Podcast
Questions and Answers
What is the primary cell type found in bone tissue?
What is the primary cell type found in bone tissue?
- Osteocytes (correct)
- Osteoblasts
- Osteoclasts
- Chondrocytes
What does osteoid refer to in bone?
What does osteoid refer to in bone?
- The outer layer of bone
- The fatty tissue in bone marrow
- The mineralized part of bone
- The matrix of the bone that contains proteoglycans and glycoproteins (correct)
Which component is primarily responsible for the tensile strength of bone?
Which component is primarily responsible for the tensile strength of bone?
- Hydroxyapatite
- Bone marrow
- Osteocytes
- Collagen fibers (correct)
What is the role of collagen fibers in bone tissue?
What is the role of collagen fibers in bone tissue?
Which property of bone is attributed to the bonds between collagen fibers?
Which property of bone is attributed to the bonds between collagen fibers?
When collagen fibers break due to impact, what is the primary benefit?
When collagen fibers break due to impact, what is the primary benefit?
What is the primary inorganic component of bone?
What is the primary inorganic component of bone?
Approximately what percentage of bone's volume is made up of mineral salts?
Approximately what percentage of bone's volume is made up of mineral salts?
What percentage of bone is made up of mineral salts?
What percentage of bone is made up of mineral salts?
What is the primary contribution of mineral salts to the properties of bone?
What is the primary contribution of mineral salts to the properties of bone?
Which component do mineral salts crystallize around in bone?
Which component do mineral salts crystallize around in bone?
Which statement accurately describes the inorganic components of bone?
Which statement accurately describes the inorganic components of bone?
What role does calcium phosphate have in maintaining bone health?
What role does calcium phosphate have in maintaining bone health?
Which statement best describes osteoporosis in relation to bone's organic components?
Which statement best describes osteoporosis in relation to bone's organic components?
What role do osteoclasts play in bone health?
What role do osteoclasts play in bone health?
What is the effect of collagen's arrangement on bone tissue?
What is the effect of collagen's arrangement on bone tissue?
Which statement best describes the role of the mineral component in bone?
Which statement best describes the role of the mineral component in bone?
How do proteoglycans and glycoproteins influence bone functionality?
How do proteoglycans and glycoproteins influence bone functionality?
Which process facilitates the healing of bone after an injury?
Which process facilitates the healing of bone after an injury?
What role does energy dissipation play in bone's response to impact?
What role does energy dissipation play in bone's response to impact?
What percentage of bone's weight is primarily attributed to inorganic components?
What percentage of bone's weight is primarily attributed to inorganic components?
Which cell type plays a key role in the formation of new bone by secreting bone matrix?
Which cell type plays a key role in the formation of new bone by secreting bone matrix?
Which statement is true about osteocytes?
Which statement is true about osteocytes?
What is the primary function of osteoclasts in bone tissue?
What is the primary function of osteoclasts in bone tissue?
Which property of mineral salts is most critical to bone structure?
Which property of mineral salts is most critical to bone structure?
Bone lining cells are primarily involved in:
Bone lining cells are primarily involved in:
What is the main role of collagen fibers in bone tissue?
What is the main role of collagen fibers in bone tissue?
Which statement about the inorganic components of bone is correct?
Which statement about the inorganic components of bone is correct?
What term is used to describe the process by which bone matrix is formed by osteoblasts?
What term is used to describe the process by which bone matrix is formed by osteoblasts?
Which of the following components is primarily responsible for increasing the hardness of bone?
Which of the following components is primarily responsible for increasing the hardness of bone?
Which cell type arises from osteogenic cells and is crucial for bone formation?
Which cell type arises from osteogenic cells and is crucial for bone formation?
What role do proteoglycans and glycoproteins primarily serve in bone tissue?
What role do proteoglycans and glycoproteins primarily serve in bone tissue?
What is the main benefit of collagen fibers breaking upon impact?
What is the main benefit of collagen fibers breaking upon impact?
Which of the following is true about the organic components of bone?
Which of the following is true about the organic components of bone?
What is the primary function of collagen fibers in bone tissue?
What is the primary function of collagen fibers in bone tissue?
What property of bone is significantly influenced by the arrangement of collagen fibers?
What property of bone is significantly influenced by the arrangement of collagen fibers?
What is the primary significance of mineral salts in bone tissue?
What is the primary significance of mineral salts in bone tissue?
Approximately what percentage of bone's overall structure is made up of organic components?
Approximately what percentage of bone's overall structure is made up of organic components?
What is primarily stored in the bone marrow of bones?
What is primarily stored in the bone marrow of bones?
What is the primary function of osteocytes in bone tissue?
What is the primary function of osteocytes in bone tissue?
What characteristic feature differentiates osteoclasts from other bone cells?
What characteristic feature differentiates osteoclasts from other bone cells?
Which component of bone is primarily associated with providing compressive strength?
Which component of bone is primarily associated with providing compressive strength?
Osteogenic cells can differentiate into which type of bone cells?
Osteogenic cells can differentiate into which type of bone cells?
What is the main function of osteoblasts in the context of bone health?
What is the main function of osteoblasts in the context of bone health?
Bone lining cells primarily function to:
Bone lining cells primarily function to:
Which process describes the creation of new bone matrix by osteoblasts?
Which process describes the creation of new bone matrix by osteoblasts?
The presence of mineral salts in bone primarily contributes to which property?
The presence of mineral salts in bone primarily contributes to which property?
What occurs when collagen fibers in bone matrix are subjected to significant impact?
What occurs when collagen fibers in bone matrix are subjected to significant impact?
What role does calcium phosphate play in bone structure?
What role does calcium phosphate play in bone structure?
What term is commonly used to refer to the osteon?
What term is commonly used to refer to the osteon?
Which structural element primarily characterizes the osteon?
Which structural element primarily characterizes the osteon?
What arrangement do collagen fibers have in adjacent lamellae of an osteon?
What arrangement do collagen fibers have in adjacent lamellae of an osteon?
What is the primary function of the tiny weight-bearing pillars found within osteons?
What is the primary function of the tiny weight-bearing pillars found within osteons?
How do the crystals of bone salts interact with collagen fibers in osteons?
How do the crystals of bone salts interact with collagen fibers in osteons?
What is the primary structural feature of an osteon?
What is the primary structural feature of an osteon?
How do the collagen fibers in adjacent lamellae of an osteon orient?
How do the collagen fibers in adjacent lamellae of an osteon orient?
What is the role of tiny weight-bearing pillars within osteons?
What is the role of tiny weight-bearing pillars within osteons?
What is significant about the structure of an osteon in relation to its function?
What is significant about the structure of an osteon in relation to its function?
What role do lamellae play in an osteon's structure?
What role do lamellae play in an osteon's structure?
What are the tiny channels that connect lacunae to the central canal called?
What are the tiny channels that connect lacunae to the central canal called?
What is the primary function of the canaliculi in the bone structure?
What is the primary function of the canaliculi in the bone structure?
Where do osteocytes reside within the osteon?
Where do osteocytes reside within the osteon?
Which structure serves as the main pathway for nutrients and waste products to travel in the bone?
Which structure serves as the main pathway for nutrients and waste products to travel in the bone?
How do osteocytes in lacunae communicate with each other?
How do osteocytes in lacunae communicate with each other?
What is a key characteristic of bones regarding their vascularization?
What is a key characteristic of bones regarding their vascularization?
Which canals contain the blood vessels that supply nutrients to the bone?
Which canals contain the blood vessels that supply nutrients to the bone?
What is the primary function of the blood vessels running between and around osteons?
What is the primary function of the blood vessels running between and around osteons?
Which of the following statements is true regarding bone growth and healing?
Which of the following statements is true regarding bone growth and healing?
What role do Volkmann's canals play in bone structure?
What role do Volkmann's canals play in bone structure?
How does the blood supply in bones affect their overall health?
How does the blood supply in bones affect their overall health?
What happens to the bone if its blood supply is compromised?
What happens to the bone if its blood supply is compromised?
Which of the following structures is responsible for the direct supply of nutrients to osteons?
Which of the following structures is responsible for the direct supply of nutrients to osteons?
What is a key characteristic of spongy bone compared to compact bone?
What is a key characteristic of spongy bone compared to compact bone?
What structures make up the framework of spongy bone?
What structures make up the framework of spongy bone?
What is found within the small, irregular cavities adjacent to trabeculae in spongy bone?
What is found within the small, irregular cavities adjacent to trabeculae in spongy bone?
How do canaliculi function in spongy bone compared to compact bone?
How do canaliculi function in spongy bone compared to compact bone?
