Podcast
Questions and Answers
What is the primary function of the trophoblastic layer during embryonic development?
What is the primary function of the trophoblastic layer during embryonic development?
- To form the three primary germ layers
- To develop into the chorion (correct)
- To develop into the embryo
- To undergo rapid mitotic divisions
What is the name of the process during which the zygote undergoes a series of rapid mitotic divisions?
What is the name of the process during which the zygote undergoes a series of rapid mitotic divisions?
- Implantation
- Gastrulation
- Cleavage (correct)
- Fertilization
What is the primary function of the corpus luteum during embryonic development?
What is the primary function of the corpus luteum during embryonic development?
- To form the blastocyst
- To undergo gastrulation
- To develop into the embryo
- To secrete progesterone and some estrogen (correct)
During which stage of embryonic development does the embryo undergo a reorganization into germ layers?
During which stage of embryonic development does the embryo undergo a reorganization into germ layers?
What is the name of the structure that forms from the inner cell mass during embryonic development?
What is the name of the structure that forms from the inner cell mass during embryonic development?
Approximately how many days after fertilization does implantation typically occur?
Approximately how many days after fertilization does implantation typically occur?
What is the primary function of the inner cell mass during embryonic development?
What is the primary function of the inner cell mass during embryonic development?
Which layer of the blastocyst is responsible for the formation of the placenta and associated structures?
Which layer of the blastocyst is responsible for the formation of the placenta and associated structures?
What are the layers of the blastocyst?
What are the layers of the blastocyst?
What are the three primary germ layers that form during embryonic development?
What are the three primary germ layers that form during embryonic development?
Which germ layer is responsible for forming the skin and the nervous system?
Which germ layer is responsible for forming the skin and the nervous system?
Through which structure does the mother's blood supply nutrients and oxygen to the fetus?
Through which structure does the mother's blood supply nutrients and oxygen to the fetus?
What is the primary route by which fetal waste products are removed?
What is the primary route by which fetal waste products are removed?
Which component of the placenta arises from the trophoblast?
Which component of the placenta arises from the trophoblast?
What function do the chorionic villi perform in the placenta?
What function do the chorionic villi perform in the placenta?
What is fertilization?
What is fertilization?
What are Steroids?
What are Steroids?
Which type of hormone directly affects gene expression without a second messenger system?
Which type of hormone directly affects gene expression without a second messenger system?
Which type of hormones require a second messenger system?
Which type of hormones require a second messenger system?
What is the potential consequence of a tumor in the hypothalamus or pituitary gland?
What is the potential consequence of a tumor in the hypothalamus or pituitary gland?
What is the primary mechanism of action of protein hormones?
What is the primary mechanism of action of protein hormones?
Which of the following best describes monoamines?
Which of the following best describes monoamines?
Where Are the Posterior Pituitary Hormones Produced?
Where Are the Posterior Pituitary Hormones Produced?
Which of the following lists contains only hormones secreted by the anterior pituitary gland?
Which of the following lists contains only hormones secreted by the anterior pituitary gland?
What is the common feature of FSH, LH, ACTH, TSH, PRL, and GH?
What is the common feature of FSH, LH, ACTH, TSH, PRL, and GH?
What is the relationship between the hypothalamus and the posterior pituitary gland?
What is the relationship between the hypothalamus and the posterior pituitary gland?
Which two hormones are secreted from the posterior pituitary gland?
Which two hormones are secreted from the posterior pituitary gland?
What type of hormone typically interacts with its target cells by binding to receptors on the cell membrane and activating a second messenger system?
What type of hormone typically interacts with its target cells by binding to receptors on the cell membrane and activating a second messenger system?
Which hormone is classified as a peptide/protein hormone and is lipid-insoluble?
Which hormone is classified as a peptide/protein hormone and is lipid-insoluble?
Which characteristic is shared by both peptides/proteins and monoamines, but not by steroids?
Which characteristic is shared by both peptides/proteins and monoamines, but not by steroids?
Which hormone is likely to bind to intracellular receptors and affect gene expression directly?
Which hormone is likely to bind to intracellular receptors and affect gene expression directly?
How do protein hormones typically interact with their target cells?
How do protein hormones typically interact with their target cells?
Which of the following hormones is derived from cholesterol and is lipid-soluble?
Which of the following hormones is derived from cholesterol and is lipid-soluble?
What is a characteristic of peptide/protein hormones in terms of hormone classification?
