Podcast
Questions and Answers
What is the inheritance pattern of the most common inherited abnormality of the red blood cell membrane?
What is the inheritance pattern of the most common inherited abnormality of the red blood cell membrane?
It is usually transmitted as an autosomal dominant disorder, but can also be autosomal recessive.
Which proteins are partially deficient in the disorder affecting red blood cell membranes?
Which proteins are partially deficient in the disorder affecting red blood cell membranes?
The disorder results from a partial deficiency of spectrin or ankyrin.
What are the consequences of the membrane defect in red blood cells?
What are the consequences of the membrane defect in red blood cells?
The defect leads to the formation of spherocytes that are poorly deformable and have a shortened life span.
What condition may require phototherapy or exchange transfusions during the neonatal period?
What condition may require phototherapy or exchange transfusions during the neonatal period?
What is a potential consequence of prolonged splenic trapping of spherocytes?
What is a potential consequence of prolonged splenic trapping of spherocytes?
What happens to hemoglobin (Hb) levels in infants, and why is this significant?
What happens to hemoglobin (Hb) levels in infants, and why is this significant?
How does the heart compensate for low hemoglobin in infants, and what are the potential outcomes?
How does the heart compensate for low hemoglobin in infants, and what are the potential outcomes?
What remains unchanged with age in a person's blood profile according to the document?
What remains unchanged with age in a person's blood profile according to the document?
What are the implications of a hyperdynamic circulation in infants as a compensatory mechanism?
What are the implications of a hyperdynamic circulation in infants as a compensatory mechanism?
Why is it important to monitor hemoglobin levels in neonates and infants?
Why is it important to monitor hemoglobin levels in neonates and infants?
What can occur if the heart is overloaded due to compensatory mechanisms in infants?
What can occur if the heart is overloaded due to compensatory mechanisms in infants?
What role does the heart play in compensating for anemia in infants?
What role does the heart play in compensating for anemia in infants?
What are the main causes of decreased RBC production?
What are the main causes of decreased RBC production?
List three types of microcytic anemia.
List three types of microcytic anemia.
What is macrocytic anemia and what are two common causes?
What is macrocytic anemia and what are two common causes?
What does an increased reticulocyte count usually indicate?
What does an increased reticulocyte count usually indicate?
Explain the relationship between hypothyroidism and anemia.
Explain the relationship between hypothyroidism and anemia.
How does hypersplenism affect RBC survival?
How does hypersplenism affect RBC survival?
What is the significance of the four stages of iron deficiency?
What is the significance of the four stages of iron deficiency?
Describe what is meant by normocytic anemia.
Describe what is meant by normocytic anemia.
What are the implications of having iron deficiency without anemia for a significant portion of the population?
What are the implications of having iron deficiency without anemia for a significant portion of the population?
What genetic mutation commonly causes β-thalassemia?
What genetic mutation commonly causes β-thalassemia?
What distinguishes β-thalassemia major from minor?
What distinguishes β-thalassemia major from minor?
What are symptoms of β-thalassemia major observed in infants?
What are symptoms of β-thalassemia major observed in infants?
What is the silent carrier state for β-thalassemia?
What is the silent carrier state for β-thalassemia?
Describe a common diagnostic characteristic of β-thalassemia.
Describe a common diagnostic characteristic of β-thalassemia.
What is a potential physical manifestation of severe anemia due to β-thalassemia?
What is a potential physical manifestation of severe anemia due to β-thalassemia?
What does 'crew cut' or 'hair on end' appearance refer to?
What does 'crew cut' or 'hair on end' appearance refer to?
How does β-thalassemia intermedia present in comparison to β-thalassemia major?
How does β-thalassemia intermedia present in comparison to β-thalassemia major?
What type of anemia is commonly associated with β-thalassemia?
What type of anemia is commonly associated with β-thalassemia?
What role does hemolysis play in thalassemia-related symptoms?
What role does hemolysis play in thalassemia-related symptoms?
What are the most common manifestations of G6PD deficiency during episodes of hemolysis?
What are the most common manifestations of G6PD deficiency during episodes of hemolysis?
How does the age of red blood cells affect G6PD deficiency?
How does the age of red blood cells affect G6PD deficiency?
Which factors can induce episodes of hemolytic anemia in G6PD deficiency?
Which factors can induce episodes of hemolytic anemia in G6PD deficiency?
What is a typical urine finding during a hemolytic episode in G6PD deficiency?
What is a typical urine finding during a hemolytic episode in G6PD deficiency?
Describe the general health of children with G6PD deficiency between hemolytic episodes.