What is the primary advantage of the organization of trabeculae in spongy bone?
What is the primary advantage of the organization of trabeculae in spongy bone?
In spongy bone, how do trabeculae respond to changes in stress?
In spongy bone, how do trabeculae respond to changes in stress?
Which type of bone is primarily involved in the production of blood cells due to the presence of red bone marrow?
Which type of bone is primarily involved in the production of blood cells due to the presence of red bone marrow?
The design of spongy bone allows it to:
The design of spongy bone allows it to:
What is the primary function of a negative feedback loop in the body?
What is the primary function of a negative feedback loop in the body?
What role do calcium ions (Ca²⁺) play in the body?
What role do calcium ions (Ca²⁺) play in the body?
When blood calcium levels rise above the normal range, what happens in a negative feedback loop?
When blood calcium levels rise above the normal range, what happens in a negative feedback loop?
What is the primary hormone responsible for increasing blood calcium levels?
What is the primary hormone responsible for increasing blood calcium levels?
How do mechanical forces influence bone remodeling?
How do mechanical forces influence bone remodeling?
What effect do gravitational forces have on bone structure?
What effect do gravitational forces have on bone structure?
What is the result of prolonged inactivity on bone density?
What is the result of prolonged inactivity on bone density?
In calcium homeostasis, what triggers the secretion of parathyroid hormone (PTH)?
In calcium homeostasis, what triggers the secretion of parathyroid hormone (PTH)?
What is the normal range of calcium ions (Ca²⁺) in the blood?
What is the normal range of calcium ions (Ca²⁺) in the blood?
How much calcium is typically found in the human body?
How much calcium is typically found in the human body?
What percentage of total body calcium is stored in bone mineral?
What percentage of total body calcium is stored in bone mineral?
Which hormone decreases blood calcium levels when they are elevated?
Which hormone decreases blood calcium levels when they are elevated?
Why is maintaining blood calcium levels important for the body?
Why is maintaining blood calcium levels important for the body?
What do osteoclasts release to digest the bone matrix?
What do osteoclasts release to digest the bone matrix?
What happens to osteoid after it is secreted by osteoblasts?
What happens to osteoid after it is secreted by osteoblasts?
What process allows for the continuous renewal and maintenance of bone tissue?
What process allows for the continuous renewal and maintenance of bone tissue?
How well-defined is the process of mineralization of osteoid in adult bone?
How well-defined is the process of mineralization of osteoid in adult bone?
Which cells are responsible for the breakdown of bone tissue during remodeling?
Which cells are responsible for the breakdown of bone tissue during remodeling?
At what age does the rate of bone remodeling and deposition begin to decline significantly?
At what age does the rate of bone remodeling and deposition begin to decline significantly?
What is the typical percentage of bone mass lost each decade after the age of 40?
What is the typical percentage of bone mass lost each decade after the age of 40?
Which hormone's decline primarily influences bone remodeling as individuals age?
Which hormone's decline primarily influences bone remodeling as individuals age?
What condition is associated with a significant decline in bone formation after age 35?
What condition is associated with a significant decline in bone formation after age 35?
What factors influence the rate of bone remodeling and deposition as one ages?
What factors influence the rate of bone remodeling and deposition as one ages?
Which type of cartilage is predominant in the skeleton before 8 weeks of gestation?
Which type of cartilage is predominant in the skeleton before 8 weeks of gestation?
What initiates primary ossification?
What initiates primary ossification?
What structure encircles the diaphysis during the early stages of bone development?
What structure encircles the diaphysis during the early stages of bone development?
During endochondral ossification, what happens to the cartilage?
During endochondral ossification, what happens to the cartilage?
What persists after the ossification of the epiphyses?
What persists after the ossification of the epiphyses?
What defines a nondisplaced fracture?
What defines a nondisplaced fracture?
Which type of fracture is characterized by a break that goes all the way through the bone?
Which type of fracture is characterized by a break that goes all the way through the bone?
What is an incomplete fracture?
What is an incomplete fracture?
How does an open (compound) fracture differ from a closed (simple) fracture?
How does an open (compound) fracture differ from a closed (simple) fracture?
Which statement accurately describes a displaced fracture?
Which statement accurately describes a displaced fracture?
In infants, red marrow is primarily located in which part of the bone?
In infants, red marrow is primarily located in which part of the bone?
What is the main role of red marrow in the human body?
What is the main role of red marrow in the human body?
In adults, red marrow is predominantly found in which areas?
In adults, red marrow is predominantly found in which areas?
Where is yellow marrow primarily located in adults?
Where is yellow marrow primarily located in adults?
For clinical procedures, the best source of red marrow in adults is typically found in which part of the body?
For clinical procedures, the best source of red marrow in adults is typically found in which part of the body?
What physiological process is primarily influenced by osteocalcin secretion from osteoblasts?
What physiological process is primarily influenced by osteocalcin secretion from osteoblasts?
What is the effect of osteocalcin on pancreatic beta cells?
What is the effect of osteocalcin on pancreatic beta cells?
In individuals with type 2 diabetes, how are osteocalcin levels typically affected?
In individuals with type 2 diabetes, how are osteocalcin levels typically affected?
What role does insulin have on osteocalcin levels in bone?
What role does insulin have on osteocalcin levels in bone?
Which hormone associated with fat metabolism is stimulated by osteocalcin?
Which hormone associated with fat metabolism is stimulated by osteocalcin?
What effect does osteocalcin secretion by osteoblasts primarily have on the body?
What effect does osteocalcin secretion by osteoblasts primarily have on the body?
How does insulin interact with osteocalcin in bone tissues?
How does insulin interact with osteocalcin in bone tissues?
In individuals with type 2 diabetes, how do osteocalcin levels typically change?
In individuals with type 2 diabetes, how do osteocalcin levels typically change?
Which substance is stimulated by osteocalcin and is known to influence fat metabolism?
Which substance is stimulated by osteocalcin and is known to influence fat metabolism?
Which statement best describes the relationship between osteocalcin and insulin?
Which statement best describes the relationship between osteocalcin and insulin?
What is the primary function of osteocalcin secretion by osteoblasts?
What is the primary function of osteocalcin secretion by osteoblasts?
What role does osteocalcin play in relation to pancreatic beta cells?
What role does osteocalcin play in relation to pancreatic beta cells?
What happens to osteocalcin levels in individuals with type 2 diabetes?
What happens to osteocalcin levels in individuals with type 2 diabetes?
How does insulin interact with osteocalcin in bone tissue?
How does insulin interact with osteocalcin in bone tissue?
Which hormone is stimulated by osteocalcin and plays a role in fat metabolism?
Which hormone is stimulated by osteocalcin and plays a role in fat metabolism?
What is the functional contractile unit of a skeletal muscle?
What is the functional contractile unit of a skeletal muscle?
Which characteristic of skeletal muscle allows it to respond to stimuli?
Which characteristic of skeletal muscle allows it to respond to stimuli?
What is the primary function of skeletal muscle contraction?
What is the primary function of skeletal muscle contraction?
Which process occurs when skeletal muscle receives a neural stimulus?
Which process occurs when skeletal muscle receives a neural stimulus?
Which statement accurately describes skeletal muscles?
Which statement accurately describes skeletal muscles?
What is the structure called that enables each myofiber to receive signals from a nerve?
What is the structure called that enables each myofiber to receive signals from a nerve?
What mechanism initiates muscle contraction?
What mechanism initiates muscle contraction?
Which neurotransmitter is released at the neuromuscular junction to facilitate muscle contraction?
Which neurotransmitter is released at the neuromuscular junction to facilitate muscle contraction?
What is the immediate effect of acetylcholine binding to the muscle fiber membrane?
What is the immediate effect of acetylcholine binding to the muscle fiber membrane?
What occurs at the neuromuscular junction when an action potential from the motor neuron arrives?
What occurs at the neuromuscular junction when an action potential from the motor neuron arrives?
What structure does each myofiber receive from a nerve?
What structure does each myofiber receive from a nerve?
What initiates muscle contraction?
What initiates muscle contraction?
Which neurotransmitter is released at the neuromuscular junction to facilitate muscle contraction?
Which neurotransmitter is released at the neuromuscular junction to facilitate muscle contraction?
What occurs when acetylcholine binds to receptors on the muscle fiber membrane?
What occurs when acetylcholine binds to receptors on the muscle fiber membrane?
Which ion is primarily responsible for triggering muscle contraction after the action potential is generated?
Which ion is primarily responsible for triggering muscle contraction after the action potential is generated?
What happens when acetylcholine (ACh) binds to its receptors on the muscle fiber membrane?
What happens when acetylcholine (ACh) binds to its receptors on the muscle fiber membrane?