What is a characteristic of peptide/protein hormones in terms of hormone classification?
Which of the following hormones would bind to receptors on the cell membrane and directly affect gene expression without a second messenger system?
Which of the following hormones would bind to receptors on the cell membrane and directly affect gene expression without a second messenger system?
Which of the following hormones are secreted by the thyroid gland, and what are their primary functions?
Which of the following hormones are secreted by the thyroid gland, and what are their primary functions?
What is the mechanism of action of steroid hormones?
What is the mechanism of action of steroid hormones?
Which statement correctly describes Graves’ disease?
Which statement correctly describes Graves’ disease?
What happens if you have too much growth hormone before puberty?
What happens if you have too much growth hormone before puberty?
Which hormone secreted by the thyroid gland lowers blood calcium levels?
Which hormone secreted by the thyroid gland lowers blood calcium levels?
What is the characteristic feature of Graves' disease?
What is the characteristic feature of Graves' disease?
What is the cause of thyroid imbalance in Graves' disease?
What is the cause of thyroid imbalance in Graves' disease?
What is the result of having too much growth hormone after puberty?
What is the result of having too much growth hormone after puberty?
What is the stage of cell division of the egg when ovulated?
What is the stage of cell division of the egg when ovulated?
Which of the following hormones are secreted by the thyroid gland, and what are their primary functions?
Which of the following hormones are secreted by the thyroid gland, and what are their primary functions?
What are the three types of hormones secreted from the adrenal cortex?
What are the three types of hormones secreted from the adrenal cortex?
What are the symptoms of cretinism?
What are the symptoms of cretinism?
What mineral is necessary to produce thyroid hormones?
What mineral is necessary to produce thyroid hormones?
What hormone is increased during stress and is also anti-inflammatory?
What hormone is increased during stress and is also anti-inflammatory?
What Is an Endemic Goiter?
What Is an Endemic Goiter?
What Causes Hypothyroidism?
What Causes Hypothyroidism?
What Is Myxedema?
What Is Myxedema?
What is the Function of the Parathyroid Hormones and How Do They Regulate Calcium?
What is the Function of the Parathyroid Hormones and How Do They Regulate Calcium?
What Is Myxedema?
What Is Myxedema?
What is the primary cause of hypothyroidism in adults?
What is the primary cause of hypothyroidism in adults?
What is the primary function of mineralocorticoids?
What is the primary function of mineralocorticoids?
What is the characteristic feature of Cushing's disease?
What is the characteristic feature of Cushing's disease?
What is the primary function of parathyroid hormone (PTH)?
What is the primary function of parathyroid hormone (PTH)?
What is the primary cause of cretinism?
What is the primary cause of cretinism?
Which of the following correctly matches the types of hormones secreted from the adrenal cortex with their primary functions?
Which of the following correctly matches the types of hormones secreted from the adrenal cortex with their primary functions?
Which of the following are common symptoms of Cushing's disease?
Which of the following are common symptoms of Cushing's disease?
Which hormones are produced by the adrenal medulla?
Which hormones are produced by the adrenal medulla?
Which hormone is produced in the beta cells of the pancreas?
Which hormone is produced in the beta cells of the pancreas?
Where is epinephrine produced?
Where is epinephrine produced?
Which hormone is produced in the alpha cells of the pancreas?
Which hormone is produced in the alpha cells of the pancreas?
Which of the following endocrine glands is primarily responsible for regulating sleep cycles through the secretion of melatonin?
Which of the following endocrine glands is primarily responsible for regulating sleep cycles through the secretion of melatonin?
What is the result of hyposecretion of hormones?
What is the result of hyposecretion of hormones?
Which endocrine gland is involved in the maturation of T-cells and diminishes in function with age?
Which endocrine gland is involved in the maturation of T-cells and diminishes in function with age?
What is the result of hypersecretion of hormones?
What is the result of hypersecretion of hormones?
What is the function of the pancreas in regulating hormone levels?
What is the function of the pancreas in regulating hormone levels?
What is the primary effect of insulin on blood glucose levels?
What is the primary effect of insulin on blood glucose levels?
What is the main characteristic of NIDDM (Type 2 Diabetes)?
What is the main characteristic of NIDDM (Type 2 Diabetes)?
What is the function of glucagon?
What is the function of glucagon?
What is the primary treatment for IDDM (Type 1 Diabetes)?
What is the primary treatment for IDDM (Type 1 Diabetes)?