Describe the general health of children with G6PD deficiency between hemolytic episodes.
What are some symptoms associated with hemolytic anemia in G6PD deficiency?
What are some symptoms associated with hemolytic anemia in G6PD deficiency?
What laboratory findings are associated with hemolysis in G6PD deficiency?
What laboratory findings are associated with hemolysis in G6PD deficiency?
Why are older red cells more affected by G6PD deficiency?
Why are older red cells more affected by G6PD deficiency?
What is the significance of stress in G6PD deficiency?
What is the significance of stress in G6PD deficiency?
What is the effect of specific foods like fava beans in G6PD deficiency?
What is the effect of specific foods like fava beans in G6PD deficiency?
What is thalassemia and how does it affect hemoglobin production?
What is thalassemia and how does it affect hemoglobin production?
What are some common symptoms of thalassemia?
What are some common symptoms of thalassemia?
What methods are typically used to diagnose thalassemia?
What methods are typically used to diagnose thalassemia?
How does iron chelation therapy help thalassemia patients?
How does iron chelation therapy help thalassemia patients?
Describe the role of blood transfusions in managing severe thalassemia.
Describe the role of blood transfusions in managing severe thalassemia.
What can happen if thalassemia is left untreated over time?
What can happen if thalassemia is left untreated over time?
What is the significance of bone marrow transplantation in thalassemia?
What is the significance of bone marrow transplantation in thalassemia?
How does the severity of thalassemia vary among individuals?
How does the severity of thalassemia vary among individuals?
Why is long-term management important for individuals with thalassemia?
Why is long-term management important for individuals with thalassemia?
What are the potential physical manifestations of severe anemia due to β-thalassemia?
What are the potential physical manifestations of severe anemia due to β-thalassemia?
What protein is primarily affected in iron deficiency anemia, leading to reduced oxygen transport?
What protein is primarily affected in iron deficiency anemia, leading to reduced oxygen transport?
Identify two dietary sources that can help increase iron intake to treat iron deficiency anemia.
Identify two dietary sources that can help increase iron intake to treat iron deficiency anemia.
Describe a symptom that may indicate a severe case of G6PD deficiency.
Describe a symptom that may indicate a severe case of G6PD deficiency.
What are two common triggers for hemolytic anemia in individuals with G6PD deficiency?
What are two common triggers for hemolytic anemia in individuals with G6PD deficiency?
What genetic mutation results in the production of abnormal hemoglobin in sickle cell anemia?
What genetic mutation results in the production of abnormal hemoglobin in sickle cell anemia?
What primary complication should be addressed for patients experiencing pain crises in sickle cell anemia?
What primary complication should be addressed for patients experiencing pain crises in sickle cell anemia?
How can chronic blood loss pose a risk factor for developing iron deficiency anemia?
How can chronic blood loss pose a risk factor for developing iron deficiency anemia?
In G6PD deficiency, what diagnostic test is typically utilized to measure the enzyme's levels?
In G6PD deficiency, what diagnostic test is typically utilized to measure the enzyme's levels?
What preventive measure can reduce the risk of developing iron deficiency anemia?
What preventive measure can reduce the risk of developing iron deficiency anemia?
What role does genetic counseling play for families affected by sickle cell anemia?
What role does genetic counseling play for families affected by sickle cell anemia?
Flashcards
Anemia in Infants
Anemia in Infants
A condition where the blood doesn't carry enough oxygen to the body's tissues. It can occur in infants due to their rapid growth and increased oxygen demand.
Hemoglobin (Hb) in Anemia
Hemoglobin (Hb) in Anemia
Anemia in infants is characterized by a decrease in hemoglobin (Hb) levels. Hemoglobin carries oxygen in the blood.
Heart Rate in Anemia
Heart Rate in Anemia
Infants with anemia may experience a faster heart rate to compensate for the lack of oxygen. This puts extra strain on the heart.
