Podcast
Questions and Answers
Hypertension is defined as a condition where the blood pressure is consistently above 150/100 mmHg.
Hypertension is defined as a condition where the blood pressure is consistently above 150/100 mmHg.
False (B)
Essential hypertension accounts for 90-95% of hypertension cases and has no identifiable cause.
Essential hypertension accounts for 90-95% of hypertension cases and has no identifiable cause.
True (A)
Patients with uncomplicated primary hypertension are usually symptomatic.
Patients with uncomplicated primary hypertension are usually symptomatic.
False (B)
The goal blood pressure for patients with chronic kidney disease is less than 140/90 mmHg.
The goal blood pressure for patients with chronic kidney disease is less than 140/90 mmHg.
Weight reduction for hypertension management should aim for a BMI greater than 25 kg/m².
Weight reduction for hypertension management should aim for a BMI greater than 25 kg/m².
Thiazide-type diuretics are considered a primary antihypertensive agent that is acceptable as a first-line option.
Thiazide-type diuretics are considered a primary antihypertensive agent that is acceptable as a first-line option.
β-blockers are recommended as the first-line agent for treating all patient groups with hypertension.
β-blockers are recommended as the first-line agent for treating all patient groups with hypertension.
Patients with both diabetes and hypertension should be treated with either an ACE inhibitor or a calcium channel blocker.
Patients with both diabetes and hypertension should be treated with either an ACE inhibitor or a calcium channel blocker.
Heart failure can be classified into systolic failure and myocardial failure.
Heart failure can be classified into systolic failure and myocardial failure.
The most suitable drug choice for use in pregnancy for treating hypertension is methyldopa.
The most suitable drug choice for use in pregnancy for treating hypertension is methyldopa.
Exertional dyspnea occurs when patients experience breathlessness due to physical inactivity.
Exertional dyspnea occurs when patients experience breathlessness due to physical inactivity.
Orthopnea is a condition where a patient has difficulty breathing while lying flat.
Orthopnea is a condition where a patient has difficulty breathing while lying flat.
Paroxysmal nocturnal dyspnea (PND) involves patients waking up gasping for breath.
Paroxysmal nocturnal dyspnea (PND) involves patients waking up gasping for breath.
Right-sided heart failure causes fluid retention and edema that is most significant in the upper body.
Right-sided heart failure causes fluid retention and edema that is most significant in the upper body.
Dietary modifications in heart failure patients typically recommend a salt intake of 5-6 g per day.
Dietary modifications in heart failure patients typically recommend a salt intake of 5-6 g per day.
Flashcards
Hypertension definition
Hypertension definition
High blood pressure consistently above 140/90 mmHg.
Essential vs. Secondary HTN
Essential vs. Secondary HTN
Essential HTN has no known cause; secondary HTN has a specific cause.
Hypertensive crisis BP level
Hypertensive crisis BP level
BP values significantly elevated, greater than 180/120 mm Hg.
Goal blood pressure (uncomplicated)
Goal blood pressure (uncomplicated)
Signup and view all the flashcards
Low sodium diet for HTN
Low sodium diet for HTN
Signup and view all the flashcards
First-line antihypertensive agents
First-line antihypertensive agents
Signup and view all the flashcards
Hypertension treatment in diabetics
Hypertension treatment in diabetics
Signup and view all the flashcards
Preferred diuretic for hypertension
Preferred diuretic for hypertension
Signup and view all the flashcards
Hypertension treatment in pregnancy
Hypertension treatment in pregnancy
Signup and view all the flashcards
Heart Failure Definition
Heart Failure Definition
Signup and view all the flashcards
Exertional dyspnea
Exertional dyspnea
Signup and view all the flashcards
Orthopnea
Orthopnea
Signup and view all the flashcards
Paroxysmal Nocturnal Dyspnea (PND)
Paroxysmal Nocturnal Dyspnea (PND)
Signup and view all the flashcards
Heart Failure Symptoms' Classification
Heart Failure Symptoms' Classification
Signup and view all the flashcards
Echocardiogram
Echocardiogram
Signup and view all the flashcards
Study Notes
Cardiovascular Disease
- Hypertension (HTN) is a condition where blood pressure (BP) is consistently above 140/90 mmHg.