What is the underlying mechanism of IDDM (Type 1 Diabetes)?
What is the underlying mechanism of IDDM (Type 1 Diabetes)?
What is the primary function of insulin in the body?
What is the primary function of insulin in the body?
What is the characteristic of Type 1 Diabetes?
What is the characteristic of Type 1 Diabetes?
What is the function of glucagon in the body?
What is the function of glucagon in the body?
What is the characteristic of Type 2 Diabetes?
What is the characteristic of Type 2 Diabetes?
What is the relationship between insulin and glucagon in the body?
What is the relationship between insulin and glucagon in the body?
What is the effect of stimulating glycogenolysis and gluconeogenesis in the liver?
What is the effect of stimulating glycogenolysis and gluconeogenesis in the liver?
What is the primary source of glucose in the liver during glycogenolysis?
What is the primary source of glucose in the liver during glycogenolysis?
What is the net effect of gluconeogenesis on blood glucose levels?
What is the net effect of gluconeogenesis on blood glucose levels?
What is the opposite effect of stimulating glycogenolysis and gluconeogenesis in the liver?
What is the opposite effect of stimulating glycogenolysis and gluconeogenesis in the liver?
What is the primary function of glycogenolysis and gluconeogenesis in the liver during fasting or starvation?
What is the primary function of glycogenolysis and gluconeogenesis in the liver during fasting or starvation?
Study Notes
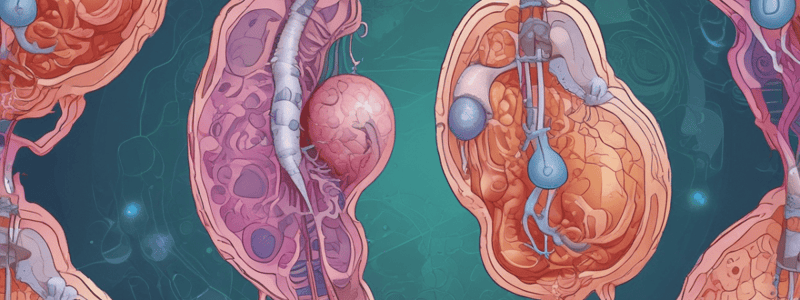
Fertilization and Cleavage
- Fertilization is the process where a sperm cell and an egg cell (oocyte) merge to form a zygote.
- Cleavage is a series of rapid mitotic divisions that the zygote undergoes, leading to the formation of a multicellular embryo.
Layers of the Blastocyst
- The blastocyst consists of two main layers: the inner cell mass and the trophoblast.
- The inner cell mass develops into the embryo.
- The trophoblast develops into the placenta and associated structures.
Implantation
- Implantation typically occurs about 6-10 days after fertilization.
Hormone Regulation
- The corpus luteum secretes progesterone (and some estrogen) until the placenta develops and takes over hormone production.
Fate of the Blastocyst Layers
- The inner cell mass develops into the embryo.
- The trophoblastic layer develops into the chorion, part of the placenta.
Gastrulation
- Gastrulation is a process during embryonic development that reorganizes the embryo into a layered structure, forming three primary germ layers.
The Three Germ Layers
- The three primary germ layers are: ectoderm, mesoderm, and endoderm.
Layers of the Blastocyst
- The blastocyst consists of two main layers.
- The inner cell mass develops into the embryo.
- The trophoblast develops into the placenta and associated structures.