Hyperdynamic Circulation
Hyperdynamic Circulation
Signup and view all the flashcards
Impact of Anemia on Circulation
Impact of Anemia on Circulation
Signup and view all the flashcards
Platelet Count with Age
Platelet Count with Age
Signup and view all the flashcards
Long-Term Impact of Anemia
Long-Term Impact of Anemia
Signup and view all the flashcards
Hereditary Spherocytosis
Hereditary Spherocytosis
Signup and view all the flashcards
Autosomal Dominant Inheritance
Autosomal Dominant Inheritance
Signup and view all the flashcards
Autosomal Recessive Inheritance
Autosomal Recessive Inheritance
Signup and view all the flashcards
Hemolytic Anemia
Hemolytic Anemia
Signup and view all the flashcards
Splenomegaly
Splenomegaly
Signup and view all the flashcards
Thalassemia
Thalassemia
Signup and view all the flashcards
Beta-thalassemia
Beta-thalassemia
Signup and view all the flashcards
Beta-thalassemia Minor
Beta-thalassemia Minor
Signup and view all the flashcards
Beta-thalassemia Major
Beta-thalassemia Major
Signup and view all the flashcards
Cooley's Anemia
Cooley's Anemia
Signup and view all the flashcards
Beta-thalassemia Trait (Carrier)
Beta-thalassemia Trait (Carrier)
Signup and view all the flashcards
Beta-thalassemia Intermedia
Beta-thalassemia Intermedia
Signup and view all the flashcards
Hemolysis
Hemolysis
Signup and view all the flashcards
Erythropoiesis
Erythropoiesis
Signup and view all the flashcards
Decreased RBC Production
Decreased RBC Production
Signup and view all the flashcards
Increased RBC Destruction
Increased RBC Destruction
Signup and view all the flashcards
Macrocytic Anemia
Macrocytic Anemia
Signup and view all the flashcards
Microcytic Anemia
Microcytic Anemia
Signup and view all the flashcards
Normocytic Anemia
Normocytic Anemia
Signup and view all the flashcards
Macrocytic MCV
Macrocytic MCV
Signup and view all the flashcards
Microcytic MCV
Microcytic MCV
Signup and view all the flashcards
Normocytic MCV
Normocytic MCV
Signup and view all the flashcards
MCV Assessment
MCV Assessment
Signup and view all the flashcards
G6PD Deficiency
G6PD Deficiency
Signup and view all the flashcards
Episodic Hemolytic Anemia
Episodic Hemolytic Anemia
Signup and view all the flashcards
Chronic Nonspherocytic Hemolytic Anemia
Chronic Nonspherocytic Hemolytic Anemia
Signup and view all the flashcards
G6PD Deficiency and Hemolytic Anemia
G6PD Deficiency and Hemolytic Anemia
Signup and view all the flashcards
Coca-Cola Urine
Coca-Cola Urine
Signup and view all the flashcards
Hemoglobin
Hemoglobin
Signup and view all the flashcards
Hematinuria
Hematinuria
Signup and view all the flashcards
Urobilinogen
Urobilinogen
Signup and view all the flashcards
Iron Deficiency Anemia
Iron Deficiency Anemia
Signup and view all the flashcards
Sickle Cell Anemia
Sickle Cell Anemia
Signup and view all the flashcards
Pain Crisis
Pain Crisis
Signup and view all the flashcards
Hemoglobin Levels
Hemoglobin Levels
Signup and view all the flashcards
Hydroxyurea
Hydroxyurea
Signup and view all the flashcards
Genetic Counseling
Genetic Counseling
Signup and view all the flashcards
Iron Deficiency Anemia Prevention
Iron Deficiency Anemia Prevention
Signup and view all the flashcards
What is thalassemia?
What is thalassemia?
Signup and view all the flashcards
What causes thalassemia?
What causes thalassemia?
Signup and view all the flashcards
How severe is thalassemia?
How severe is thalassemia?
Signup and view all the flashcards
What are the symptoms of thalassemia?
What are the symptoms of thalassemia?
Signup and view all the flashcards
How is thalassemia diagnosed?
How is thalassemia diagnosed?
Signup and view all the flashcards
What treatments are available for thalassemia?
What treatments are available for thalassemia?
Signup and view all the flashcards
Why is long-term management crucial for thalassemia?
Why is long-term management crucial for thalassemia?
Signup and view all the flashcards
How is thalassemia classified?
How is thalassemia classified?
Signup and view all the flashcards
What is beta-thalassemia?
What is beta-thalassemia?
Signup and view all the flashcards
What is the outlook for individuals with thalassemia?
What is the outlook for individuals with thalassemia?
Signup and view all the flashcards
Study Notes
Anemia in Children
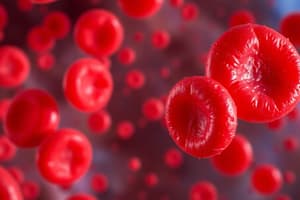
- Anemia is defined as a decrease in hemoglobin concentration or red blood cell (RBC) volume below healthy levels.