Which ions pass through the ligand-gated ion channels after ACh binds to its receptors?
Which ions pass through the ligand-gated ion channels after ACh binds to its receptors?
What is the result of more Na+ diffusing into the muscle fiber than K+ diffusing out?
What is the result of more Na+ diffusing into the muscle fiber than K+ diffusing out?
What is the net effect on the membrane potential when acetylcholine opens ligand-gated ion channels?
What is the net effect on the membrane potential when acetylcholine opens ligand-gated ion channels?
Why does more sodium (Na+) diffuse into the muscle fiber than potassium (K+) diffuses out during local depolarization?
Why does more sodium (Na+) diffuse into the muscle fiber than potassium (K+) diffuses out during local depolarization?
What is the immediate consequence of local depolarization in the muscle fiber membrane?
What is the immediate consequence of local depolarization in the muscle fiber membrane?
What triggers the opening of ligand-gated ion channels in the neuromuscular junction?
What triggers the opening of ligand-gated ion channels in the neuromuscular junction?
What type of ion channel is opened by the binding of acetylcholine at the neuromuscular junction?
What type of ion channel is opened by the binding of acetylcholine at the neuromuscular junction?
What are T-tubules in skeletal muscle cells?
What are T-tubules in skeletal muscle cells?
What is the primary function of T-tubules in muscle fibers?
What is the primary function of T-tubules in muscle fibers?
How do T-tubules contribute to muscle contraction?
How do T-tubules contribute to muscle contraction?
What is the result of the electrical impulse traveling through the T-tubules?
What is the result of the electrical impulse traveling through the T-tubules?
Where are T-tubules located in relation to the sarcomere?
Where are T-tubules located in relation to the sarcomere?
What happens when an electrical impulse travels down the T-tubules?
What happens when an electrical impulse travels down the T-tubules?
Why is it important for T-tubules to transmit electrical impulses deep into the muscle fiber?
Why is it important for T-tubules to transmit electrical impulses deep into the muscle fiber?
Which structure does the T-tubule system work closely with to trigger muscle contraction?
Which structure does the T-tubule system work closely with to trigger muscle contraction?
What is the primary role of the sarcoplasmic reticulum in muscle fibers?
What is the primary role of the sarcoplasmic reticulum in muscle fibers?
How is the sarcoplasmic reticulum best described?
How is the sarcoplasmic reticulum best described?
What occurs when the sarcoplasmic reticulum releases calcium ions?
What occurs when the sarcoplasmic reticulum releases calcium ions?
In which location is calcium stored in a muscle fiber prior to contraction?
In which location is calcium stored in a muscle fiber prior to contraction?
How does the sarcoplasmic reticulum contribute to muscle contraction regulation?
How does the sarcoplasmic reticulum contribute to muscle contraction regulation?
What triggers the sarcoplasmic reticulum to release calcium ions?
What triggers the sarcoplasmic reticulum to release calcium ions?
What happens when calcium is pumped back into the sarcoplasmic reticulum?
What happens when calcium is pumped back into the sarcoplasmic reticulum?
What is the relationship between the sarcoplasmic reticulum and the myofibrils in a muscle fiber?
What is the relationship between the sarcoplasmic reticulum and the myofibrils in a muscle fiber?
What is the role of tropomyosin in muscle contraction?
What is the role of tropomyosin in muscle contraction?
Which of the following accurately describes troponin's functions?
Which of the following accurately describes troponin's functions?
What is the composition of the troponin complex?
What is the composition of the troponin complex?
How do troponin and tropomyosin interact during muscle contraction?
How do troponin and tropomyosin interact during muscle contraction?
What clinical significance do troponin levels in the blood indicate?
What clinical significance do troponin levels in the blood indicate?
What is the outcome when calcium ions bind to troponin during muscle contraction?
What is the outcome when calcium ions bind to troponin during muscle contraction?
How does the movement of tropomyosin affect muscle contraction?
How does the movement of tropomyosin affect muscle contraction?
Which ion is crucial for triggering the movement of tropomyosin during muscle contraction?
Which ion is crucial for triggering the movement of tropomyosin during muscle contraction?
What is the primary function of tropomyosin in resting muscle fibers?
What is the primary function of tropomyosin in resting muscle fibers?
What effect does the removal of calcium from troponin have on muscle fibers?
What effect does the removal of calcium from troponin have on muscle fibers?
What initiates the exposure of myosin-binding sites on actin during contraction?
What initiates the exposure of myosin-binding sites on actin during contraction?
In the absence of calcium ions, what happens to the position of tropomyosin on actin filaments?
In the absence of calcium ions, what happens to the position of tropomyosin on actin filaments?
What is a direct consequence of calcium ions binding to troponin?
What is a direct consequence of calcium ions binding to troponin?
What is excitation-contraction coupling?
What is excitation-contraction coupling?
What triggers the wave of depolarization in the muscle fiber?
What triggers the wave of depolarization in the muscle fiber?
Which structure transmits the action potential deep into the muscle fiber during excitation-contraction coupling?
Which structure transmits the action potential deep into the muscle fiber during excitation-contraction coupling?
What is the immediate effect of the action potential traveling down the T-tubules?
What is the immediate effect of the action potential traveling down the T-tubules?
What is released from the sarcoplasmic reticulum in response to the action potential traveling through the T-tubules?
What is released from the sarcoplasmic reticulum in response to the action potential traveling through the T-tubules?
How does calcium contribute to the excitation-contraction coupling process?
How does calcium contribute to the excitation-contraction coupling process?
What happens after calcium is released from the sarcoplasmic reticulum during excitation-contraction coupling?
What happens after calcium is released from the sarcoplasmic reticulum during excitation-contraction coupling?
Which of the following events directly follows the spread of depolarization across the sarcolemma?
Which of the following events directly follows the spread of depolarization across the sarcolemma?
What happens to calcium (Ca2+) when the action potential (AP) stops?
What happens to calcium (Ca2+) when the action potential (AP) stops?
What occurs to cross-bridge formation when calcium is removed from the cytoplasm?
What occurs to cross-bridge formation when calcium is removed from the cytoplasm?
What causes the muscle fibers to relax after the action potential ends?
What causes the muscle fibers to relax after the action potential ends?
Why do actin and myosin filaments slide past each other when no cross-bridges are formed?
Why do actin and myosin filaments slide past each other when no cross-bridges are formed?
What ensures that the muscle is ready for the next action potential?
What ensures that the muscle is ready for the next action potential?
Why is calcium concentration in the cisternae of the sarcoplasmic reticulum high after muscle relaxation?
Why is calcium concentration in the cisternae of the sarcoplasmic reticulum high after muscle relaxation?
Which mechanism is responsible for returning calcium to the sarcoplasmic reticulum?
Which mechanism is responsible for returning calcium to the sarcoplasmic reticulum?
What is the primary role of ATP during muscle contraction and relaxation?
What is the primary role of ATP during muscle contraction and relaxation?
What occurs to calcium (Ca2+) after the action potential (AP) ceases?
What occurs to calcium (Ca2+) after the action potential (AP) ceases?
What happens to cross-bridge formation when calcium is removed from the cytoplasm?
What happens to cross-bridge formation when calcium is removed from the cytoplasm?
What is the primary reason that muscle fibers relax after the action potential ends?
What is the primary reason that muscle fibers relax after the action potential ends?
Why do actin and myosin filaments slide past each other when no cross-bridges are formed?
Why do actin and myosin filaments slide past each other when no cross-bridges are formed?
What ensures that the muscle is prepared for the next action potential?
What ensures that the muscle is prepared for the next action potential?
Why is there a high concentration of calcium in the cisternae of the sarcoplasmic reticulum after muscle relaxation?
Why is there a high concentration of calcium in the cisternae of the sarcoplasmic reticulum after muscle relaxation?
Which mechanism is responsible for returning calcium to the sarcoplasmic reticulum?
Which mechanism is responsible for returning calcium to the sarcoplasmic reticulum?
What happens to muscle contraction when cross-bridges are broken down by ATP?
What happens to muscle contraction when cross-bridges are broken down by ATP?
What process is primarily responsible for maintaining muscle contraction during active transport?
What process is primarily responsible for maintaining muscle contraction during active transport?
What is the primary reason for the rigidity of muscles after death?
What is the primary reason for the rigidity of muscles after death?
What prevents cross-bridge formation during muscle relaxation?
What prevents cross-bridge formation during muscle relaxation?
What happens to calcium ions in muscle fibers after death?
What happens to calcium ions in muscle fibers after death?
Which of the following effects of rigor mortis is observed as time progresses after death?