Placenta Formation
- The chorionic villi, arising from the trophoblast, form the fetal portion of the placenta
Nutrient and Waste Transport
- The placenta facilitates the exchange of nutrients and waste between the mother and fetus
- The mother's blood supplies nutrients and oxygen to the fetus through the placenta
- Fetal waste products are removed through the mother's circulatory system via the placenta
Classification of Hormones
- Steroids: derived from cholesterol, lipid-soluble (e.g., cortisol, estrogen, testosterone)
- Peptides/Proteins: made of amino acids, water-soluble (e.g., insulin, growth hormone)
- Monoamines: derived from amino acids, water-soluble (e.g., epinephrine, norepinephrine, thyroid hormones)
Mechanism of Action of Hormones
Protein Hormones
- Bind to receptors on the cell membrane
- Require a second messenger system (e.g., cAMP) to relay the signal inside the cell
Steroid Hormones
- Pass through the cell membrane and bind to intracellular receptors
- Directly affect gene expression without a second messenger
Hormones Secreted by the Hypothalamus
- TRH, CRH, GnRH, GHRH, PIH, Somatostatin, Oxytocin, ADH
Hormones Secreted by the Anterior Pituitary Gland
- FSH, LH, ACTH, TSH, PRL, GH
Hormones Secreted by the Posterior Pituitary Gland
- Oxytocin, ADH (Vasopressin)
- Produced in the hypothalamus and stored and released by the posterior pituitary gland
Effects of Tumors in the Hypothalamus or Pituitary Gland
- Can lead to hyposecretion or hypersecretion of hormones
- Affects growth, metabolism, and other bodily functions
- Specific effects depend on the hormones involved
Hormones of the Anterior Pituitary Gland
- FSH (Follicle-Stimulating Hormone) is secreted from the anterior pituitary gland
- LH (Luteinizing Hormone) is secreted from the anterior pituitary gland
- ACTH (Adrenocorticotropic Hormone) is secreted from the anterior pituitary gland
- TSH (Thyroid-Stimulating Hormone) is secreted from the anterior pituitary gland
- PRL (Prolactin) is secreted from the anterior pituitary gland
- GH (Growth Hormone) is secreted from the anterior pituitary gland
Hormones of the Posterior Pituitary Gland
- Oxytocin is secreted from the posterior pituitary gland
- ADH (Vasopressin) is secreted from the posterior pituitary gland
Production of Posterior Pituitary Hormones
- Posterior pituitary hormones are produced in the hypothalamus
- Posterior pituitary hormones are stored and released by the posterior pituitary gland
Steroids
- Derived from cholesterol and are lipid-soluble
- Examples include cortisol, estrogen, and testosterone
- Pass through the cell membrane and bind to intracellular receptors, directly affecting gene expression without a second messenger
Peptides/Proteins
- Made of amino acids and are water-soluble
- Examples include insulin and growth hormone
- Bind to receptors on the cell membrane and activate a second messenger system
- Classified as hormones that interact with their target cells by binding to receptors on the cell membrane and activating a second messenger system
Monoamines
- Derived from amino acids and are water-soluble
- Examples include epinephrine and norepinephrine
- Classified as hormones that interact with their target cells by binding to receptors on the cell membrane and activating a second messenger system
Hormone Classification
- Shared characteristic of peptides/proteins and monoamines: water-solubility
- Steroids are derived from cholesterol and are lipid-soluble, whereas peptides/proteins and monoamines are derived from amino acids and are water-soluble
Growth Hormone
- Excessive growth hormone before puberty leads to Gigantism, characterized by excessive growth.
- Excessive growth hormone after puberty leads to Acromegaly, characterized by enlarged bones in hands, feet, and face.
Thyroid Hormone (TH)
- TH includes T3 and T4, which regulate metabolism, growth, and development.
- Thyroid gland functions also include the secretion of Calcitonin, which lowers blood calcium levels.
Hyperthyroidism
- Hyperthyroidism is caused by the overproduction of thyroid hormones, often due to Graves' disease or thyroid nodules.
- Graves' disease is an autoimmune disorder that leads to hyperthyroidism, characterized by goiter, exophthalmos, and other symptoms.
- In Graves' disease, autoantibodies mimic TSH, stimulating excessive thyroid hormone production.
Oogenesis
- Meiosis I is the type of cell division that occurs when a primary oocyte divides to become a secondary oocyte.
- At the completion of meiosis I, one secondary oocyte and one polar body are produced.
- The secondary oocyte is released during ovulation, paused in Metaphase II of meiosis.
Ovulation and Corpus Luteum
- After ovulation, the tissue that surrounds the oocyte transforms into the corpus luteum.
- The corpus luteum is a temporary endocrine structure that secretes progesterone and estrogen.
Hormones and Phases of Menstrual Cycle
- Estrogen causes thickening of the uterine lining during the proliferative phase.
- Progesterone causes thickening of the uterine lining during the secretory phase.
- Rising levels of LH (Luteinizing hormone) stimulate ovulation.
- Ovulation typically occurs on day 14 of a 28-day cycle.
Menstrual Cycle Phases
- Menses ( menstrual bleeding) occurs on days 1-5 of the menstrual cycle.
- The proliferative phase occurs on days 6-14, ending with ovulation.
- The follicular phase occurs from day 1 to day 14 of the menstrual cycle.
Hormonal Maintenance and Decline
- Progesterone and estrogen are necessary to maintain the uterine lining in preparation for embryo implantation.