- Cord blood hemoglobin levels: 16.8 g/dL
- 2-week-old: 16.5 g/dL
- 3-month-old: 12.09 g/dL
- 6-month-to-6-year-old: 12.01 g/dL
- 7-12-year-old: 13.01 g/dL
Clinical presentations of Anemia
- General manifestations: pallor, sleepiness, irritability, weakness, decreased exercise tolerance.
- Flow murmur: often present in anemia.
- Shortness of breath on exertion, tachycardia, cardiac dilation, and high-output heart failure can occur. These stem from increasingly severe anemia, regardless of the underlying cause.
- The heart tries to compensate by increasing heart rate (HR) and cardiac output (CO), but this may lead to hyperdynamic circulation and, over time, heart failure.
Classification of Anemia
- Morphological classification: based on RBC size (mean corpuscular volume, MCV).
- Microcytic: <70 fL
- Normocytic: 70-90 fL
- Macrocytic: >90 fL
- Physiological classification: decreased RBC production or increased destruction.
- Decreased RBC production: ineffective erythropoiesis, failure of erythropoiesis
- Increased destruction: hemolysis (hyper-splenism), bleeding (blood loss)
Types of Anemia
- Microcytic anemia: iron deficiency anemia, thalassemias, lead poisoning, anemia of chronic disease, sideroblastic anemia
- Normocytic anemia: chronic disease, inflammation, anemia of aplastic, infection, drugs, malignancies, endocrinopathies (hypothyroidism), renal failure, acute bleeding
- Macrocytic anemia: vitamin B12 deficiency, folate deficiency, liver disease, hypothyroidism, other disorders (e.g., diamond-blackfan anemia, aplastic anemia, down syndrome)
Iron Deficiency Anemia (IDA)
- Most common cause of anemia in children.
- 15% frequency rate in children.
- Causes: increased demand, decreased intake, increased loss.
- Increased demand: growth spurts in children and infants, puberty
- Decreased intake: poor diet (inability to access sufficient nutrients), poor absorption (e.g., intolerance)
- Increased loss: GI bleeding, hemolysis, surgical procedures, worm infestation
Iron Absorption
- Enhanced by: orange juice, vitamin C, soy sauce, vinegar
- Inhibited by: tea, coffee, milk, phytate
Forms of Iron in the Body
- Iron in food: meat, beans, and vegetables
- Iron in storage: ferritin (liver, spleen, muscle, bone marrow), hemosiderin (excreted in urine)
- Iron in circulation: recycled from hemoglobin breakdown
Clinical Features of Iron Deficiency Anemia
- CNS manifestations: apathy, irritability, poor concentration, poor muscle tone, cognitive deficits, poor school performance
- Pica (pagophagia): persistent craving and compulsive eating of nonfood substances like ice
- Breath-holding spells: in children.
Oral Signs in Iron Deficiency Anemia (IDA)
- Koilonychia (spoon-shaped nails)
- Atrophic glossitis (beefy red tongue)
- Cheilosis (angular stomatitis)
- Plummer-Vinson syndrome: triad of IDA, esophageal webs, and dysphagia
Lab Findings in Anemia
- Low hemoglobin, low MCV, low MCHC, elevated RDW, microcytic hypochromic red blood cells, anisocytosis with target cells, teardrops, elliptical cells, and fragmented cells
- Increased platelets with normal morphology
Treatment of Anemia
- Oral iron therapy: 3-6 mg/kg/d, divided doses
- Iron therapy results in increased reticulocyte counts within 3-5 days, peaking between 5 and 7 days with increasing hemoglobin levels thereafter)
- Iron medication is continued for 8 weeks after blood values are normalized
- To restore iron stores
Congenital Hypoplastic Anemia (Diamond-Blackfan Anemia)
- Rare congenital bone marrow failure syndrome
- Usually becomes symptomatic in early infancy.
- More than 90% of cases are recognized within the first year of life.
- Characterized by macrocytic anemia, reticulocytopenia, and deficiency or absence of red blood cells (RBC) precursors in an otherwise normal cellular bone marrow.
Associated anomalies in Diamond-Blackfan Anemia
- Microcephaly, micrognathia
- Triphalangeal thumb, bifid thumb
- Heart defects (VSD, ASD, coarctation)
- Genitourinary tract anomalies (absence or horseshoe kidney, hypospadia)
- Short stature
Diagnosis of Diamond-Blackfan Anemia
- Complete blood count: very low number of red blood cells, low hemoglobin
- Low retic count
- Bone marrow sample (biopsy): few new red blood cells
Treatment of Diamond-Blackfan Anemia
- Prednisolone
- Androgens
- Antithymocyte globulin
- Transfusion
- Stem cell transplantation
Thalassemias
- Heterogenous group of inherited disorders characterized by reduced or absent globin chain synthesis.
