Podcast
Questions and Answers
What is the most common cause of facial paralysis?
What is the most common cause of facial paralysis?
- Stroke
- Bell's palsy (correct)
- Lyme disease
- Tumors
Which cranial nerve is primarily affected in Bell's palsy?
Which cranial nerve is primarily affected in Bell's palsy?
- CN IX (Glossopharyngeal nerve)
- CN VII (Facial nerve) (correct)
- CN X (Vagus nerve)
- CN V (Trigeminal nerve)
What percentage of Bell's palsy cases experience incomplete recovery?
What percentage of Bell's palsy cases experience incomplete recovery?
- 10%
- 50%
- 70%
- 30% (correct)
Early treatment with corticosteroids for Bell's palsy aims to:
Early treatment with corticosteroids for Bell's palsy aims to:
Which of the following is a typical symptom of Bell's palsy?
Which of the following is a typical symptom of Bell's palsy?
What is believed to be the primary cause of Bell's palsy?
What is believed to be the primary cause of Bell's palsy?
Which of the following viruses is most commonly associated with Bell's palsy?
Which of the following viruses is most commonly associated with Bell's palsy?
Which of the following conditions is NOT listed as a risk factor for Bell's palsy?
Which of the following conditions is NOT listed as a risk factor for Bell's palsy?
What finding on physical examination helps differentiate Bell's palsy from a central cause of facial weakness, such as stroke?
What finding on physical examination helps differentiate Bell's palsy from a central cause of facial weakness, such as stroke?
According to the provided information, what percentage of patients with Bell's palsy typically achieve full recovery within 6 months?
According to the provided information, what percentage of patients with Bell's palsy typically achieve full recovery within 6 months?
Which diagnostic study assesses the severity of nerve damage and potential for recovery in Bell's palsy?
Which diagnostic study assesses the severity of nerve damage and potential for recovery in Bell's palsy?
First-line treatment for Bell's Palsy typically involves:
First-line treatment for Bell's Palsy typically involves:
Besides corticosteroids, which of the following medications might be prescribed for Bell's palsy if a viral etiology is suspected?
Besides corticosteroids, which of the following medications might be prescribed for Bell's palsy if a viral etiology is suspected?
According to the provided information, under which circumstance should antivirals be considered in conjunction with glucocorticoids for the treatment of Bell's palsy?
According to the provided information, under which circumstance should antivirals be considered in conjunction with glucocorticoids for the treatment of Bell's palsy?
A patient presents with Bell's Palsy classified as House-Brackmann Grade IV. According to the information, which factor would suggest a high risk stratification for this patient?
A patient presents with Bell's Palsy classified as House-Brackmann Grade IV. According to the information, which factor would suggest a high risk stratification for this patient?
Flashcards
Bell's Palsy Definition
Bell's Palsy Definition
Acute, idiopathic facial nerve palsy (CN VII) causing unilateral facial weakness or paralysis.
Bell's Palsy Etiology
Bell's Palsy Etiology
Inflammation and compression of the facial nerve, often linked to viral reactivation like HSV-1.
Bell's Palsy Incidence
Bell's Palsy Incidence
15-30 cases per 100,000 annually. Higher rates in pregnancy and individuals with diabetes.