Which of the following effects of rigor mortis is observed as time progresses after death?
What role does ATP play in muscle contraction and relaxation mechanisms?
What role does ATP play in muscle contraction and relaxation mechanisms?
What physiological change triggers muscle contraction after death?
What physiological change triggers muscle contraction after death?
Which statement best describes the role of calcium in muscle contraction?
Which statement best describes the role of calcium in muscle contraction?
What occurs to calcium (Ca2+) when the action potential stops?
What occurs to calcium (Ca2+) when the action potential stops?
What is the effect of removing calcium from the cytoplasm on cross-bridge formation?
What is the effect of removing calcium from the cytoplasm on cross-bridge formation?
What causes muscle fibers to relax after the action potential ends?
What causes muscle fibers to relax after the action potential ends?
Why do actin and myosin slide past each other when no cross-bridges are formed?
Why do actin and myosin slide past each other when no cross-bridges are formed?
What ensures that the muscle is ready for the next action potential?
What ensures that the muscle is ready for the next action potential?
Why is calcium concentration in the cisternae of the sarcoplasmic reticulum high after muscle relaxation?
Why is calcium concentration in the cisternae of the sarcoplasmic reticulum high after muscle relaxation?
Which mechanism is responsible for returning calcium to the sarcoplasmic reticulum?
Which mechanism is responsible for returning calcium to the sarcoplasmic reticulum?
What role does ATP play in muscle relaxation?
What role does ATP play in muscle relaxation?
What is the primary mechanism of muscle contraction that involves energy usage?
What is the primary mechanism of muscle contraction that involves energy usage?
What prevents cross-bridge formation during muscle relaxation?
What prevents cross-bridge formation during muscle relaxation?
What physiological process contributes to the rigidity observed during rigor mortis?
What physiological process contributes to the rigidity observed during rigor mortis?
Which event occurs after death that contributes to the phenomenon of rigor mortis?
Which event occurs after death that contributes to the phenomenon of rigor mortis?
Why do muscles remain contracted in rigor mortis despite the lack of ATP?
Why do muscles remain contracted in rigor mortis despite the lack of ATP?
What role does ATP play in muscle contraction and relaxation?
What role does ATP play in muscle contraction and relaxation?
What causes the sustained contraction in muscle fibers post-mortem?
What causes the sustained contraction in muscle fibers post-mortem?
What physiological change primarily leads to the rigidity of muscles after death?
What physiological change primarily leads to the rigidity of muscles after death?
What describes muscle tone?
What describes muscle tone?
What is the primary function of muscle tone?
What is the primary function of muscle tone?
What mechanism is primarily responsible for maintaining muscle tone?
What mechanism is primarily responsible for maintaining muscle tone?
How are small motor units characterized compared to large motor units?
How are small motor units characterized compared to large motor units?
Which statement best describes the function of large motor units?
Which statement best describes the function of large motor units?
What role do spinal reflexes have concerning muscle tone?
What role do spinal reflexes have concerning muscle tone?
Which option correctly defines a small motor unit?
Which option correctly defines a small motor unit?
What factor allows large motor units to produce powerful movements?
What factor allows large motor units to produce powerful movements?
What defines a motor unit?
What defines a motor unit?
What characterizes the latent phase of a muscle contraction?
What characterizes the latent phase of a muscle contraction?
During which phase do muscle fibers actively generate tension and shorten?
During which phase do muscle fibers actively generate tension and shorten?
What is the primary event during the relaxation phase of muscle contraction?
What is the primary event during the relaxation phase of muscle contraction?
Which factor primarily influences the speed and duration of muscle contractions?
Which factor primarily influences the speed and duration of muscle contractions?
Which muscle fiber type is expected to contract the fastest?
Which muscle fiber type is expected to contract the fastest?
Why do some muscle contractions last longer than others?
Why do some muscle contractions last longer than others?
What type of muscle contraction is characterized by a rapid and brief response to a single action potential?
What type of muscle contraction is characterized by a rapid and brief response to a single action potential?
Which type of muscle fiber is primarily associated with endurance activities?
Which type of muscle fiber is primarily associated with endurance activities?
What is a key characteristic of slow-twitch (Type I) muscle fibers?
What is a key characteristic of slow-twitch (Type I) muscle fibers?
Fast-twitch muscle fibers are best suited for which type of activity?
Fast-twitch muscle fibers are best suited for which type of activity?
What is the primary energy source for fast-twitch (Type II) muscle fibers?
What is the primary energy source for fast-twitch (Type II) muscle fibers?
Which of the following best describes the contraction velocity of fast-twitch muscle fibers?
Which of the following best describes the contraction velocity of fast-twitch muscle fibers?
Why do slow-twitch (Type I) fibers have more blood capillaries than fast-twitch (Type II) fibers?
Why do slow-twitch (Type I) fibers have more blood capillaries than fast-twitch (Type II) fibers?
Which muscle fiber type would you expect to have a larger diameter?
Which muscle fiber type would you expect to have a larger diameter?
Fast-twitch fibers (Type II) can be further divided into which categories?
Fast-twitch fibers (Type II) can be further divided into which categories?
Which type of muscle fiber is primarily associated with endurance activities?
Which type of muscle fiber is primarily associated with endurance activities?
What is a key characteristic of slow-twitch (Type I) muscle fibers?
What is a key characteristic of slow-twitch (Type I) muscle fibers?
Fast-twitch muscle fibers are best suited for which type of activity?
Fast-twitch muscle fibers are best suited for which type of activity?
What is the primary energy source for fast-twitch (Type II) muscle fibers?
What is the primary energy source for fast-twitch (Type II) muscle fibers?
Which of the following best describes the contraction velocity of fast-twitch muscle fibers?
Which of the following best describes the contraction velocity of fast-twitch muscle fibers?
Why do slow-twitch (Type I) fibers have more blood capillaries than fast-twitch (Type II) fibers?
Why do slow-twitch (Type I) fibers have more blood capillaries than fast-twitch (Type II) fibers?
Which muscle fiber type would you expect to have a larger diameter?
Which muscle fiber type would you expect to have a larger diameter?
Fast-twitch fibers (Type II) can be further divided into which categories?
Fast-twitch fibers (Type II) can be further divided into which categories?
What primarily causes glycolytic muscles to fatigue quickly?
What primarily causes glycolytic muscles to fatigue quickly?
Which energy pathway do endurance muscles predominantly rely on?
Which energy pathway do endurance muscles predominantly rely on?
What advantage do slow-twitch fibers have during endurance activities?
What advantage do slow-twitch fibers have during endurance activities?
How can muscle function affect fiber type distribution?
How can muscle function affect fiber type distribution?
Which muscle fibers are primarily engaged in short bursts of high-intensity activity?
Which muscle fibers are primarily engaged in short bursts of high-intensity activity?
What is the effect of prolonged exercise on ATP production in muscle fibers?
What is the effect of prolonged exercise on ATP production in muscle fibers?
What adaptation is commonly observed in athletes training for endurance events?
What adaptation is commonly observed in athletes training for endurance events?
What role does lactic acid play in muscle fatigue during high-intensity exercise?
What role does lactic acid play in muscle fatigue during high-intensity exercise?
Why do glycolytic (fast-twitch) muscles fatigue quickly?
Why do glycolytic (fast-twitch) muscles fatigue quickly?
Which energy production pathway is primarily used by endurance muscles with high content of slow-twitch (Type I) fibers?
Which energy production pathway is primarily used by endurance muscles with high content of slow-twitch (Type I) fibers?
What is the main advantage of slow-twitch (Type I) fibers in endurance activities?
What is the main advantage of slow-twitch (Type I) fibers in endurance activities?
How does muscle function influence fiber type composition?
How does muscle function influence fiber type composition?
Which type of muscle fibers is primarily used during short bursts of high-intensity activity?
Which type of muscle fibers is primarily used during short bursts of high-intensity activity?
What happens to ATP production in muscle fibers during prolonged exercise?
What happens to ATP production in muscle fibers during prolonged exercise?
Which of the following adaptations would you expect to see in athletes training for endurance events?
Which of the following adaptations would you expect to see in athletes training for endurance events?
What role does lactic acid play in muscle fatigue during high-intensity exercise?
What role does lactic acid play in muscle fatigue during high-intensity exercise?
What is a primary adaptation to endurance training?
What is a primary adaptation to endurance training?
Which adaptation occurs as a result of strength training?
Which adaptation occurs as a result of strength training?
What is the main goal of endurance training?
What is the main goal of endurance training?
Which adaptation is specifically linked to strength training?
Which adaptation is specifically linked to strength training?