- Imbalance will leads to ineffective erythropoiesis and shortened RBC lifespan.
Normal Hemoglobin (Hb) in Adults
- Hb A: 2α, 2β (more than 95%)
- Hb F: 2α, 2γ (less than 2.5%)
- Hb A2: 2α, 2δ (2-3.4%)
Beta-Thalassemia Major
- Characterized by severe microcytic, hypochromic anemia
- Detected early in childhood (after 6 months)
- Infants fail to thrive
- Pallor, variable jaundice, abdominal enlargement, hepatosplenomegaly.
- Marked bone changes (due to expansion of marrow space for increased erythropoiesis).
- Characteristic changes in skull, long bones and hand bones (crew-cut skull)
Sickle Cell Disease (SCD)
- Inherited red blood cell disorder
- Normal RBCs are round, move through small tubes to deliver oxygen
- Abnormal HbS polymerizes, forms rigid fibers, distorts RBCs into sickle shapes when deoxygenated
- Consequences: reduced RBC deformability, hemolysis, vaso-occlusion, ischemia and inflammation
Sickle Cell Anemia: Pathophysiology
- Molecular basis; substitution of valine for glutamic acid on beta-globin chain
- Consequences: reduced RBC deformability, hemolysis, vaso-occlusion, ischemia and inflammation.
- Chronic hemolytic anemia.
- Sickle cells adhere to endothelial cells and can activate inflammatory pathways, leading to tissue damage and organ dysfunction
Clinical Features of Pain Crisis
- Sudden onset of severe deep pain (bones, joints, chest, back, and abdomen)
- Pain lasting hours to days
- Accompanying symptoms: swelling, tenderness, fever (if infection is present), tachycardia
- Common sites: dactylitis, long bones (femur, humerus), ribs, and sternum
- Recurrent Crises: chronic pain, organ damage, and avascular necrosis.
G6PD Deficiency
- Deficiency of G6PD is the most common red cell enzyme defect leading to hemolytic anemia.
- X-linked recessive inheritance; high frequency in certain populations (African, Mediterranean, and Asian ancestry).
- Hundreds of G6PD variants are characterized.
G6PD Deficiency: Clinical Presentations
- Neonatal jaundice and episodic acute hemolytic anemia, often induced by infections, certain drugs (including fava beans), or other stressors
- Episodes of hemolysis are associated with pallor, jaundice, hemoglobinuria and sometimes cardiovascular compromise
- Children are asymptomatic between episodes of hemolysis.
- Dark-colored urine ("coca- cola colored urine") is a typical sign
G6PD Deficiency: Triggering Agents
- Medications: antibacterial (sulfonamides, trimethoprim, sulfamethoxazole, nalidixic acid, chloramphenicol, nitrofurantoin), antimalarials (primaquine, pamaquine, chloroquine, quinacrine)
- Chemicals: phenacetin, vitamin K analogs, methylene blue, probenecid, acetylsalicylic acid, phenazopyridine, phenylhydrazine, benzene, naphthalene
- Illness: diabetic acidosis
G6PD Deficiency: Diagnosis
- Fall in hemoglobin and hematocrit
- Free hemoglobin in plasma and urine
- Heinz bodies: precipitated hemoglobin within red blood cells
- Reticulocytosis: increased number of reticulocytes (immature red blood cells)
G6PD Deficiency: Prevention and Treatment
- Prevention of hemolysis is essential.
- Supportive care (e.g., blood transfusions) may be necessary in severe cases or when Hb is <7 g/dL.
- Discontinuing the causative oxidant agent is crucial for recovery.
Hereditary Spherocytosis
- Common inherited abnormality of the red blood cell (RBC) membrane.
- Usually transmitted as an autosomal dominant or less commonly autosomal recessive disorder.
- 25% of patients have no previous family history.
- De-novo mutations or undetected mild disease in parents
Hereditary Spherocytosis: Clinical Presentations
- Neonatal period: hyperbilirubinemia, potentially severe enough to require phototherapy or exchange transfusions.
- Features of anemia: splenomegaly
Hereditary Spherocytosis: Lab Findings
- Normochromic, normocytic anemia
- Hb maintained 6-9 gm/dL
- Spherocytosis (spherical red blood cells)
- Reticulocytosis elevated reticulocytes)
Hereditary Spherocytosis: Treatment
- Splenectomy: removal of spleen to relieve anemia symptoms
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.