atria account for?
What is the endogenous pacemaker of the heart?
What is the endogenous pacemaker of the heart?
What term is used to describe an area functioning as a pacemaker that is not the SA node?
What term is used to describe an area functioning as a pacemaker that is not the SA node?
What happens if the SA node fails as the pacemaker of the heart?
What happens if the SA node fails as the pacemaker of the heart?
What do modern pacemakers sense and stimulate as needed?
What do modern pacemakers sense and stimulate as needed?
What is never at rest in the pacemaker cells of the heart?
What is never at rest in the pacemaker cells of the heart?
What drives the depolarization in the first phase of the pacemaker potential?
What drives the depolarization in the first phase of the pacemaker potential?
What channels begin to open just short of the threshold level in order to trigger an action potential in the second phase of the pacemaker potential?
What channels begin to open just short of the threshold level in order to trigger an action potential in the second phase of the pacemaker potential?
Which ions are involved in driving the rest of the depolarization in cardiac pacemaker cells?
Which ions are involved in driving the rest of the depolarization in cardiac pacemaker cells?
What is implanted in the chest with two leads going into the heart through the vena cava in a modern pacemaker?
What is implanted in the chest with two leads going into the heart through the vena cava in a modern pacemaker?
What does an early implantable pacemaker stimulate the heart with?
What does an early implantable pacemaker stimulate the heart with?
Study Notes
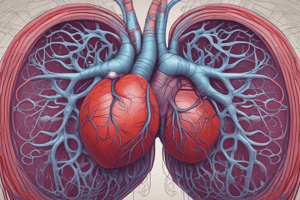
Cardiac Physiology and Electrocardiography
- The first topic of the course emphasizes the understanding of heart function and its electrical activity.
- The electrical axis of the heart indicates the overall direction of electrical activity and can help identify heart abnormalities.
- Endogenous pacemaker cells are responsible for initiating and controlling the heart's rhythmic contractions.
- An ECG (electrocardiogram) is crucial for diagnosing heart conditions by reflecting the electrical activity of the heart.
- The sinoatrial (SA) node is the part of the cardiovascular system responsible for producing the heartbeat pattern observed on an ECG.
Heart Structure and Function
- The course covers multiple major topics related to cardiovascular and respiratory physiology.
- The right ventricle pumps deoxygenated blood to the lungs for oxygenation.
- The interventricular septum separates the two ventricles of the heart.
- The left ventricle pumps oxygenated blood to the rest of the body, requiring more force than the right ventricle.
- The right ventricle does not require as much force because it pumps blood over a shorter distance (to the lungs).
Cardiac Conduction System
- Electrical activity that triggers heart muscle contraction is generated by the SA node.
- Internodal pathways facilitate the rapid conduction of electrical signals between the SA node and the atrioventricular (AV) node.
- The fibrous skeleton of the heart prevents electrical activity from spreading indiscriminately, ensuring proper signal conduction.
- Purkinje fibers play a crucial role in carrying electrical impulses to the ventricles, ensuring coordinated contraction.
Cardiac Muscle Cell Coupling
- Cardiac muscle cells are electrically coupled via gap junctions, allowing for synchronized contraction.
- Gap junctions enable direct electrical communication between cells, crucial for effective heart function.
- Excessive stretching and enlargement of cardiac muscle cells can lead to impaired function and heart failure.
Cardiac Output and Blood Pressure
- Cardiac output is calculated as heart rate multiplied by stroke volume, determining the amount of blood the heart pumps.
- Cardiovascular regulatory systems primarily function to maintain blood pressure and ensure adequate blood flow to organs.
- Blood pressure is primarily influenced by cardiac output and vascular resistance.
Heart Valves and Accessory Organs
- The primary function of the atrioventricular valve is to prevent backflow of blood from the ventricles to the atria during contraction.
- In the digestive system, accessory organs aid in digestion but are not part of the main digestive tract itself.
Respiratory and Renal Physiology
- Spirometry is used to measure lung function and capacity in respiratory physiology.
- The next lecture will build upon concepts covered in respiratory physiology, likely expanding into related systems.
- Alveolar ventilation assesses the efficiency of gas exchange in the respiratory system.
- Renal physiology regulates fluid, electrolytes, and waste product excretion.
Ventilation-Perfusion and Gas Transport
- Components involved in ventilation-perfusion matching ensure optimal gas exchange efficiency within the lungs.
- Blood-gas transport refers to how oxygen and carbon dioxide are carried in the blood.
Cardiac Action Potential Phases
- Phase 3 of the cardiac action potential is characterized by rapid depolarization, primarily caused by sodium influx.
- Repolarization in phase 4 occurs as potassium ions exit the cell.
- Calcium channels maintain the plateau phase (phase 2), allowing for sustained contraction.
- Phase 1 involves initial depolarization, followed by a rapid rising phase (phase 0) which is triggered by sodium ion influx.
Pacemaker Activity
- The endogenous pacemaker of the heart is the SA node, which sets the rhythm.
- If the SA node fails, other areas like the AV node can take over as pacemakers.
- Modern pacemakers can sense the heart’s activity and provide stimulation as needed to maintain rhythm.
- Pacemaker cells are never at rest, continuously generating electrical signals for heart function.
Modern Pacemaker Technology
- Modern pacemakers consist of a device implanted in the chest with leads entering the heart, specifically through the vena cava.
- Early implantable pacemakers provided continuous stimulation to ensure heart beats were regular.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge of the cardiovascular system anatomy with this quiz. Explore the structure and function of the heart's chambers and how blood moves through them.