Podcast
Questions and Answers
What is one important nursing consideration when using antidiarrheal medications?
What is one important nursing consideration when using antidiarrheal medications?
- They can cause constipation in all patients.
- They should be avoided in patients with severe dehydration. (correct)
- They should be given to all infants immediately.
- They are universally safe for all patients.
What is the primary mechanism of action for prokinetic agents like metoclopramide?
What is the primary mechanism of action for prokinetic agents like metoclopramide?
- They block action of norepinephrine.
- They inhibit GI smooth muscle contraction.
- They augment acetylcholine, increasing upper GI motility. (correct)
- They increase gastric acid production.
What common adverse effect is associated with prolonged use of antidiarrheal medications?
What common adverse effect is associated with prolonged use of antidiarrheal medications?
- Decreased heart rate.
- Electrolyte imbalance. (correct)
- Enhanced hydration.
- Increased appetite.
At what age does control of bowel movements typically begin in toddlers?
At what age does control of bowel movements typically begin in toddlers?
Which of the following is NOT part of a physical examination for gastrointestinal issues?
Which of the following is NOT part of a physical examination for gastrointestinal issues?
What should patients do if diarrhea does not improve within two days?
What should patients do if diarrhea does not improve within two days?
What percentage of older adults are expected to experience constipation?
What percentage of older adults are expected to experience constipation?
What condition might lead to the use of prokinetic agents?
What condition might lead to the use of prokinetic agents?
Which of the following is a common adverse effect of anticholinergic medications?
Which of the following is a common adverse effect of anticholinergic medications?
What is the primary action of anticholinergics in urinary management?
What is the primary action of anticholinergics in urinary management?
Which diagnostic test allows for direct visualization of the bladder wall?
Which diagnostic test allows for direct visualization of the bladder wall?
Which of the following nursing interventions is essential for managing urinary incontinence?
Which of the following nursing interventions is essential for managing urinary incontinence?
What is the mechanism of action of cholinergic medications such as bethanechol?
What is the mechanism of action of cholinergic medications such as bethanechol?
Which condition would contraindicate the use of anticholinergics?
Which condition would contraindicate the use of anticholinergics?
Which of the following is an example of a pharmacologic therapy that may be indicated for severe urinary conditions?
Which of the following is an example of a pharmacologic therapy that may be indicated for severe urinary conditions?
What should be monitored in a patient receiving cholinergic drugs due to potential adverse effects?
What should be monitored in a patient receiving cholinergic drugs due to potential adverse effects?
What should the bladder capacity typically simulate to trigger the stretch receptors?
What should the bladder capacity typically simulate to trigger the stretch receptors?
What could be a consequence of excessive intake of spicy foods?
What could be a consequence of excessive intake of spicy foods?
What is a characteristic of oliguria?
What is a characteristic of oliguria?
Which factor does NOT influence bowel elimination?
Which factor does NOT influence bowel elimination?
What defines dysuria?
What defines dysuria?
Which condition involves the inability to sense the feeling to urinate?
Which condition involves the inability to sense the feeling to urinate?
Which term describes the production of excessively large amounts of urine?
Which term describes the production of excessively large amounts of urine?
What is a potential result of diverticulitis?
What is a potential result of diverticulitis?
Which of the following is NOT a risk factor for bladder and bowel elimination issues?
Which of the following is NOT a risk factor for bladder and bowel elimination issues?
What condition results in liquid feces with increased frequency?
What condition results in liquid feces with increased frequency?
What is the mechanism of action (MOA) for stool softeners/surfactant laxatives like docusate sodium?
What is the mechanism of action (MOA) for stool softeners/surfactant laxatives like docusate sodium?
What potential adverse effect can occur with prolonged use of stool softeners?
What potential adverse effect can occur with prolonged use of stool softeners?
Which of the following is an example of a stimulant laxative?
Which of the following is an example of a stimulant laxative?
Why should stimulant laxatives not be used with bowel obstruction?
Why should stimulant laxatives not be used with bowel obstruction?
What is a key nursing consideration for osmotic laxatives like magnesium hydroxide?
What is a key nursing consideration for osmotic laxatives like magnesium hydroxide?
What is a common side effect of stimulant laxatives?
What is a common side effect of stimulant laxatives?
What can happen if osmotic laxatives are taken within 1 hour of milk or antacids?