Diabetes as a Risk Factor
Diabetes as a Risk Factor
Signup and view all the flashcards
Pregnancy as a Risk Factor
Pregnancy as a Risk Factor
Signup and view all the flashcards
Unilateral Facial Weakness
Unilateral Facial Weakness
Signup and view all the flashcards
Lagophthalmos
Lagophthalmos
Signup and view all the flashcards
Hyperacusis
Hyperacusis
Signup and view all the flashcards
Loss of Taste in Bell's Palsy
Loss of Taste in Bell's Palsy
Signup and view all the flashcards
Post-auricular Pain
Post-auricular Pain
Signup and view all the flashcards
Unilateral Facial Drooping
Unilateral Facial Drooping
Signup and view all the flashcards
Bell’s Phenomenon
Bell’s Phenomenon
Signup and view all the flashcards
Reduced Corneal Reflex
Reduced Corneal Reflex
Signup and view all the flashcards
Taste Impairment Test
Taste Impairment Test
Signup and view all the flashcards
Intact Forehead Movement
Intact Forehead Movement
Signup and view all the flashcards
Study Notes
- Bell's palsy is an acute, idiopathic peripheral facial nerve (CN VII) palsy
- Results in unilateral facial weakness or paralysis
- It is the most common cause of facial paralysis
- Symptoms develop abruptly over 48-72 hours
- While often self-limiting, incomplete recovery occurs in about 30% of cases, meaning prompt intervention is needed
- Early treatment with corticosteroids improves outcomes and reduces complications, such as synkinesis
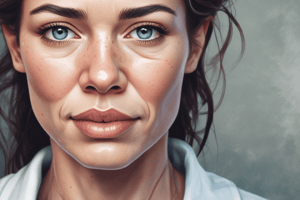
- Bell's palsy causes sudden, temporary weakness in your facial muscles
- This makes half of your face droop
- Your smile becomes one-sided, and your eye on the affected side resists closing
- Can occur at any age
- The exact cause is unknown
- Believed to be the result of swelling and inflammation of the CN VII (facial nerve) that controls the muscles on one side of your face
- In most cases the disease is temporary
- Symptoms improve in a few weeks with complete recovery in 6 months
- A few people have long-term symptoms and rarely it recurs
- The Facial Nerve (CN VII) passes through a narrow corridor of bone on its way to your face.
- Facial weakness or paralysis may cause one corner of your mouth to droop, and you may have trouble retaining saliva on that side of your mouth.
- It may also make it difficult to close the eye on the affected side of your face.
Etiology
- Arises from inflammation and compression of the facial nerve within the bony facial canal
- Likely triggered by viral reactivation (e.g., HSV-1)
- Ischemia from microvascular dysfunction (e.g., diabetes, hypertension) may exacerbate nerve injury
- Autoimmune mechanisms and environmental factors (e.g., pregnancy, cold exposure) may also contribute
- Secondary causes like Lyme disease or tumors must be excluded
- In acute, there is inflammation of the facial nerve with mononuclear cells, consistent with an infectious or immune cause
- Herpes simplex virus (HSV) type 1 DNA was frequently detected in endoneurial fluid and posterior auricular muscle, suggesting reactivation of this virus
- Reactivation of varicella-zoster virus is associated with the disease in up to one-third of cases and may represent the second most frequent cause
- A variety of other viruses have also been implicated less commonly
- can be observed in the setting of human immunodeficiency virus (HIV) seroconversion
Incidence
- Annual incidence: 15-30 cases per 100,000
- 40,000 cases per year in the U.S.
- Higher rates in pregnancy (third trimester) and individuals with diabetes
- Lifetime risk: 1 in 60
Risk Factors
- Diabetes: Microvascular ischemia increases nerve vulnerability
- Pregnancy: Hormonal changes and fluid retention elevate risk
- Hypertension: Linked to poorer recovery and recurrence
- The exact cause remains unknown
- Often related to a Viral illness
Viral Illnesses Common
- Herpes simplex (I and II)
- Herpes zoster
- Epstein-Barr
- Cytomegalovirus
- Adenovirus
- Mumps
- Rubella
- Influenza B
- Coxsackievirus
- Lyme's disease (bacterial)
Prevention
- Manage chronic conditions (diabetes, hypertension)
- Avoid cold exposure and viral triggers
- No specific immunizations, though HSV vaccination research is ongoing
Clinical Manifestations
- Sudden unilateral facial weakness: Inability to close the eye, smile symmetrically, or raise the eyebrow (House-Brackmann Grade II-VI)