What happens to the number of myofibers as a result of resistance training?
What happens to the number of myofibers as a result of resistance training?
What is the primary reason for the increase in fiber diameter during strength training?
What is the primary reason for the increase in fiber diameter during strength training?
What type of muscle fibers are primarily recruited during endurance training?
What type of muscle fibers are primarily recruited during endurance training?
Which of the following statements is true regarding muscle adaptations to training?
Which of the following statements is true regarding muscle adaptations to training?
What is a primary adaptation to endurance training?
What is a primary adaptation to endurance training?
Which adaptation occurs as a result of strength training?
Which adaptation occurs as a result of strength training?
What is the main goal of endurance training?
What is the main goal of endurance training?
Which adaptation is specifically linked to strength training?
Which adaptation is specifically linked to strength training?
What happens to the number of myofibers as a result of resistance training?
What happens to the number of myofibers as a result of resistance training?
What is the primary reason for the increase in fiber diameter during strength training?
What is the primary reason for the increase in fiber diameter during strength training?
What type of muscle fibers are primarily recruited during endurance training?
What type of muscle fibers are primarily recruited during endurance training?
Which of the following statements is true regarding muscle adaptations to training?
Which of the following statements is true regarding muscle adaptations to training?
Flashcards are hidden until you start studying
Study Notes
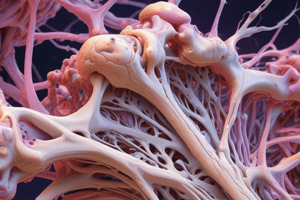
Bone Tissue
- Osteocytes are the primary cell type found in bone tissue.
- Osteoid refers to the matrix of the bone that contains proteoglycans and glycoproteins, providing flexibility and strength.
- Collagen fibers are primarily responsible for the tensile strength of bone, contributing to its flexibility and ability to dissipate energy.
- The organic components of bone, like collagen fibers, proteoglycans, and glycoproteins, provide a buffer against mechanical forces, reducing the risk of fractures.
- Calcium phosphates are the primary inorganic component of bone, contributing to its hardness.
- Approximately 50% of bone's volume and 70% of its weight is made up of inorganic components.
- Mineral salts crystalize around collagen fibers, increasing the hardness of the bone.
- Calcium phosphate plays a crucial role in contributing to the hardness and strength of bone.
- Hydroxyapatite is the main mineral component of bone, contributing to its hardness.
- Bone marrow is the soft, spongy tissue found inside bones, responsible for blood cell production and fat storage.
- Osteoblasts are responsible for building new bone tissue.
- Osteoclasts are responsible for breaking down bone tissue.
Bone Tissue: Cells and Composition
- Osteocytes are the primary cell type found in bone tissue
- Osteoid refers to the organic matrix of bone, which contains proteoglycans and glycoproteins
- Collagen fibers provide tensile strength and flexibility to bone, contributing to its toughness and ability to dissipate energy
- Proteoglycans and glycoproteins contribute to the strength and flexibility of bone, acting as a buffer against mechanical forces and reducing the risk of fractures
- Calcium phosphates are the primary inorganic component of bone, contributing to its hardness
- Mineral salts make up approximately 50% of bone's volume and 70% of its weight, crystalizing around collagen fibers to increase hardness
- Osteogenic cells are the precursor cells that give rise to osteoblasts and most other bone cells
- Osteoblasts form new bone by secreting bone matrix, a process known as osteogenesis
- Osteocytes are formed when osteoblasts become embedded in the bone matrix and communicate mechanical stress signals to remodeling cells
- Osteoclasts are responsible for absorbing bone tissue during growth and healing
- Bone lining cells maintain the bone matrix on surfaces not undergoing remodeling
- Osteocytes are not directly involved in the formation or absorption of bone tissue.
Bone Structure
- Osteocytes are the primary cell type in bone tissue. They are responsible for maintaining the bone matrix and communicating mechanical stress signals to remodeling cells.
- Osteoid is the unmineralized portion of bone, containing proteoglycans and glycoproteins.
- Collagen fibers provide the tensile strength of bone.
- Hydroxyapatite (calcium phosphate) provides compressive strength to bone.
- Bone's organic components (collagen and osteoid) buffer against mechanical forces and reduce the risk of fractures.
- Around 50% of bone's volume is made up of mineral salts, accounting for 70% of bone's weight.
Bone Cells
- Osteoblasts form new bone by secreting bone matrix during the process called osteogenesis.
- Osteoclasts absorb bone tissue during growth and healing.
- Osteogenic cells are the precursors to both osteoblasts and other bone cells.
- Bone lining cells maintain the matrix on surfaces not undergoing remodeling.
Bone Remodeling
- Bone remodeling involves coordinated activity of osteoblasts and osteoclasts.
- Osteoblasts lay down new bone matrix to form new bone.
- Osteoclasts resorb bone tissue and break down bone.
- The continuous process of bone remodeling is essential for maintaining bone strength and responding to changes in mechanical stress.
Osteon
- The osteon is also known as the Haversian system.
- It is a structural unit of compact bone.
- The primary feature is a hollow tube of bone matrix.
- Collagen fibers in adjacent lamellae (concentric rings of bone matrix) run in different directions.
- This arrangement of collagen fibers provides resistance to strain and torsion.
- Bone salts align with and alternate the direction of collagen fibers, further strengthening the osteon.
- The osteon's structure is an example of how structure relates to function.
- Elongated cylinders of an osteon are oriented parallel to the long axis of the bone.
Osteon Structure and Function
- The osteon, also known as the Haversian system, is a primary structural unit of compact bone.
- The osteon is characterized by a hollow tube of bone matrix, which provides strength and resistance to strain and torsion.
- Collagen fibers within adjacent lamellae of an osteon run in different directions, contributing to the bone’s strength and flexibility.
- Tiny weight-bearing pillars within osteons provide resistance to strain and torsion, enhancing the bone’s structural integrity.
- Crystals of bone salts, such as hydroxyapatite, align with and alternate the direction of collagen fibers within the lamellae, contributing to the bone’s hardness and rigidity.
- The structure of the osteon is a clear example of how structure relates to function, as its intricate design maximizes strength and resilience.
- The elongated cylinders of an osteon are oriented parallel to the long axis of the bone, providing support and stability.
- Lamellae, concentric rings of bone matrix, form the structural framework of the osteon, encasing the central canal which contains blood vessels and nerves.
Osteon Structure
- The central canal or Haversian canal, is the main channel within the osteon, containing blood vessels and nerves that supply the bone tissue.
- Osteocytes, mature bone cells, reside in small spaces called lacunae, which are embedded within the lamellae, concentric rings of bone matrix.
- Canaliculi are tiny channels that connect the lacunae to the central canal, allowing for communication and transport of nutrients and waste products between osteocytes.
Osteocyte Communication and Function
- Osteocytes rely on the canaliculi network to communicate with each other and with the central canal.
- This communication system enables the passage of nutrients, oxygen, and waste products, ensuring the survival and function of osteocytes.
- The canaliculi are essential for maintaining the health and integrity of the bone tissue.
Cells of the Osteon
- Osteocytes are the mature bone cells responsible for maintaining the bone tissue, and they reside in the lacunae within the osteon.
- Osteoblasts are responsible for forming new bone matrix, while osteoclasts break down bone tissue, contributing to bone remodeling.
- The Haversian canal serves as the main route for the delivery of nutrients and the removal of waste products from osteocytes.
Bone Vascularization
- Bones have a rich blood supply which is essential for their growth, healing, and overall health.
- Haversian canals and Volkmann's canals contain blood vessels that supply nutrients to the bone.
- Haversian canals run longitudinally through the bone, while Volkmann's canals connect them to each other and the periosteum.
- Blood vessels within the canals deliver nutrients and oxygen to osteocytes, removing waste products as well.
Blood Supply and Bone Health
- A compromised blood supply can lead to weakened bones, impaired healing, and stunted growth.
- Nutrient delivery and waste removal via blood vessels are crucial for maintaining bone health.
- Medullary cavity is a large central space within the bone also supplies nutrients and blood cells.
Further Key Points
- Osteocytes, the mature bone cells, reside in lacunae within the bone matrix.
- Canaliculi are small channels that connect lacunae to each other and to the Haversian canals, facilitating communication between osteocytes.
Spongy Bone vs. Compact Bone
- Spongy bone is lighter and less dense than compact bone.
Spongy Bone Structure
- Trabeculae and bars of bone make up the framework of spongy bone.
- Red bone marrow is found within the small, irregular cavities adjacent to trabeculae.
Canaliculi Function
- Canaliculi in spongy bone connect to adjacent cavities instead of a central Haversian canal.