What can happen if osmotic laxatives are taken within 1 hour of milk or antacids?
What is the recommended time frame for a bowel movement to occur after using stool softeners?
What is the recommended time frame for a bowel movement to occur after using stool softeners?
What should be avoided in older adults to minimize health risks?
What should be avoided in older adults to minimize health risks?
What is a potential risk during dialysis?
What is a potential risk during dialysis?
What is the initial voiding characteristic in newborns?
What is the initial voiding characteristic in newborns?
What factors can significantly affect bowel elimination?
What factors can significantly affect bowel elimination?
Which statement about diverticula disease is accurate?
Which statement about diverticula disease is accurate?
What dietary recommendation can aid in reducing bowel elimination issues?
What dietary recommendation can aid in reducing bowel elimination issues?
What condition might result from the presence of excess gas in the intestines?
What condition might result from the presence of excess gas in the intestines?
What is the expected change in glomerular filtration rate (GFR) for newborns?
What is the expected change in glomerular filtration rate (GFR) for newborns?
What defines nocturnal enuresis in children?
What defines nocturnal enuresis in children?
Which of the following factors can lead to diarrhea?
Which of the following factors can lead to diarrhea?
What potential complication arises from diverticula inflammation?
What potential complication arises from diverticula inflammation?
What does the term 'persistence of liquid feces' indicate?
What does the term 'persistence of liquid feces' indicate?
In older adults, what happens to renal function as they age?
In older adults, what happens to renal function as they age?
What impact does fluid intake have on bowel elimination?
What impact does fluid intake have on bowel elimination?
Flashcards are hidden until you start studying
Study Notes
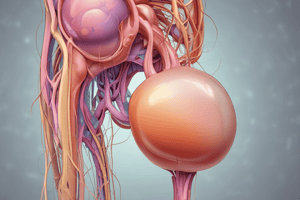
Bladder Elimination
- Normal bladder elimination: 250-400 mL of urine, voluntary control, intact nerve conduction
Factors Affecting Bladder Elimination
- Fluid and food intake
- Muscle tone
- Surgical and diagnostic procedures
- Medications
Risk Factors for Bladder Elimination Issues
- Age
- Arteriosclerosis, chronic conditions, surgery, genetics
Alterations in Bladder Elimination
- Polyuria: production of abnormally large amounts of urine
- Polydipsia: compulsive intake of excessive amounts of fluid
- Anuria: less than 100 mL a day (no urine)
- Oliguria: less than 400 mL a day (low urine output)
- Frequency: urinating often
- Urgency: strong urge to urinate
- Nocturia: urinating 2 or more times a night
- Dysuria: trouble urinating
- Hesitancy: hesitating to urinate
- Neurogenic bladder: unable to sense the feeling to urinate
Observation and Patient Interview
- Look for: anxiety, odor, absorbent items
- Voiding pattern: frequency, volume, color of urine, pain, issues with voiding
- Investigate other factors influencing urinary elimination
Physical Examination
- Palpation of abdomen
- Flank pain
- Skin turgor
- Inspection of any urine or fecal material
- Genitalia
Diagnostic Tests
- Urine studies: culture, sensitivity, urinalysis
- Bladder scan: evaluates bladder emptying
- Radiologic examinations: retrograde pyelography
- Cystoscopy: allows for direct visualization of bladder wall
- Imaging: KUB radiograph, CT, MRI, US, etc.
- Kidney biopsy
Independent Nursing Interventions
- Monitoring intake and output
- Catheter care
- Incontinence care
- Urine specimen collection
- Patient teaching
Collaborative Therapies
- Treatment team can consist of many members
- Referrals may need to be made
- Pharmacologic therapy can be initiated
- Dialysis can be used for severe injury or disease progression
Anticholinergics (Muscarinic Antagonists)
- Examples: oxybutynin
- MOA: blocks receptors in the detrusor muscle of the bladder preventing contractions, and the urge to void
- Adverse effects: blurred vision, constipation, dry mouth, anhidrosis, photophobia, dry eyes, tachycardia, hallucinations, confusion
- Nursing considerations: contraindicated in patients with urinary retention, GI obstruction
Cholinergics (Muscarinic Agonists)
- Examples: bethanechol
- MOA: Stimulates bladder contraction, and assists with voiding
- Adverse effects: cramping, other GI symptoms, diaphoresis, headache, nausea, bradycardia, hypotension, bronchoconstriction
- Nursing considerations: do not give patients with GI or urinary tract obstruction, asthma, bradycardia, hypotension, or Parkinson Disease.
