Podcast
Questions and Answers
What is the primary function of buffer systems in the human body?
What is the primary function of buffer systems in the human body?
- To neutralize acids and bases, maintaining pH balance (correct)
- To generate excess acids in the bloodstream
- To increase the concentration of hydrogen ions
- To facilitate respiration and increase oxygen levels
Which buffer system maintains a normal ratio of carbonic acid to bicarbonate?
Which buffer system maintains a normal ratio of carbonic acid to bicarbonate?
- Phosphate buffer system
- Protein buffer system
- Bicarbonate buffer system (correct)
- Ammonia buffer system
What generally indicates acidosis in the body?
What generally indicates acidosis in the body?
- A pH balance of 7.45 or higher
- An accumulation of hydrogen ions or loss of bicarbonate (correct)
- A loss of carbon dioxide
- A maintained ratio of bicarbonate to carbonic acid
How do the lungs and kidneys collaborate in regulating acid-base balance?
How do the lungs and kidneys collaborate in regulating acid-base balance?
Which of the following correctly defines a buffer?
Which of the following correctly defines a buffer?
What happens to blood pH when the ratio of carbonic acid to bicarbonate is maintained?
What happens to blood pH when the ratio of carbonic acid to bicarbonate is maintained?
Which of the following conditions results from an accumulation of bicarbonate in the blood?
Which of the following conditions results from an accumulation of bicarbonate in the blood?
During an ABG test, which substances are primarily measured?
During an ABG test, which substances are primarily measured?
What indicates alkalosis in the body?
What indicates alkalosis in the body?
What is expected when small amounts of an acid or base are added to a buffer solution?
What is expected when small amounts of an acid or base are added to a buffer solution?
What is the primary function of the bicarbonate buffer system in the body?
What is the primary function of the bicarbonate buffer system in the body?
What occurs to the respiratory rate during hyperventilation?
What occurs to the respiratory rate during hyperventilation?
In the kidneys, what is primarily conserved during acidosis?
In the kidneys, what is primarily conserved during acidosis?
Which of the following correctly describes the phosphate buffer system?
Which of the following correctly describes the phosphate buffer system?
What role do proteins play in the protein buffer system?
What role do proteins play in the protein buffer system?
Which of the following is NOT a characteristic of the bicarbonate buffer system?
Which of the following is NOT a characteristic of the bicarbonate buffer system?
What happens to pH during hypoventilation?
What happens to pH during hypoventilation?
Which two processes are primarily managed by the kidneys in acid-base regulation?
Which two processes are primarily managed by the kidneys in acid-base regulation?
What effect does an increase in respiratory rate have on CO2 levels?
What effect does an increase in respiratory rate have on CO2 levels?
What is the effect of dihydrogen phosphate in the phosphate buffer system?
What is the effect of dihydrogen phosphate in the phosphate buffer system?
What is the primary cause of respiratory acidosis?
What is the primary cause of respiratory acidosis?
Which of the following symptoms is commonly associated with respiratory acidosis?
Which of the following symptoms is commonly associated with respiratory acidosis?
What condition is characterized by a low blood pH due to excess acid in the body?
What condition is characterized by a low blood pH due to excess acid in the body?
What compensatory mechanism occurs during metabolic acidosis?
What compensatory mechanism occurs during metabolic acidosis?
Which statement correctly describes respiratory alkalosis?
Which statement correctly describes respiratory alkalosis?
How does metabolic alkalosis typically occur?
How does metabolic alkalosis typically occur?
Which electrolyte disturbance can occur with respiratory alkalosis?
Which electrolyte disturbance can occur with respiratory alkalosis?
What best describes the role of proteins in acid-base balance?
What best describes the role of proteins in acid-base balance?
What is a common outcome of impaired ventilation in respiratory acidosis?
What is a common outcome of impaired ventilation in respiratory acidosis?
What can contribute to respiratory alkalosis aside from hyperventilation?
What can contribute to respiratory alkalosis aside from hyperventilation?
In metabolic acidosis, what is the primary physiological response?
In metabolic acidosis, what is the primary physiological response?
Which condition primarily results from respiratory depression?
Which condition primarily results from respiratory depression?
What is a potential consequence of chronic respiratory acidosis on the cardiovascular system?