Trabeculae Advantages
- Trabeculae provide maximum strength.
- Trabeculae can realign to follow lines of stress, which allows for bone adaptation.
Blood Cell Production
- Spongy bone is primarily involved in blood cell production due to the presence of red bone marrow.
Spongy Bone Design
- Spongy bone design allows it to absorb shock and reduce weight while maintaining strength.
Negative Feedback Loops
- Maintain homeostasis by reversing deviations from a set point.
- Act to counter changes in the body's internal environment.
Calcium in the Body
- Essential for:
- Muscle contraction
- Nerve impulse transmission
- Bone structure
Calcium Homeostasis
- High blood calcium levels: Trigger the release of calcitonin, which lowers calcium levels.
- Low blood calcium levels: Trigger the release of parathyroid hormone (PTH), which increases calcium levels.
- PTH:
- Stimulates calcium reabsorption in the kidneys.
- Increases calcium absorption from the gut.
- Promotes bone resorption (breakdown of bone tissue).
Bone Remodeling
- Mechanical forces:
- Stimulate bone formation in areas subjected to stress.
- Influence the alignment and strength of bone trabeculae.
- Prolonged inactivity:
- Decreases bone density due to lack of mechanical stress.
Calcium in the Blood
- The normal blood calcium ion (Ca²⁺) concentration ranges between 9 and 11 mg/dl.
Calcium in the Body
- The human body typically contains between 1200 and 1400 grams of calcium.
- 99% of the body's calcium is stored in bones.
- 1.5 grams of calcium are typically present in the blood.
Calcium Homeostasis
- The hormonal control loop is the primary mechanism responsible for maintaining stable blood calcium levels.
- Calcitonin is a hormone that decreases blood calcium levels when they are elevated.
- Parathyroid hormone (PTH) increases blood calcium levels. PTH stimulates bone resorption, calcium reabsorption in the kidneys, and calcium absorption in the intestines.
Importance of Calcium
- Calcium is crucial for various bodily functions, including:
- Muscle contraction
- Nerve function
- Blood clotting
Osteoclasts and Bone Resorption
- Osteoclasts release proteolytic enzymes and H⁺ ions to digest the bone matrix.
- The primary function of osteoclasts is to release calcium and phosphorus into the blood circulation.
- Osteoclasts are responsible for the breakdown of bone tissue during bone remodeling.
Osteoblasts and Bone Formation
- Osteoblasts secrete osteoid, an unmineralized matrix that contributes to bone formation.
- After secretion, osteoid undergoes mineralization, a process that is not fully understood.
- Approximately 5% of adult bone is remodeled each week.
Bone Remodeling
- Bone remodeling is a continuous process that allows for the renewal and maintenance of bone tissue. This involves both bone formation by osteoblasts and bone resorption by osteoclasts.
Bone Remodeling and Deposition
- Bone remodeling and deposition are most vigorous up to age 25.
- Between ages 25 and 35, the rate of bone remodeling slowly declines.
- After age 40, bone reabsorption exceeds bone formation.
- About 10% of bone mass is lost each decade after age 40.
- This decline in bone formation after age 35 leads to a higher risk of fractures and osteoporosis.
Factors Influencing Bone Health
- Physical activity levels and diet significantly influence the rate of bone remodeling and deposition as one ages.
- Estrogen and testosterone, which decrease with age, are key hormones that influence bone remodeling.
Maintaining Bone Health After Age 40
- It is crucial to maintain bone health after age 40 to reduce the risk of osteoporosis and fractures.
Cartilage Types and Development
- Hyaline cartilage is the primary cartilage in the skeleton before 8 weeks of gestation.
Primary Ossification
- Primary ossification is the process of bone formation from hyaline cartilage.
- The first step is the secretion of osteoid by periosteal osteoblasts.
- A bone collar forms around the diaphysis during primary ossification.
Endochondral Ossification
- Endochondral ossification is the process by which cartilage is replaced by bone.
- Calcification of cartilage occurs during this process.
Periosteal Bud and Ossification
- The periosteal bud, containing blood vessels, nerves, and red marrow, infiltrates the diaphysis during ossification.
Bone Formation and Elongation
- As the diaphysis elongates and the medullary cavity appears, spongy bone is formed.
Epiphyseal Ossification
- The epiphyses ossify, but hyaline cartilage persists at the epiphyseal plates and articular surfaces.
- Hyaline cartilage remains only at the epiphyseal plates and articular cartilages after the epiphyses ossify.
Fracture Types
- Nondisplaced fracture: Bone remains in its normal position, no misalignment.
- Displaced fracture: Bone ends are out of alignment, requiring medical intervention.
- Complete fracture: Break extends completely through the bone.
- Incomplete fracture: Break does not go all the way through the bone, it's partial.
- Open (compound) fracture: Bone protrudes through the skin, increasing risk of infection.
- Closed (simple) fracture: Skin remains intact, no bone protrusion.
Red Marrow Location and Function
- Red marrow is found in the medullary cavity of the diaphysis and all areas of spongy bone in infants.
- The primary function of red marrow is haematopoiesis (production of blood cells).
- In adults, red marrow is mostly found in the diploe of flat bones like the pelvis, sternum, and skull.
- In adults, red marrow is specifically found in the head of long bones.
Yellow Marrow
- Yellow marrow primarily consists of fat.
- In adults, yellow marrow extends into the epiphyses of long bones.
Bone Marrow Biopsy
- Bone marrow is most commonly taken from the hip bone (pelvis) for clinical bone marrow biopsies.
- The flat bones, such as the pelvis, are typically the best source of red marrow for clinical procedures in adults.
Osteocalcin and Insulin
- Osteocalcin is a hormone secreted by osteoblasts, primarily influencing insulin production and uptake.
- Osteocalcin targets pancreatic beta cells to divide and produce insulin.
- Osteocalcin levels are reduced in patients with type 2 diabetes.
- Insulin activates inactive osteocalcin in bone.
Osteocalcin and Adiponectin
- Osteocalcin stimulates the release of adiponectin from adipocytes.
- Adiponectin restricts fat storage.
FGF23
- Fibroblast growth factor 23 (FGF23) regulates phosphate reabsorption in the kidneys.
Osteocalcin and Insulin: Synergistic Relationship
- Osteocalcin and insulin have a two-way synergistic mechanism.
- Osteocalcin promotes insulin production, and insulin activates osteocalcin.
Osteocalcin and Insulin Production
- Osteocalcin, secreted by osteoblasts, primarily influences insulin production and uptake.
- Osteocalcin directly targets pancreatic beta cells to promote their division and insulin production.
- In patients with type 2 diabetes, osteocalcin levels are reduced.
- Insulin activates inactive osteocalcin in bone.
Adiponectin and Fat Storage
- Adiponectin, a hormone released by adipocytes, is stimulated by osteocalcin.
- Adiponectin restricts fat storage and promotes energy expenditure.
FGF23 and Phosphate Regulation
- Fibroblast growth factor 23 (FGF23) regulates phosphate reabsorption in the kidneys.
The Relationship between Osteocalcin and Insulin
- There is a two-way synergistic mechanism between osteocalcin and insulin.
- This means that they both influence each other's function and activity.
Osteocalcin & Insulin
- Osteocalcin is secreted by osteoblasts and primarily influences insulin production and uptake.
- Osteocalcin targets pancreatic beta cells to divide and produce insulin.
- Osteocalcin levels are reduced in patients with type 2 diabetes.
- Insulin activates inactive osteocalcin in bone.
Osteocalcin & Adiponectin
- Osteocalcin stimulates the release of adiponectin from adipocytes.
- Adiponectin restricts fat storage.
Osteocalcin & FGF23
- FGF23 regulates phosphate reabsorption in the kidneys.
Relationship between Osteocalcin & Insulin
- There is a two-way synergistic mechanism between osteocalcin and insulin.
The Functional Contractile Unit of Skeletal Muscle
- The sarcomere is the functional contractile unit of a skeletal muscle.
Characteristics of Skeletal Muscle
- Excitability: The ability of skeletal muscle to respond to stimuli, such as nerve impulses.
Primary Function of Skeletal Muscle Contraction
- The primary function of skeletal muscle contraction is to move bones.
Muscle Contractility
- Contractility refers to the muscle's ability to shorten and produce movement.
The Sarcomere in a Skeletal Muscle
- The sarcomere is the area between two Z discs.
Neural Stimulation and Skeletal Muscle
- When skeletal muscle receives a neural stimulus, it becomes excitable and contracts.
The Role of Skeletal Muscle Contraction in Maintaining Posture
- Skeletal muscle contraction keeps the body upright and stable, maintaining posture.