- Lagophthalmos: Incomplete eyelid closure causing corneal dryness
- Hyperacusis: Sound sensitivity due to stapedius muscle dysfunction
- Loss of taste: Anterior 2/3 of the tongue (chorda tympani involvement)
- Post-auricular pain: Precedes paralysis in 60% of cases
- Sudden onset of mild weakness to total paralysis on one side of the face
- Drooling
- Postauricular pain - pain around the jaw or in or behind the ear on the affected side
- Headache
- A decrease in taste
- Changes in the production of tears and saliva
- The onset is fairly abrupt, with maximal weakness being attained by 48 hours as a general rule
- Pain behind the ear may precede the paralysis for a day or two
- Taste sensation may be lost unilaterally, and hyperacusis may be present
- In some cases, there is mild cerebrospinal fluid lymphocytosis
- MRI may reveal swelling and uniform enhancement of the geniculate ganglion and facial nerve and, in some cases, entrapment of the swollen nerve in the temporal bone
- Approximately 80% of patients recover within a few weeks or months
- Electromyography may be of some prognostic value: evidence of denervation after 10 days indicates there has been axonal degeneration, that there will be a long delay (3 months as a rule) before regeneration occurs, and that it may be incomplete
- The presence of incomplete paralysis in the first week is the most favorable prognostic sign
- Recurrences are reported in about 7% of cases
Review Of Systems
- Neurological: Facial asymmetry, difficulty blinking, speech changes
- Ophthalmological: Dry eye, excessive tearing
- Otolaryngological: Ear pain, hyperacusis
- Gastrointestinal: Altered taste, drooling
- Dermatological: Flattened nasolabial fold
Physical Assessment Findings
- Unilateral facial drooping: Asymmetric smile and forehead wrinkling
- Bell's phenomenon: Upward eye deviation on attempted closure
- Reduced corneal reflex: Due to orbicularis oculi weakness
- Taste impairment: Tested with sweet/salty substances on anterior tongue
- Intact forehead movement: Differentiates from central causes (e.g., stroke)
Assessment Tools & Grading
- Observe for facial asymmetry including smile, nasolabial folds, blinking
- General Exam including otoscopy, palpation of masses near neck and face, and skin exam
- Assessment of Motor Function -
- Raise eyebrows, close eyes tightly, smile, puff out cheeks, purse lips, grimace (show upper and lower teeth)
- Assess sensory function measuring sensation of the face and ears, taste sensation to the anterior 2/3rd of tongue
- Assess Reflexes - Orbicularis reflex: tap the glabella and observe for asymmetry in blink pattern; Bell Phenomenon: observe upward movement of eyes during forced eye closure
- House-Brackmann Scale: Grades severity from I (normal) to VI (total paralysis)
- Sunnybrook Facial Grading System: Quantifies symmetry and movement
High Yield Questions to Ask Patient
- Did symptoms develop suddenly (≤72 hours)?
- Any recent viral illness, tick exposure, or trauma?
- Pain behind the ear before weakness?
- Difficulty closing one eye or tasting food?
- History of diabetes, hypertension, or pregnancy?
- Prior episodes of facial weakness?
- Recent weight loss, fever, or rash (e.g., Lyme, Ramsay Hunt)?
- Exposure to loud noises worsening symptoms?
- Current medications (e.g., antivirals, steroids)?
- Family history of autoimmune disorders?
Clinical Algorithms
- Acute Evaluation:
- Rule out stroke (forehead sparing? MRI/CT)
- Check for vesicular rash (Ramsay Hunt) or tick exposure (Lyme serology)
- Assess House-Brackmann grade
- Management:
- Start steroids within 72 hours
- Add antivirals if HSV/VZV suspected
- Refer refractory cases to neurology
Treatment Prioritization
- Corticosteroids: Prednisone 60 mg/day × 5 days, then 5-day taper
- Eye protection: Artificial tears, nighttime ointment, patching
- Antivirals: Valacyclovir 1 g TID × 7 days if HSV/VZV suspected
- Physical therapy: Facial exercises to prevent contractures
- Symptomatic measures:
- The use of paper tape to depress the upper eyelid during sleep and prevent corneal drying
- Artificial tears
- Massage of the weakened muscles
- A course of glucocorticoids, given as prednisone 60-80 mg daily during the first 5 days and then tapered over the next 5 days, modestly shortens the recovery period and improves the functional outcome
