Podcast
Questions and Answers
What is the primary mechanism of action of calcium channel blockers?
What is the primary mechanism of action of calcium channel blockers?
- Increasing the contraction of cardiac muscle
- Enhancing the contraction of vascular smooth muscle
- Blocking the influx of calcium ions into vascular smooth muscle cells and cardiac cells (correct)
- Reducing the frequency of the heart's contractions
What is a common adverse effect of calcium channel blockers?
What is a common adverse effect of calcium channel blockers?
- Increased peripheral resistance
- Dizziness or lightheadedness (correct)
- Tachycardia
- Hypertension
What is a rare but serious adverse effect of calcium channel blockers?
What is a rare but serious adverse effect of calcium channel blockers?
- Angioedema (correct)
- Bradycardia
- Peripheral vasoconstriction
- Hypertension
What is the effect of calcium channel blockers on cardiac muscle?
What is the effect of calcium channel blockers on cardiac muscle?
What is a less common adverse effect of calcium channel blockers?
What is a less common adverse effect of calcium channel blockers?
What is the overall effect of calcium channel blockers on blood pressure?
What is the overall effect of calcium channel blockers on blood pressure?
Which type of calcium channels do calcium channel blockers primarily block?
Which type of calcium channels do calcium channel blockers primarily block?
What is a common adverse effect of dihydropyridine calcium channel blockers?
What is a common adverse effect of dihydropyridine calcium channel blockers?
Which class of calcium channel blockers is least commonly used?
Which class of calcium channel blockers is least commonly used?
What is a therapeutic indication for calcium channel blockers besides hypertension?
What is a therapeutic indication for calcium channel blockers besides hypertension?
What is the primary enzyme responsible for metabolizing calcium channel blockers?
What is the primary enzyme responsible for metabolizing calcium channel blockers?
What is the effect of calcium channel blockers on vasodilation?
What is the effect of calcium channel blockers on vasodilation?
What is the range of elimination half-life for calcium channel blockers?
What is the range of elimination half-life for calcium channel blockers?
Flashcards are hidden until you start studying
Study Notes
Calcium Channel Blockers
Mechanism of Action
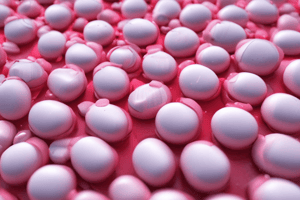
- Calcium channel blockers (CCBs) work by blocking the influx of calcium ions into vascular smooth muscle cells and cardiac cells
- This leads to:
- Relaxation of vascular smooth muscle, causing vasodilation
- Decreased peripheral resistance
- Decreased blood pressure
- CCBs also:
- Inhibit the contraction of cardiac muscle, reducing cardiac output
- Decrease the frequency of the heart's contractions
- The combined effect is a decrease in blood pressure and a reduction in the workload on the heart
Adverse Effects
- Common adverse effects:
- Dizziness or lightheadedness due to vasodilation
- Headache
- Flushing
- Peripheral edema (swelling of the legs and ankles)
- Less common adverse effects:
- Bradycardia (slow heart rate)
- Hypotension (low blood pressure)
- Gastrointestinal disturbances (nausea, vomiting, diarrhea)
- Rare but serious adverse effects:
- Angioedema (severe allergic reaction)
- Stevens-Johnson syndrome (severe skin and mucous membrane disorder)
- Heart block (impaired heart rhythm)
Calcium Channel Blockers
Mechanism of Action
- Block influx of calcium ions into vascular smooth muscle cells and cardiac cells
- Result in relaxation of vascular smooth muscle, causing vasodilation
- Decrease peripheral resistance
- Decrease blood pressure
- Inhibit contraction of cardiac muscle, reducing cardiac output
- Decrease frequency of heart's contractions
- Combined effect: decrease in blood pressure and reduction in heart's workload
Adverse Effects
- Common:
- Dizziness or lightheadedness due to vasodilation
- Headache
- Flushing
- Peripheral edema
- Less common:
- Bradycardia
- Hypotension
- Gastrointestinal disturbances
- Rare but serious:
- Angioedema
- Stevens-Johnson syndrome
- Heart block
Calcium Channel Blockers (CCBs)
Mechanism of Action
- Inhibit influx of calcium ions into vascular smooth muscle cells and cardiac myocytes to reduce muscle contraction and vasodilation
- Block L-type calcium channels to decrease contraction force of the heart and lower blood pressure
Adverse Effects
- Common: headache, dizziness, flushing, peripheral edema
- Less common: bradycardia, AV block, hypotension, constipation
- Rare: allergic reactions, Stevens-Johnson syndrome, lupus-like syndrome
Classes of CCBs
Dihydropyridines (DHPs)
- Most commonly used CCBs
- Examples: nifedipine, amlodipine, felodipine
Phenylalkylamines
- Less commonly used CCBs
- Examples: verapamil, gallopamil
Benzothiazepines
- Less commonly used CCBs
- Examples: diltiazem, clentiazem
Therapeutic Indications
- Hypertension (primary indication)
- Angina pectoris
- Supraventricular tachyarrhythmias (PSVT, atrial fibrillation)
- Raynaud's phenomenon
- Migraine prophylaxis
Pharmacokinetics
- Well absorbed from the GI tract, with varying bioavailability among CCBs
- High protein binding (90-98%)
- Metabolized by the liver via CYP3A4
- Elimination half-life: 2-12 hours, depending on the CCB
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.