Podcast
Questions and Answers
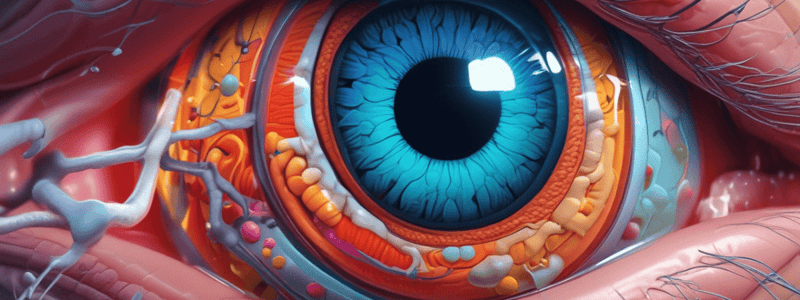
What eye structure extends into the sclera and covers the posterior region of the eye?
What eye structure extends into the sclera and covers the posterior region of the eye?
- Choroid
- Cornea (correct)
- Ciliary body
- Conjunctiva
Which eye structure contains blood vessels that nourish the retina?
Which eye structure contains blood vessels that nourish the retina?
- Ciliary muscle
- Choroid (correct)
- Conjunctiva
- Sclera
What is responsible for flattening and rounding the lens in the eye so that it can see near and far?
What is responsible for flattening and rounding the lens in the eye so that it can see near and far?
- Optic disc
- Ciliary muscle (correct)
- Iris
- Retina
What eye structure is known as the thin pigmented layer of smooth muscle unique to each person?
What eye structure is known as the thin pigmented layer of smooth muscle unique to each person?
Which part of the eye changes the amount of light entering by dilating and contracting?
Which part of the eye changes the amount of light entering by dilating and contracting?
Where in the eye is the blind spot located?
Where in the eye is the blind spot located?
What is the receptor-containing portion of the retina that is an extension of the CNS?
What is the receptor-containing portion of the retina that is an extension of the CNS?
What is the main function of CN2 (Optic Nerve) according to the text?
What is the main function of CN2 (Optic Nerve) according to the text?
Which area of the eye has the highest concentration of cones?
Which area of the eye has the highest concentration of cones?
What is the clinical defect associated with macular degeneration, as per the text?
What is the clinical defect associated with macular degeneration, as per the text?
Where is aqueous humor formed in the eye?
Where is aqueous humor formed in the eye?
Which part of the eye surrounds the fovea centralis and has fairly high acuity?
Which part of the eye surrounds the fovea centralis and has fairly high acuity?
What is the main role of the canal of Schlemm in the eye?
What is the main role of the canal of Schlemm in the eye?
Which part of the eye is associated with blindness when affected by macular degeneration?
Which part of the eye is associated with blindness when affected by macular degeneration?
What is the role of the brain's built-in analgesic system?
What is the role of the brain's built-in analgesic system?
Which of the following is NOT an endogenous opiate involved in the analgesic pathway?
Which of the following is NOT an endogenous opiate involved in the analgesic pathway?
What is the function of vitreous humor in the eye?
What is the function of vitreous humor in the eye?
Where is the anterior cavity located in the eye?
Where is the anterior cavity located in the eye?
What defect is associated with an inability of the aqueous humor to drain properly?
What defect is associated with an inability of the aqueous humor to drain properly?
Which fluid-filled cavity in the eye contains vitreous humor?
Which fluid-filled cavity in the eye contains vitreous humor?
What substance is made at a rate of approximately 5ml per day in the eye?
What substance is made at a rate of approximately 5ml per day in the eye?
What is the age-related reduction in accommodation ability known as?
What is the age-related reduction in accommodation ability known as?
Which type of lens is needed to correct hyperopia?
Which type of lens is needed to correct hyperopia?
What condition results from the uneven curvature of the cornea?
What condition results from the uneven curvature of the cornea?
Which photoreceptor is responsible for night vision?
Which photoreceptor is responsible for night vision?
What deficiency leads to night blindness associated with rods?
What deficiency leads to night blindness associated with rods?
What is the name of the pigment found in the discs of rods?
What is the name of the pigment found in the discs of rods?