- Essential hypertension affects 90-95% of hypertensive patients; it has no identifiable cause.
- Secondary hypertension has a specific identified cause for elevated BP.
- Hypertensive crises involve markedly elevated BP (>180/120 mmHg).
Clinical Presentation and Complications
- Uncomplicated primary hypertension is usually asymptomatic.
- Common complications include stroke and myocardial infarction.
- Diagnosis is made after averaging two or more BP measurements taken on separate occasions.
Treatment and Desired Outcome
- Goal blood pressure values are less than 140/90 mmHg for uncomplicated hypertension and less than 130/80 mmHg for patients with chronic kidney disease, coronary artery disease, or stroke (myocardial infarction [MI] or angina).
- People with diabetes and hypertension should be treated to a systolic blood pressure (SBP) goal of <140 mmHg. Lower systolic targets (<130 mmHg) may be appropriate for younger patients. Patients with diabetes should be treated to a diastolic blood pressure (DBP) <80 mmHg.
- Nonpharmacological therapy includes weight reduction (BMI < 25 kg/m²), a low-fat and low-sodium diet, regular exercise (at least 30 minutes per day), and smoking cessation.
Pharmacologic Therapy
- Initial drug selection depends on BP elevation and comorbid conditions.
- Acceptable first-line options include thiazide-type diuretics, ACE inhibitors, ARBs, and calcium channel blockers (CCBs).
- Beta-blockers are generally not recommended as first-line agents unless there's a compelling indication.
- ACE inhibitors or ARBs are the recommended treatment for patients with diabetes and hypertension.
Thiazides and Other Diuretics
- Thiazides are the preferred type of diuretic for treating hypertension.
- Loop diuretics are effective only in cases of significantly impaired renal function and are a suitable choice if heart failure is present.
- Methyldopa is suitable for use in pregnancy.
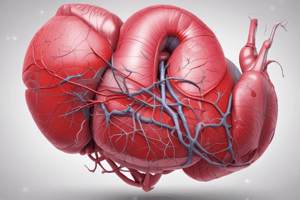
Heart Failure
- Heart failure (HF) is a condition where the heart cannot pump sufficient blood to meet the body's metabolic needs.
- Systolic failure involves decreased ejection of blood during systole; diastolic failure involves reduced ventricular filling during diastole.
- Common causes include coronary artery disease and hypertension.
Clinical Manifestations of Heart Failure
- Left-sided failure causes pulmonary congestion and edema (shortness of breath, exertional dyspnea, orthopnea, nocturnal dyspnea).
- Right-sided failure causes systemic congestion and edema (especially in the legs).
Investigations for Heart Failure
- Echocardiogram is used to assess left ventricle (LV) size and ejection fraction (EF).
- Chest X-ray helps detect cardiac enlargement and pulmonary edema.
- ECG assesses other cardiac problems, such as arrhythmias.
Nonpharmacological Interventions for Heart Failure
- Dietary modifications involve sodium restriction and sometimes fluid restriction.
- Aerobic exercise is encouraged when patients are stable, while heavy weight training is not.
- Modifying classic risk factors (tobacco and alcohol consumption) is important to minimize the potential for further damage.
Pharmacologic Treatment of Heart Failure
- ACE inhibitors, ARBs, beta-blockers, aldosterone antagonists, and the combination of angiotensin-receptor/neprilysin inhibitors (ARNIs) are effective for specific symptoms and disease progression.
- Neprilysin inhibitors increase the availability of natriuretic peptides improving heart function.
- Loop diuretics (furosemide, bumetanide, torsemide) are commonly used for fluid retention.
- Nitrates and hydralazine can be used for persistent symptoms despite other treatments.
Digoxin in Heart Failure
- Digoxin provides symptomatic benefits but does NOT improve survival.
- It is often added for patients who remain symptomatic despite optimal HF regimen (ACE inhibitor or ARB, beta-blocker, and diuretic).
- Consideration of Digoxin is for patients with atrial fibrillation.
- Recent research suggests limited benefit from digoxin for mild to moderate diastolic HF for symptom and heart rate control.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.