Skeletal Muscle Contraction and Movement
- Skeletal muscles contract to produce movement.
Neuromuscular Junction
- The neuromuscular junction is a specialized synapse where a motor neuron communicates with a muscle fiber.
- A single motor neuron can innervate multiple muscle fibers.
- Acetylcholine is the neurotransmitter released at the neuromuscular junction.
- Acetylcholine binding to receptors on the muscle fiber membrane triggers an action potential in the muscle fiber.
- This action potential travels along the muscle fiber, leading to muscle contraction.
Muscle Contraction Initiation
- An action potential traveling down a motor neuron initiates muscle contraction.
- This action potential triggers the release of acetylcholine from the motor neuron's axon terminal.
- Acetylcholine diffuses across the synaptic space and binds to receptors on the muscle fiber membrane.
- This binding triggers an action potential in the muscle fiber, leading to the release of calcium ions from the sarcoplasmic reticulum.
- Calcium ions bind to troponin, initiating the sliding filament mechanism of muscle contraction.
The Neuromuscular Junction
-
The neuromuscular junction is the specialized synapse between a motor neuron and a muscle fiber.
-
It is responsible for transmitting signals from the nervous system to the muscles, initiating muscle contraction.
Muscle Contraction Initiation
-
Muscle contraction is initiated by an action potential traveling down the motor neuron.
-
This action potential triggers the release of acetylcholine from the motor neuron's axon terminal.
-
Acetylcholine diffuses across the synapse and binds to receptors on the muscle fiber membrane.
-
This binding triggers the muscle fiber to generate its own action potential.
Role of Calcium
-
The action potential in the muscle fiber travels along the sarcolemma and into the T-tubules.
-
This triggers the release of calcium ions from the sarcoplasmic reticulum.
-
Calcium ions bind to troponin, a protein that regulates the interaction between actin and myosin filaments.
-
This binding allows the actin and myosin filaments to slide past each other, shortening the muscle fiber and causing contraction.
Acetylcholine and Muscle Contraction
- Acetylcholine (ACh) binding to its receptors on the muscle fiber membrane opens ligand-gated ion channels
- These channels allow sodium (Na+) and potassium (K+) ions to pass through
- More Na+ diffuses into the muscle fiber than K+ diffuses out due to the electrochemical gradient favoring sodium influx
- This causes a transient change in membrane potential, known as local depolarization
- Local depolarization triggers the action potential to spread across the sarcolemma
Neuromuscular Junction: The Key to Muscle Activation
- The binding of acetylcholine (ACh) to its receptors at the neuromuscular junction opens ligand-gated ion channels
- These are not voltage-gated, mechanically-gated, or leak channels
- The opening of these channels allows for the influx of sodium and potassium ions, triggering the sequence of events that lead to muscle contraction
T-tubules in Muscle Cells
- T-tubules are continuous extensions of the sarcolemma (muscle cell membrane) that penetrate deep into the muscle fiber.
- They are essential for transmitting electrical impulses from the surface of the muscle fiber to the interior, ensuring a coordinated contraction of the entire cell.
- This transmission is crucial because it triggers the release of calcium ions from the sarcoplasmic reticulum (SR), which are necessary for muscle contraction.
- T-tubules are located at the A-band/I-band junction of the sarcomere, the functional unit of muscle contraction.
- They work closely with the SR to initiate muscle contraction by allowing the electrical impulse to reach the SR, stimulating calcium release.
- Without T-tubules, the electrical impulse would only affect the surface of the muscle fiber, resulting in a weak and uncoordinated contraction.
- The T-tubule system ensures the synchronized release of calcium ions along the entire length of the muscle fiber, resulting in a strong and coordinated contraction.
Sarcoplasmic Reticulum (SR) and Muscle Contraction
-
Primary Role of SR: The SR's primary role is to regulate muscle contraction by storing and releasing calcium ions (Ca2+).
-
Structure: The SR is an elaborate smooth endoplasmic reticulum that surrounds each myofibril within a muscle fiber.
-
Calcium Release: When an action potential travels down a T-tubule, it triggers the release of Ca2+ from the SR.
-
Contraction Initiation: The release of Ca2+ into the sarcoplasm allows myosin heads to bind to actin filaments, initiating muscle contraction.
-
Calcium Reuptake: After contraction, Ca2+ is actively pumped back into the SR by the SR Ca2+ ATPase pump, leading to muscle relaxation.
-
Relationship with Myofibrils: The SR is positioned around the myofibrils, ensuring that Ca2+ release is precisely targeted to the contractile proteins for efficient contraction.
Troponin
- A protein complex found in skeletal and cardiac muscle fibers
- Controls muscle contraction by regulating the interaction of actin and myosin
- Binds calcium ions (Ca²⁺) to trigger contraction
- Composed of three subunits:
- Troponin C: Binds calcium.
- Troponin I: Inhibits actin-myosin interactions.
- Troponin T: Binds to tropomyosin.
- Elevated blood troponin levels indicate damage to cardiac muscle, often used as a biomarker for myocardial infarction (heart attack)
Tropomyosin
- A long, coiled protein found along the length of actin filaments
- Regulates muscle contraction by blocking myosin binding sites on actin in the absence of calcium.
- Composed of two identical polypeptide chains forming a coiled-coil structure
- Positions itself along actin filaments, stabilizing them.
- Allows contraction when calcium binds to troponin, triggering a shift in tropomyosin, exposing active sites on actin for myosin.
Interaction Between Troponin and Tropomyosin
- Both proteins work together to regulate muscle contraction.
- Calcium binding to troponin leads to a shift in tropomyosin, exposing active sites on actin.
- Essential for the contraction mechanism in both skeletal and cardiac muscle.
Muscle Contraction and Troponin
- Calcium ions (Ca2+) bind to troponin during muscle contraction.
- This binding causes troponin to change shape, pulling tropomyosin away from the myosin-binding sites on actin.
- The exposure of myosin-binding sites allows myosin heads to bind to actin, forming cross-bridges.
- Tropomyosin blocks myosin-binding sites on actin filaments when the muscle is at rest, preventing contraction.
- This blocking action is reversed when calcium binds to troponin.
- When calcium is removed from troponin, tropomyosin returns to its blocking position, preventing further cross-bridge formation and muscle contraction.
Excitation-Contraction Coupling
- The link between the action potential and muscle contraction.
Muscle Fiber Depolarization
- Triggered by the influx of sodium ions through ligand-gated channels.
T-tubules
- Transmit the action potential deep into the muscle fiber.
Calcium Release
- The action potential traveling down T-tubules triggers the release of calcium ions from the sarcoplasmic reticulum.
Calcium and Contraction
- Calcium binds to troponin, causing tropomyosin to move away from the myosin-binding sites on actin.
- This allows myosin heads to bind to actin filaments, initiating contraction.
Relaxation
- After the action potential is over, calcium is actively transported back into the sarcoplasmic reticulum.
- This allows tropomyosin to cover the myosin binding sites on actin again, ending the contraction.
Muscle Relaxation and Calcium
- When the action potential stops, calcium (Ca2+) is pumped back into the sarcoplasmic reticulum.
- This is achieved through active transport, which requires ATP.
Cross-Bridge Formation and Muscle Relaxation
- When calcium is removed from the cytoplasm, cross-bridge formation is inhibited.
- This is because calcium binds to troponin, which moves tropomyosin away from the myosin-binding sites on actin.
- Without calcium, tropomyosin blocks the myosin-binding sites, preventing cross-bridge formation.
- This allows actin and myosin filaments to slide past each other, leading to muscle relaxation.
Actin and Myosin Sliding
- During relaxation, actin and myosin filaments slide past each other due to contraction of another muscle or the muscle's own weight.
- This is not due to any active process within the muscle fiber itself.
The Sarcoplasmic Reticulum and Muscle Relaxation
- After muscle relaxation, calcium is stored in the cisternae of the sarcoplasmic reticulum, ensuring it's readily available for the next muscle contraction.
- This high concentration of calcium in the sarcoplasmic reticulum facilitates rapid diffusion into the cytoplasm when the next action potential arrives.
Preventing Cross-Bridge Formation
- The absence of calcium in the cytoplasm prevents cross-bridge formation during muscle relaxation.
- This is because calcium is essential for moving tropomyosin away from the myosin-binding sites on actin.
Rigor Mortis
- Rigor mortis refers to the stiffening of muscles after death.
- It starts about 4 hours after death, peaks at approximately 13 hours, and lasts about 50 hours.
- The lack of ATP after death causes the myosin heads to remain attached to the actin filaments, resulting in a sustained muscle contraction.