What is a potential consequence of chronic respiratory acidosis on the cardiovascular system?
Flashcards are hidden until you start studying
Study Notes
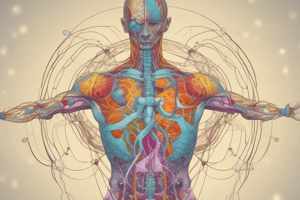
Buffer Systems and Acid-Base Balance
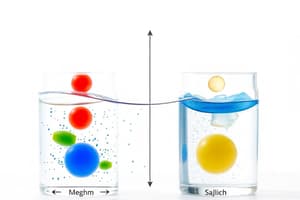
- Buffer systems resist changes in pH, essential for maintaining a stable internal environment.
- Chemical Buffer Systems work by neutralizing excess acids or bases. These systems react with acids and bases to prevent significant changes in pH.
- Physiological Buffer Systems include the lungs and kidneys which play a crucial role in regulating acid-base balance.
Major Buffer Systems in the Body
- Bicarbonate Buffer System is the primary buffer system.
- Lungs regulate carbonic acid (H2CO3) production by managing CO2 levels.
- Kidneys regulate bicarbonate (HCO3-) production.
- Lungs control CO2 content in the extracellular fluid (ECF) by adjusting ventilation.
- Increased CO2 leads to hyperventilation (increased respiratory rate).
- Reduced CO2 leads to hypoventilation (decreased respiratory rate).
- Kidneys regulate HCO3- in the ECF by either reabsorbing or excreting acids and bases into urine.
- Acidosis stimulates kidney excretion of H+ and conservation of HCO3-.
- Alkalosis causes the kidneys to retain H+ and excrete HCO3-.
- Phosphate Buffer System is essential for regulating pH in intracellular fluid (ICF) and urine.
- Consists of mono and dihydrogen phosphate ions (HPO₄²⁻/H₂PO₄⁻).
- Neutralizes excess acid by reacting with monohydrogen phosphate, increasing dihydrogen phosphate.
- Neutralizes excess base by reacting with dihydrogen phosphate, increasing monohydrogen phosphate.
- Protein Buffer System helps regulate pH in both ECF and ICF.
- Proteins are chains of amino acids containing amine (– NH2) and carboxyl (–COOH) groups.
- Amine groups (NH2) bind to excess H+ (acid) in the blood.
- Carboxyl groups (COOH) release H+ (acid) in the blood to combat excess base.
Acid-Base Imbalance
- Acidosis occurs when pH is below 7.35, meaning there is an accumulation of acids or loss of bases (HCO3-).
- Alkalosis occurs when pH is above 7.35, indicating an accumulation of bases or loss of acids.
Respiratory Acidosis:
- Occurs when the lungs cannot remove enough CO2 from the body leading to CO2 accumulation in the blood, causing a low pH.
- Caused by:
- Respiratory center depression (hypoventilation)
- COPD
- Narcotics
- Respiratory arrest
- Paralysis of respiratory muscles
- Causes:
- Decreased excitability of the central nervous system (CNS)
- Headache, drowsiness, disorientation, coma
- Cardiovascular issues: dysrhythmias, decreased cardiac contractility, hypotension.
- Hypercalcemia: acidosis decreases Ca++ binding to albumin, increasing serum ionized Ca++ levels.
Metabolic Acidosis:
- Caused by loss of bicarbonate or an increase in acid generation.
- Symptoms resemble respiratory acidosis, but the primary cause is HCO3 loss.
Respiratory Alkalosis:
- Caused by a decrease in CO2 levels in the blood due to hyperventilation (increased excretion by the lungs).
- Caused by:
- Hyperventilation
- Hypoxemia (low blood oxygen)
- Fever
- Anger
- Psychological dyspnea: anxiety-induced hyperventilation, experiencing shortness of breath
- Causes:
- Increased excitability of the CNS
- Lightheadedness, numbness, tingling, confusion, blurred vision
- Cardiovascular issues: increased cardiac contractility, hypertension
- Hypokalemia: increased blood pH causes shift of K out of plasma and interstitial fluids into urine.
Metabolic Alkalosis
- Characterized by an accumulation of bicarbonate in the body.
- Most commonly caused by loss of stomach acid due to excessive vomiting.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.