- Large and well-controlled randomized trials found no added benefit of the antiviral agents valacyclovir (1000 mg daily for 5-7 days) or acyclovir (400 mg five times daily for 10 days) compared to glucocorticoids alone
- Either of these agents should be used if vesicular lesions are observed in the palate or external auditor canal
- For patients with permanent paralysis from the disease, a number of cosmetic surgical procedures have been used to restore a relatively symmetric appearance to the face
Nonpharmacological Management
- Eye care: Lubricating drops hourly, moisture chamber goggles
- Facial massage: Prevents muscle atrophy
- Neuromuscular retraining: Improves symmetry
- Eye protection
- MOST IMPORTANT: Eye patch at night, lubricant eye drops every 2 hours, protective glasses; Physical therapy to restore muscle strength
- Facial Massage – warm moist compresses
- Acupuncture
Pharmacological Management
- 1st Line: Prednisone or prednisolone 60-80 mg PO daily × 5 days, taper by 10mg/day for at least 10 days
- 2nd Line: Valacyclovir 1 g PO TID × 7 days (if HSV/VZV suspected)
- Adjuncts: Artificial tears (carboxymethylcellulose), lubricating ointment (lanolin)
- Steroids (maximum benefit when started within 72 hours - Prednisone or Prednisolone 60-80mg for 5 days with taper by 10mg/ day for a total of at least 10 days
- Antivirals (in conjunction with Steroids)
- Tapered dosage of corticosteroids (must be initiated within 3 days of onset or little benefit)
- Studies are limited for treatment in children younger than 16 years
- Children have higher rates of spontaneous recovery than adults
- Valacyclovir is first line due to superior bioavailability and ease of administration
- Oral antiviral agents plus oral corticosteroids for patients with House-Brackmann grade IV or higher
- Eye Care:
- Artificial tears (liquid or gel): applied every hour while awake
- Ointment with mineral oil and white petrolatum (e.g., Soothe) applied at night
- Aspirin, acetaminophen, ibuprofen for pain relief
- Cautious use of steroids in pregnancy
- Monitor blood pressure for hypertensive disorder
Differentiation
- Guilian-Barré presents with Ascending paralysis and areflexia -- Diagnostic test is Lumbar puncture, EMG
- Lyme Disease presents with Erythema migrans, bilateral palsy -- Diagnostic test is Lyme serology
- Ramsay Hunt Syndrome presents with Vesicular rash, ear pain -- Diagnostic test is VZV PCR
- Stroke presents with Forehead sparing, focal deficits -- Diagnostic test is MRI brain
- Parotid Tumor presents with Progressive weakness, mass on imaging -- Diagnostic test is CT/MRI with contrast
Consultation/Referral
- Neurology: Atypical features or no improvement at 3 weeks
- Ophthalmology: Persistent lagophthalmos/corneal ulceration
- ENT: Surgical decompression if refractory (rare)
- Ophthalmology – eye complications i.e.: corneal abrasion
- Neurology - for CNS involvement or if suspected
- Neurosurgery - decompressive surgery for those with 90% nerve compression
- Otolaryngology – Botox injections if not resolved in 3 months
Initial Diagnosis Patient Guidance
- Reassure 70% recover fully within 6 months
- Eye care: Demonstrate artificial tears and patching
- Medication adherence: Stress steroid taper completion
- Follow-up: Schedule at 1 and 3 weeks
Risk Stratification
- Low risk: House-Brackmann Grade II-III, no comorbidities
- High risk: Grade IV-VI, diabetes, or pregnancy
Follow Up
- 1 week: Assess steroid response, eye integrity
- 1 month: EMG if no improvement
- 3-6 months: Evaluate for synkinesis
Expected Course
- 85% show improvement within 3 weeks
- Full recovery in 70% by 6 months
- 5% of patients will have severe sequalae which can include:
- Facial asymmetry
- Vision loss
- Hearing loss
- Tinnitus
- Poorer prognosis with complete paralysis, age >60, or hypertension
Possible Complications
- Corneal ulceration: From exposure keratopathy
- Synkinesis: Aberrant nerve regeneration causing involuntary movements
- Chronic facial asymmetry: Affects 5-10%
Key Pearls
- "Forehead sparing” suggests central pathology (e.g., stroke)
- Steroids within 72 hours improve recovery by 14%
- House-Brackmann Grade ≥IV predicts incomplete recovery
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.