Which type of vision is primarily associated with cones?
Which type of vision is primarily associated with cones?
Which part of the photopigment absorbs light?
Which part of the photopigment absorbs light?
What is the main function of the opsin protein in the disc membrane?
What is the main function of the opsin protein in the disc membrane?
Which adaptation allows gradual distinction of objects when entering a dark area?
Which adaptation allows gradual distinction of objects when entering a dark area?
What leads to the breakdown of cyclic guanosine monophosphate (cGMP) during light adaptation?
What leads to the breakdown of cyclic guanosine monophosphate (cGMP) during light adaptation?
What is the role of G-proteins (transducin) in the phototransduction process?
What is the role of G-proteins (transducin) in the phototransduction process?
Which pathway does the optic nerve (CN2) follow after leaving the ganglion cells?
Which pathway does the optic nerve (CN2) follow after leaving the ganglion cells?
During dark adaptation, what enables the gradual distinction of objects in a dark area?
During dark adaptation, what enables the gradual distinction of objects in a dark area?
What happens to the I bands during muscle contraction?
What happens to the I bands during muscle contraction?
In muscle relaxation, what enzyme breaks down Acetylcholine at the neuromuscular junction?
In muscle relaxation, what enzyme breaks down Acetylcholine at the neuromuscular junction?
What is the primary cause of Rigor Mortis?
What is the primary cause of Rigor Mortis?
During muscle contractions, what is the role of ATP?
During muscle contractions, what is the role of ATP?
What happens to the Z line during muscle contraction?
What happens to the Z line during muscle contraction?
Which molecule is responsible for muscle relaxation by breaking down ACh at the neuromuscular junction?
Which molecule is responsible for muscle relaxation by breaking down ACh at the neuromuscular junction?
What is the consequence of continuous binding of Calcium ions during muscle relaxation?
What is the consequence of continuous binding of Calcium ions during muscle relaxation?
Which event occurs as a result of the removal of Acetylcholine at the neuromuscular junction?
Which event occurs as a result of the removal of Acetylcholine at the neuromuscular junction?
'Twitch' in muscle contractions is characterized by:
'Twitch' in muscle contractions is characterized by:
In muscle contractions, which enzyme breaks down ATP into ADP + P?
In muscle contractions, which enzyme breaks down ATP into ADP + P?
What type of muscle fibers fatigue less and are rich in red color?
What type of muscle fibers fatigue less and are rich in red color?
In muscle contraction, what provides the energy for the power stroke of the cross bridge?
In muscle contraction, what provides the energy for the power stroke of the cross bridge?
What causes muscle fatigue when the exercising muscle can no longer respond to stimulation with the same degree of contractile activity?
What causes muscle fatigue when the exercising muscle can no longer respond to stimulation with the same degree of contractile activity?
What is the main function of the Golgi Tendon Muscle?
What is the main function of the Golgi Tendon Muscle?
What is the mechanism of action that creates a more globular structure in smooth muscle cells?
What is the mechanism of action that creates a more globular structure in smooth muscle cells?
Which type of muscle fibers stop at glycolysis and are anaerobic?
Which type of muscle fibers stop at glycolysis and are anaerobic?
What does the lack of myoglobin in white muscle fibers result in?
What does the lack of myoglobin in white muscle fibers result in?
Which neurons bring messages from peripheral receptors to the CNS?
Which neurons bring messages from peripheral receptors to the CNS?
What is the role of the Gamma Motor Neuron in muscle spindles?
What is the role of the Gamma Motor Neuron in muscle spindles?
During which phase of muscle relaxation is Ca2+ actively transported back into the sarcoplasmic reticulum?
During which phase of muscle relaxation is Ca2+ actively transported back into the sarcoplasmic reticulum?
What is the primary structural component of thin filaments in muscle cells?
What is the primary structural component of thin filaments in muscle cells?
Which protein binds to calcium ions to expose the actin binding site for the crossbridge formation during muscle contraction?
Which protein binds to calcium ions to expose the actin binding site for the crossbridge formation during muscle contraction?
What is the rope-like molecule that stabilizes the thick filament in muscle cells?