- As ATP is required to detach the myosin heads from the actin filaments and pump calcium back into the sarcoplasmic reticulum, the muscles stay contracted in rigor mortis.
- Calcium leakage from the sarcoplasmic reticulum into the cytoplasm further contributes to the formation of cross-bridges between actin and myosin.
- Without ATP, the muscle fibers cannot relax, leading to the stiffening associated with rigor mortis.
Rigor Mortis
-
ATP Depletion
- ATP is vital for muscle contraction & relaxation.
- Muscle cells require ATP to detach myosin heads from the actin filaments after contraction.
- ATP production ends after death due to lack of oxygen, preventing ATP regeneration.
-
Cross-Bridge Formation
- Without ATP, myosin heads remain attached to actin filaments, causing continuous & sustained contraction.
- This inability of myosin to detach from actin results in muscle rigidity.
-
Calcium Leakage
- After death, calcium ions leak from the sarcoplasmic reticulum (SR) into the cytoplasm. - This leakage triggers calcium binding to troponin, moving tropomyosin away from actin's myosin-binding sites.
- This promotes cross-bridge formation, but the lack of ATP prevents the cycle from completing, sustaining contraction.
-
Lack of Relaxation
- ATP is also needed to pump calcium back into the SR.
- The persistent excess calcium in the cytoplasm maintains the contraction and rigidity.
-
Rigor Mortis onset: >4 hours after death
- Rises to a peak at ~13 hours
- Persists for ~50 hours
Muscle Tone
- Muscle Tone is a state of partial contraction that maintains muscle firmness without active movement.
- Spinal reflexes activate motor units, which are responsible for maintaining muscle tone.
Function of Muscle Tone
- The function of muscle tone is to maintain posture and stabilize joints.
Motor Units
- Small motor units control fine movements, while large motor units control large muscles.
- A small motor unit is a single neuron controlling a few muscle fibers, enabling precise movement.
- Large motor units are found in muscles that produce powerful, large-scale movements like those in the thighs or back.
Spinal Reflexes and Muscle Tone
- Spinal reflexes contribute to muscle tone by intermittently activating motor units, ensuring muscles are ready for action.
Importance of Muscle Tone
- Muscle tone, even in relaxed muscles, ensures muscles are primed for immediate response to stimuli.
Motor Units
- A motor unit is a single motor neuron and all the muscle fibers it innervates
- Each motor neuron can innervate multiple muscle fibers, but each muscle fiber is only innervated by one motor neuron
Muscle Contraction Phases
- Latent Phase: A brief delay between the action potential and the onset of contraction
- Contraction Phase: Muscle fibers generate tension and shorten
- Relaxation Phase: Calcium is pumped back into the sarcoplasmic reticulum, and tension decreases
Muscle Fiber Types and Contraction Speed and Duration
- There are three main types of muscle fibers:
- Type I fibers (slow-twitch): Slow contraction speed, high resistance to fatigue, used for endurance activities
- Type IIa fibers (fast-twitch, oxidative): Faster contraction speed than type-I, high resistance to fatigue, used for activities requiring both power and endurance
- Type IIb fibers (fast-twitch, glycolytic): Fastest contraction speed, low resistance to fatigue, used for short bursts of power
Factors Influencing Contraction Speed and Duration
- Muscle fiber type: Type I fibers are slowest while Type IIb are fastest.
- Metabolic properties: Type I fibers are highly aerobic and use oxygen efficiently, while Type IIb fibers are glycolytic and utilize anaerobic metabolism.
- Number of motor units activated: Recruiting more motor units increases contraction strength and speed.
- Frequency of action potentials: More frequent action potentials lead to a stronger contraction.
Types of Muscle Contractions
- Twitch contraction: A rapid and brief response to a single action potential.
- Tetanic contraction: A sustained, powerful contraction resulting from a high frequency of action potentials.
Muscle Fiber Types
- Type I fibers are primarily associated with endurance activities.
- Type I fibers are slow-twitch and have a high myoglobin content, which allows for aerobic respiration.
- Type II fibers are fast-twitch and are best suited for activities like sprinting or weightlifting.
- Type II fibers primarily use anaerobic glycolysis for energy production.
- Type II fibers have a rapid and powerful contraction velocity.
- Type I fibers have a higher capillary density than Type II fibers to supply oxygen for aerobic metabolism.
- Type IIb fibers have a larger diameter than Type I fibers.
- Type I fibers can sustain prolonged activity due to increased myoglobin and capillary density.
- Type II fibers can be further divided into Type IIa and Type IIb.
### Muscle Fiber Types
- Type I fibers are primarily associated with endurance activities.
- Type I fibers have a high myoglobin content which allows for greater oxygen storage and aerobic metabolism.
- Type I fibers have a slower contraction velocity but can sustain prolonged activity.
- Type I fibers have a higher density of blood capillaries to deliver oxygen for sustained aerobic metabolism.
- Type I fibers have a smaller diameter compared to Type II fibers.
Fast-twitch Muscle Fibers
- Fast-twitch fibers (Type II) are best suited for high-intensity, short-duration activities such as sprinting or weightlifting.
- Type II fibers primarily rely on anaerobic glycolysis for energy production.
- Type II fibers have a rapid and powerful contraction velocity.
- Type II fibers have a larger diameter than Type I fibers.
- Type II fibers can be further divided into Type IIa and Type IIb.
### Type IIa and Type IIb Fibers
- Type IIa fibers are intermediate in their characteristics, possessing some qualities of both Type I and Type IIb fibers.
- Type IIb fibers are fastest-twitching and have the largest diameter. They are the most powerful but fatigue quickly
Muscle Fatigue and Fiber Types
- Fast-twitch (Type IIb) muscle fibers fatigue quickly due to lactic acid build-up from anaerobic metabolism.
- Slow-twitch (Type I) muscle fibers primarily use aerobic oxidative phosphorylation for energy production, allowing them to sustain prolonged activity.
- Slow-twitch fibers are advantageous for endurance activities due to their ability to constantly supply ATP.
Muscle Function and Fiber Type Adaptation
- Different activities and training can lead to adaptations in muscle fiber type distribution.
- Short bursts of high-intensity activity primarily utilize Type IIb fibers.
ATP Production and Prolonged Exercise
- Type I fibers maintain a constant ATP production through aerobic processes during prolonged exercise.
Endurance Training Adaptations
- Endurance training leads to an increased number of slow-twitch fibers and mitochondrial density.
Lactic Acid and Muscle Fatigue
- Lactic acid build-up during high-intensity exercise decreases muscle pH, contributing to fatigue.
Muscle Fatigue and Fiber Types
- Fast-twitch (Type IIb) muscle fibers fatigue quickly due to lactic acid build-up from anaerobic metabolism.
- Endurance muscles rely primarily on aerobic oxidative phosphorylation for energy production, fueled by slow-twitch (Type I) fibers.
- Slow-twitch fibers are suited for endurance activities because they can sustain prolonged activity with a constant supply of ATP.
- Muscle fiber type composition is adaptable based on activity and training.
- High-intensity, short-burst activities primarily utilize fast-twitch (Type IIb) fibers.
- Type I fibers maintain consistent ATP production through aerobic processes during prolonged exercise.
- Endurance training leads to increased slow-twitch fibers and mitochondrial density.
- Lactic acid contributes to muscle fatigue during high-intensity exercise by lowering pH in the muscle environment.
Muscle Adaptations to Training
- Endurance training leads to an increase in the number of mitochondria and capillaries in muscle fibers. This enhances the muscle's aerobic capacity.
- Strength training primarily leads to the fusion of satellite cells to increase nuclear content in muscle fibers. This increases the cross-sectional area of muscle fibers and thus muscle strength.
- Slow-twitch (Type I) muscle fibers are primarily recruited during endurance training, while strength training primarily impacts the cross-sectional area of muscle fibers.
- The number of myofibers in a muscle does not increase as a result of either endurance or strength training.
- Strength training increases the nuclear content of muscle fibers without increasing myofiber numbers, primarily due to an increase in the amount of actin and myosin.
Muscle Adaptations to Training
- Endurance training primarily leads to an increase in the number of mitochondria and capillaries within muscle fibers.
- Strength training results in an increase in the nuclear content of muscle fibers through the fusion of satellite cells. This does not increase the number of myofibers.
- The main goal of endurance training is to improve aerobic capacity and stamina.
- Strength training mainly leads to an increase in the cross-sectional area of muscle fibers.
- The increase in fiber diameter during strength training occurs because of an increase in the amount of actin and myosin.
- Endurance training mainly recruits slow-twitch (Type I) muscle fibers.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.