- A decline in progesterone and estrogen levels leads to the shedding of the functionalis layer of the endometrium.
FSH Function
- FSH (Follicle-stimulating hormone) stimulates the growth of ovarian follicles.
Thyroid Disorders
- Endemic goiter is a thyroid enlargement caused by iodine deficiency, leading to insufficient thyroid hormone production.
- Iodine is a necessary mineral for producing thyroid hormones.
Hypothyroidism
- Hypothyroidism is a condition characterized by insufficient production of thyroid hormones.
- Causes of hypothyroidism include Hashimoto's thyroiditis, iodine deficiency, and other factors.
Myxedema
- Myxedema is a severe form of hypothyroidism in adults, characterized by swelling, especially in the face and extremities.
Cretinism
- Cretinism is a condition caused by congenital hypothyroidism.
- Symptoms of cretinism include stunted physical and mental growth.
Parathyroid Hormones
- Parathyroid hormones (PTH) regulate calcium levels by stimulating bone resorption, increasing calcium reabsorption in the kidneys, and activating vitamin D.
Adrenal Cortex Hormones
- Mineralocorticoids (e.g., aldosterone) regulate electrolyte and water balance.
- Glucocorticoids (e.g., cortisol) regulate metabolism and stress response.
- Androgens are sex hormones.
Cortisol
- Cortisol is increased during stress and has anti-inflammatory properties.
Cushing's Disease
- Cushing's disease is a condition caused by excessive cortisol production or exposure to high levels of cortisol.
- Causes of Cushing's disease include pituitary adenoma, ectopic ACTH production, or long-term corticosteroid therapy.
- Symptoms of Cushing's disease include weight gain, thinning skin, hypertension, and glucose intolerance.
Cushing's Disease
- Cushing's disease is caused by three main factors: pituitary adenoma, ectopic ACTH production, or long-term corticosteroid therapy.
Symptoms of Cushing's Disease
- Weight gain is a key symptom of Cushing's disease.
- Thinning skin is another common symptom.
- Hypertension is a symptom of Cushing's disease.
- Glucose intolerance is a symptom of Cushing's disease.
Adrenal Medulla Hormones
- The adrenal medulla produces two essential hormones: Epinephrine and Norepinephrine.
Epinephrine Production
- Epinephrine is produced in the adrenal medulla.
Other Endocrine Glands and Their Functions
- Pineal Gland: Regulates sleep cycles through melatonin production
- Thymus: Involved in T-cell maturation, but its function diminishes with age
- Pancreas: Regulates blood glucose levels
Disorders of Other Endocrine Glands
- Pineal Gland: Disorders include sleep disturbances
- Pancreas: Disorders include diabetes mellitus
How Hormone Imbalance Affects Hormone Levels
Hyposecretion (Hormone Deficiency)
- Leads to deficiency symptoms, such as:
- Hypothyroidism
- Adrenal insufficiency
Hypersecretion (Hormone Excess)
- Leads to excess symptoms, such as:
- Hyperthyroidism
- Cushing's syndrome
Diabetes
- IDDM (Type 1 Diabetes) is characterized by autoimmune destruction of beta cells, requiring insulin replacement.
- NIDDM (Type 2 Diabetes) is marked by insulin resistance and can be managed through diet, exercise, and sometimes medication.
Insulin and Glucagon Functions
- Insulin lowers blood glucose levels by facilitating cellular uptake of glucose.
- Glucagon raises blood glucose levels by stimulating glycogenolysis and gluconeogenesis in the liver.
Diabetes
- IDDM (Type 1 Diabetes) is characterized by autoimmune destruction of beta cells, requiring insulin replacement.
- NIDDM (Type 2 Diabetes) is marked by insulin resistance and can be managed through diet, exercise, and sometimes medication.
Insulin and Glucagon Functions
- Insulin lowers blood glucose levels by facilitating cellular uptake of glucose.
- Glucagon raises blood glucose levels by stimulating glycogenolysis and gluconeogenesis in the liver.
Glucagon's Effect on Blood Glucose Levels
- Increases blood glucose levels by stimulating two key processes in the liver: glycogenolysis and gluconeogenesis.
- Glycogenolysis is the breakdown of glycogen, a complex carbohydrate stored in the liver, into glucose.
- Gluconeogenesis is the generation of new glucose molecules from non-carbohydrate sources, such as amino acids and lactate.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the reproductive process in biology, including fertilization, cleavage, and the formation of a blastocyst.