What is the rope-like molecule that stabilizes the thick filament in muscle cells?
Which structure brings the action potential deep into the interior of a muscle fiber?
Which structure brings the action potential deep into the interior of a muscle fiber?
What stores calcium in the lateral sacs called Terminal Cisternae in muscle cells?
What stores calcium in the lateral sacs called Terminal Cisternae in muscle cells?
Which region of the sarcomere contains only myosin tails?
Which region of the sarcomere contains only myosin tails?
What is the primary role of ATP in muscle relaxation?
What is the primary role of ATP in muscle relaxation?
During rigor mortis, what process prevents myosin from detaching from actin?
During rigor mortis, what process prevents myosin from detaching from actin?
What is the consequence of elevated levels of calcium ions in sarcomeres during muscle contraction?
What is the consequence of elevated levels of calcium ions in sarcomeres during muscle contraction?
Which protein attaches the entire muscle unit to the sarcolemma in muscles?
Which protein attaches the entire muscle unit to the sarcolemma in muscles?
Flashcards are hidden until you start studying
Study Notes
Muscle Fibers
- Slow-Oxidative (Type 1) Fibers:
- Break down ATP slowly
- Releases calcium ions slowly
- Frequently used muscle fibers for daily activities (e.g., walking, standing, posture)
- Fast-Oxidative (Type 2a) Fibers:
- Break down ATP faster than slow-oxidative fibers
- Releases calcium ions faster than slow-oxidative fibers
- Used occasionally for activities requiring rapid contractions (e.g., playing the piano, violin)
Muscle Contraction
- Twitch:
- Brief, weak contraction
- Produced by a single action potential
- Too short and weak to be useful
- Twitch Summation:
- Results from sustained elevation of cytosolic calcium
- Leads to tetanus
- Tetanus:
- Sustained contractile activity
- Occurs when muscle fiber is stimulated rapidly, not allowing relaxation between stimuli
Muscle Unit
- Motor Unit:
- One motor neuron and the muscle fibers it innervates
- Function together to produce muscle contraction
Muscle Tension
- Length-Tension Relationship:
- Optimum length (L0) allows for most cross-bridges to form, producing maximum strength
- Muscle typically attached to at least two different bones across a joint
- Origin: end of the muscle attached to the stationary part of the skeleton
- Insertion: end of the muscle attached to the skeletal part that moves
Types of Contractions
- Isotonic (Equal Stretch) Contractions:
- Creates force and movement
- Concentric contractions: muscle shortening (e.g., bicep curl)
- Eccentric contractions: muscle lengthening (e.g., extension of the arm)
- Isometric (Equal Measurement) Contractions:
- Creates force but no movement
- Examples: yoga, plank formation, pilates
Energy Sources for Contraction
- Three main sources of energy:
- Transfer of high-energy phosphate from creatine phosphate to ADP
- Glycolysis: breakdown of glucose to create ATP
- Oxidative phosphorylation (citric acid cycle and electron transport system)
Muscle Spindle Structure
- Collections of specialized muscle fibers:
- Intrafusal fibers
- Lie within spindle-shaped connective tissue capsules parallel to extrafusal fibers
- Each spindle has its own private efferent and afferent nerve supply
- Play a key role in stretch reflex
Golgi Tendon Muscle
- Type of muscle receptor:
- Monitors the force/tension we create
- Found close to the muscle fiber
- Has a connective tissue capsule with collagen fibers of great tensile strength
- Helps protect the muscle from excessive injury by allowing relaxation
Neuromuscular Junction
- Role of ATP:
- ATP goes through a degradation process and is broken down into ADP + P
- Phosphate is released during the stroke
- ADP is released after the stroke
- Relaxation:
- Acetylcholinesterase breaks down ACh at neuromuscular junction
- ACh is removed, stopping the action potential in the neuromuscular junction
- Calcium ions move back into the sarcoplasmic reticulum using the calcium-ATPase pump
- Tropomyosin is turned "off," and the cross-bridge stops
Rigor Mortis
- Stiffness upon death:
- No metabolism of ATP occurs
- Calcium cannot be released, remaining bound in the lateral sac
- Leads to muscle stiffness when calcium cannot be released
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.