Bowel Elimination
- Normal bowel elimination: soft, formed stool; frequency is individualized
- Diet should include fiber
- Irregular eating patterns can alter bowel elimination patterns
- Spicy foods and high sugars can lead to diarrhea
- Activity and pain can also impact bowel elimination
Factors Affecting Bowel Elimination
- Fluid and food intake
- Activity
- Pain
- Medications
Risk Factors for Bowel Elimination Issues
- Age
- Sex
- Chronic illness
- Immobility
Alterations in Bowel Elimination
- Diarrhea: passage of liquid feces with increased frequency, results in loss of fluid can lead to dehydration
- Flatulence: presence of excess gas leading to inflation and bloating
- Diverticulitis: results from inflamed diverticula can obstruct bowel
- Bowel obstruction: occurs when the contents of the intestine are unable to move through the intestine
Observation and Patient Interview
- Look for any anxiety, odor and any absorbent items
- Defecation pattern: frequency, consistency of stool, pain
- Investigate other factors influencing defecation: diet, exercise, medications, stress, ostomy
Physical examination
- Auscultate, palpate, percuss
- Inspect abdomen, gently palpate abdomen (be careful with pressure)
Diagnostic Tests
- Blood and fecal tests
- Endoscopy
- Biopsy
- Imaging (e.g. KUB radiograph, CT scan, MRI, etc.)
Newborns and Infants
- Meconium is the first stool passed, which is thick and tarry
- Immature intestines can lead to difficult stool passage
Toddlers
- Control of bowel elimination generally starts around 2-3 years old
School-Age Children/Adolescents
- Bowel elimination should be under control by this age
Pregnant Women
- Hormonal changes can impact bowel elimination
- Progesterone can lead to sluggish bowel elimination
- Enlarging uterus puts pressure on the bowels
- Increased gastric reflux
- Hemorrhoids can develop
- Postpartum risks also exist
Older Adults
- Nearly all experience constipation
- Poor intake, reduced activity, and medications contribute to constipation
- Declining renal function
- Inability to concentrate urine
Antidiarrheal Medications
- Examples: loperamide
- MOA: blocks action of acetylcholine, slowing motility of intestines
- Adverse effects: electrolyte imbalance with prolonged use
- Nursing considerations: avoid use with patients who have severe dehydration, liver or renal disorders, or glaucoma
Prokinetic Agents
- Examples: metoclopramide
- MOA: augments acetylcholine, increasing upper GI motility and peristalsis
- Adverse effects: tardive dyskinesia, extrapyramidal symptoms, restlessness, anxiety, sedation, diarrhea, increased seizure risk
- Nursing considerations: use cautiously with older adults and children, don’t use with bowel obstruction, perforation or hemorrhage
Stool Softeners/Surfactants (Laxatives)
- Examples: docusate sodium
- MOA: lowers surface tension of stool allowing water to penetrate, soften, and allow for easier passing of stool
- Adverse effects: electrolyte imbalance with prolonged use
- Nursing considerations: bowel movement should occur within 3 days, don’t use with bowel obstruction
Osmotic Laxatives
- Examples: magnesium hydroxide, lactulose
- MOA: draws water into the intestine, increasing the mass of stool and causing peristalsis
- Adverse effects: abdominal cramping, diarrhea, fluid and electrolyte imbalance, dehydration
- Nursing considerations: bowel movement should occur within 3 days, can interact with some antibiotics
Stimulant Laxatives (Cathartics)
- Examples: bisacodyl, senna
- MOA: stimulates intestinal peristalsis and increases the volume of water and electrolytes in the intestine
- Adverse effects: stomach discomfort, nausea, diarrhea, cramps, fluid and electrolyte loss
- Nursing considerations: bowel movement should occur within 12 hours, don't take with milk or antacid, avoid if bowel obstruction
Bulk-Forming Laxatives
- Examples: psyllium
- MOA: supplemental fiber to soften stool
- Adverse effects: potential for gas and abdominal bloating
- Nursing considerations: drink plenty of fluids with this type of laxative, do not use with bowl obstruction or narrowing of the bowel
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.